Implementing Nursing Care
Objectives
• Explain the relationship of implementation to the nursing diagnostic process.
• Describe the association between critical thinking and selecting nursing interventions.
• Discuss the differences between protocols and standing orders.
• Identify preparatory activities to use before implementation.
• Discuss the value of the Nursing Interventions Classification system in documenting nursing care.
• Discuss the steps for revising a plan of care before performing implementation.
• Define the three implementation skills.
• Describe and compare direct and indirect nursing interventions.
Key Terms
Activities of daily living (ADLs), p. 259
Adverse reaction, p. 261
Clinical practice guideline, p. 255
Counseling, p. 260
Direct care, p. 253
Implementation, p. 253
Indirect care, p. 253
Instrumental activities of daily living (IADLs), p. 260
Interdisciplinary care plans, p. 262
Lifesaving measure, p. 260
Nursing intervention, p. 253
Patient adherence, p. 262
Preventive nursing actions, p. 261
Standing order, p. 256
![]()
You first met Tonya and Mr. Jacobs in Chapter 16. The two have collaborated during the nursing process to develop a relevant and appropriate plan of care. During implementation Tonya works with fellow health care colleagues and Mr. and Mrs. Jacobs to provide the safest and most effective nursing interventions for the patient’s health care problems. Implementation is circular, like all steps of the nursing process. This means that, during the course of Mr. Jacobs’ hospitalization, as his clinical condition changes Tonya reassesses the status of existing nursing diagnoses, confirms that these diagnoses are still appropriate, evaluates the patient’s responses to planned interventions (see Chapter 20), and continues to deliver interventions in a timely and competent manner. Critical thinking, which includes good clinical decision making, is important for the successful implementation of nursing interventions.
Implementation, the fourth step of the nursing process, formally begins after the nurse develops a plan of care. With a care plan based on clear and relevant nursing diagnoses, the nurse initiates interventions that are designed to achieve the goals and expected outcomes needed to support or improve the patient’s health status. A nursing intervention is any treatment based on clinical judgment and knowledge that a nurse performs to enhance patient outcomes (Bulechek et al., 2008). Ideally the interventions a nurse uses are evidenced based (see Chapter 5), providing the most current, up-to-date, and effective approaches for managing patient problems. Interventions include direct and indirect care measures aimed at individuals, families, and/or the community.
Direct care interventions are treatments performed through interactions with patients (Bulechek et al., 2008). For example, a patient receives direct intervention in the form of medication administration, insertion of an intravenous (IV) infusion, or counseling during a time of grief. Indirect care interventions are treatments performed away from the patient but on behalf of the patient or group of patients (Bulechek et al., 2008). For example, indirect care measures include actions for managing the patient’s environment (e.g., safety and infection control), documentation, and interdisciplinary collaboration. Both direct and indirect care measures fall under the intervention categories described in Chapter 18: nurse-initiated, physician-initiated, and collaborative. For example, the direct intervention of patient education is a nurse-initiated intervention. The indirect intervention of consultation is a collaborative intervention.
Benner (1984) defined the domains of nursing practice, which help to explain the nature and intent of the many ways nurses intervene for patients (Box 19-1). These domains are current today. The extent of organizational and work role competencies has become more complex; thus it is important that the focus of implementation always be the patient. Nursing is an art and a science. It is not simply a task-based profession. Thus you learn to intervene for a patient within the context of his or her unique situation. Examples of factors to consider during intervention follow. Who is the patient? What does this illness mean to the patient and his or her family? What clinical situation requires you to intervene? How does the patient perceive the interventions that you will deliver? Will any cultural considerations influence your approach? In what way do you best support or show caring as you intervene? The answers to these questions enable you to deliver care compassionately and effectively with the best outcomes for your patients.
Critical Thinking in Implementation
The delivery of nursing interventions is a complex decision-making process that involves critical thinking. The context in which you deliver care to each patient and the many interventions required result in decision-making approaches for each clinical situation. Critical thinking is necessary to consider the complexity of interventions, including the number of alternative approaches and the amount of time available to act.
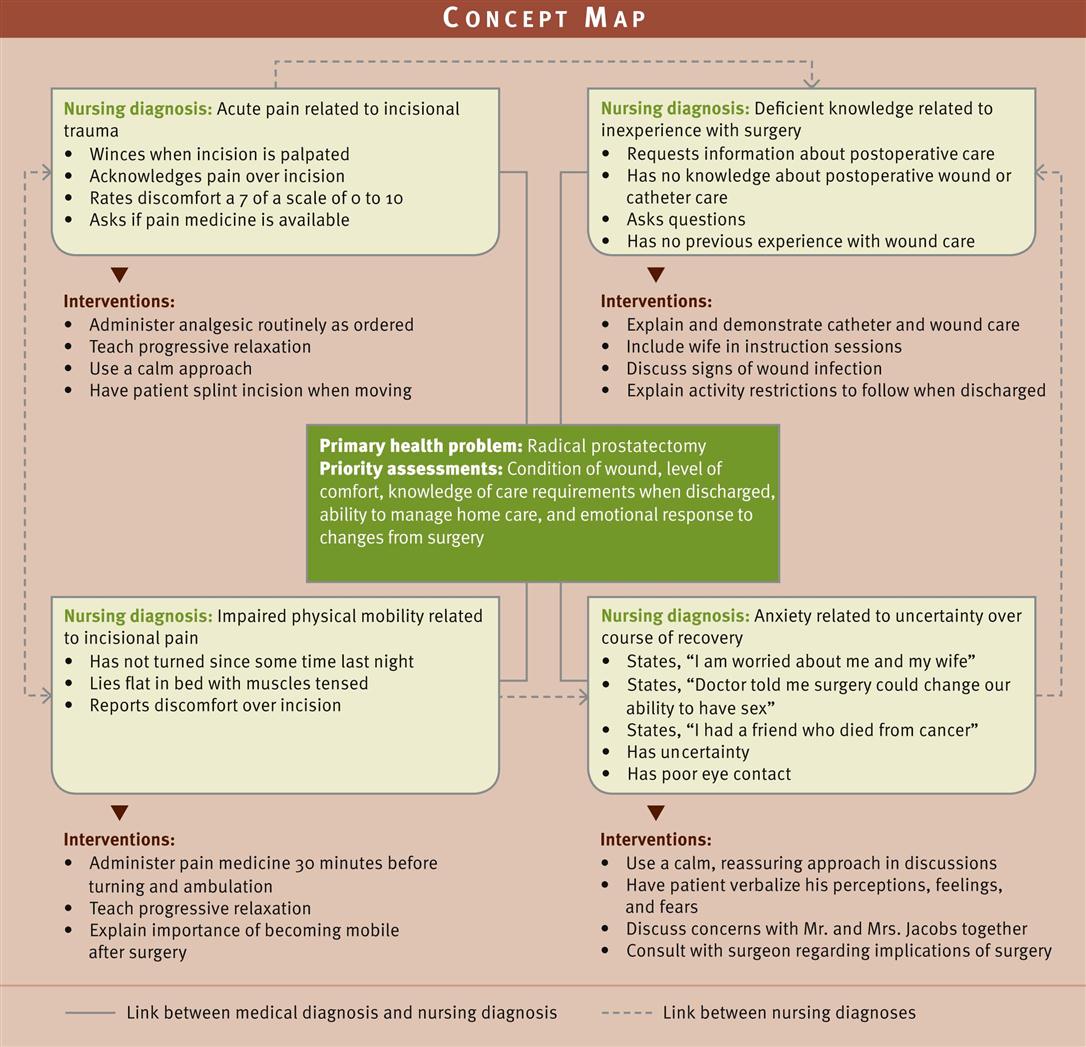
Tonya indentified four relevant nursing diagnoses for Mr. Jacobs: acute pain related to incisional trauma, deficient knowledge regarding postoperative recovery related to inexperience with surgery, impaired physical mobility related to incisional pain, and anxiety related to uncertainty over the course of recovery. The diagnoses are interrelated, and sometimes a planned intervention (e.g., administering pain medication) treats or modifies more than one of the patient’s health problems (pain and impaired physical mobility). Tonya applies critical thinking and uses her time with Mr. Jacobs wisely by anticipating his priorities, applying the knowledge she has about his problems and the interventions planned, and implementing care strategies skillfully.
Before implementing a planned intervention, use critical thinking to confirm whether the intervention is correct and still appropriate for the patient’s clinical situation. Even though you have planned a set of interventions for a patient, you have to exercise good judgment and decision making before actually delivering each intervention. Always think before you act. Patients’ conditions often change minute to minute. You need to consider the scheduling of activities on a nursing unit, which often dictates when and how to complete an intervention. Thus many factors influence your decision on how and when to intervene. You are responsible for having the necessary knowledge and clinical competency to perform interventions for your patients safely and effectively. Some tips for making decisions during implementation follow.
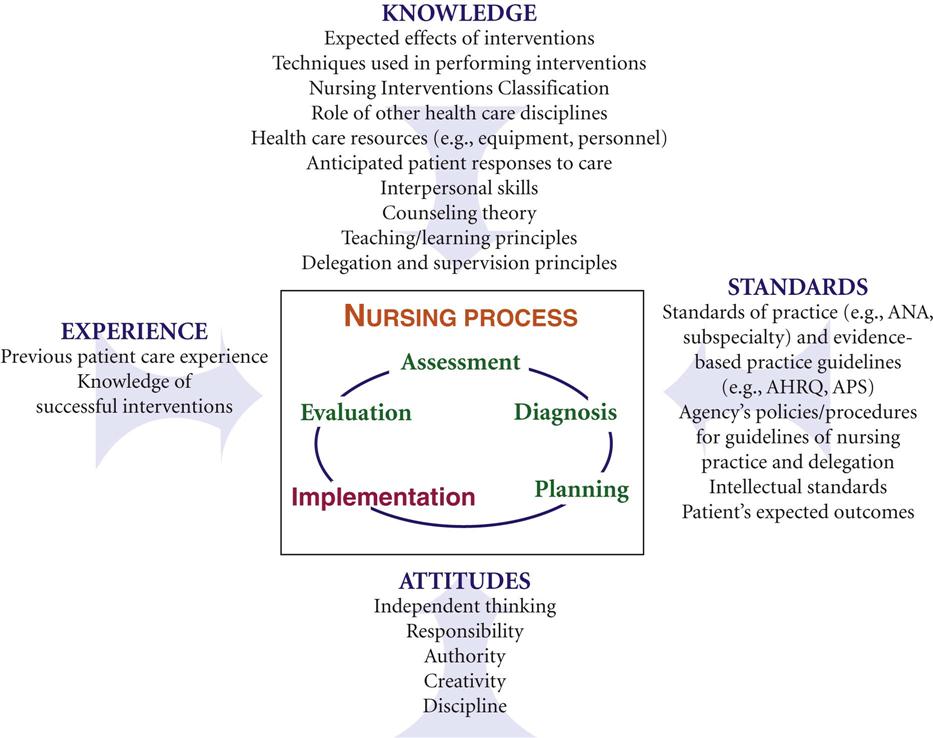
The selection and performance of nursing interventions for a patient are part of clinical decision making. The critical thinking model described in Chapter 15 provides a framework for how to make decisions when implementing nursing care (Fig. 19-1). You learn how to implement nursing care using appropriate knowledge. For example, as you proceed with an intervention, you consider what you know about the purpose of the intervention, the steps in performing the intervention correctly, the medical condition of the patient, and his or her expected response. It is important to prepare well before first caring for any patient. With experience you become more proficient in anticipating what to expect in a given clinical situation and how to modify your approach. As you gain clinical experience, you are able to consider which interventions worked previously, which have not, and why. It also helps to know the clinical standards of practice for your agency. For example, one hospital has a different set of standards for patient education than another. The standards of practice offer guidelines for selection of interventions and their frequency and whether you are able to delegate the procedures.
As you perform a nursing intervention, apply intellectual standards, which are the guidelines for rational thought and responsible action. For example, before Tonya begins to teach Mr. Jacobs, she considers how to make her instructions relevant, clear, logical, and complete to promote patient learning. She knows that it will be helpful to involve Mrs. Jacobs so any instruction is relevant to their home situation. Using simple, clear explanations and repeated instructions promote learning for Mr. Jacobs, who is inexperienced with postoperative recovery. Making an instructional DVD on wound care available to the family is a valuable resource for repeated viewing in the home.
As a critical thinker, apply critical thinking attitudes when you intervene. For example, show confidence in performing an intervention. When you are unsure of how to perform a procedure, be responsible in seeking assistance from others. Confidence in performing interventions builds trust with patients. Creativity and self-discipline are attitudes that guide you in reviewing, modifying, and implementing interventions. As a beginning nursing student, seek out supervision from instructors or experienced nurses to guide you in the decision-making process for implementation.
Standard Nursing Interventions
Health care settings present various ways for nurses to create and individualize a patient’s plan of care. Each plan of care is totally unique to that patient, with interventions individualized on the basis of his or her specific health problems. In certain situations a nurse develops the plan on the basis of personal knowledge and clinical experience. However, systems are available that provide standardized interventions for nurses to use in their plan of care. Many patients have common health care problems; thus standardized interventions for these health problems make it quicker and easier for nurses to intervene. More important, if the standards are evidence based, the nurse is more likely to deliver the most clinically effective interventions to improve patient outcomes (see Chapter 5). Standardized interventions most often set a level of clinical excellence for practice. Nurse- and physician-initiated standardized interventions are available in the form of clinical guidelines or protocols, preprinted (standing) orders, and Nursing Interventions Classification (NIC) interventions. At a professional level the American Nurses Association (ANA) defines standards of professional nursing practice, which include standards for the implementation step of the nursing process. These standards are authoritative statements of the duties that all registered nurses are expected to perform competently, regardless of role, patient population they serve, or specialty (ANA, 2010) (see Chapter 1).
Clinical Practice Guidelines and Protocols
A clinical practice guideline or protocol is a systematically developed set of statements that helps nurses, physicians, and other health care providers make decisions about appropriate health care for specific clinical situations (Manchikanti et al., 2010). A guideline guides interventions for specific health care problems or conditions such as low back pain, dizziness, or deep vein thrombosis. The guideline is developed on the basis of an authoritative examination of current scientific evidence (National Guideline Clearinghouse [NGC], 2010). Guidelines are now seen as key tools for improving the quality of health care and bridging the gap between the growth of research findings and actual clinical practice (Rosenbrand et al., 2008).
Clinicians within a health care agency sometimes choose to review the scientific literature and their own standard of practice to develop guidelines and protocols in an effort to improve their standard of care. For example, a hospital develops a rapid-assessment protocol to improve the identification and early treatment of patients suspected of having a stroke. However, clinical practice guidelines have already been developed by national health groups such as the National Institutes of Health and the National Guideline Clearinghouse. These guidelines are readily available to any clinician or health care institution that wishes to adopt evidence-based guidelines in the care of patients with specific health problems. One valuable source for nursing practice guidelines is the Gerontological Nursing Interventions Research Center (GNIRC) at the University of Iowa. The center has numerous clinical guidelines, including ones for acute confusion and delirium, acute pain management, and fall prevention for older adults (GNIRC, 2010).
Advanced practice nurses who provide primary care for patients in outpatient settings frequently follow diagnostic and treatment protocols. In such a setting nurses assess the patient and identify abnormalities. The protocol outlines the conditions that nurses are permitted to treat such as controlled hypertension and the types of treatment that they are permitted to administer such as antihypertensive medications. In acute care settings it is common to find clinical protocols that outline independent nursing interventions for specific conditions. Examples include protocols for admission and discharge, pressure ulcer care, and incontinence management. Protocols are also used in interdisciplinary settings for diagnostic testing and physical, occupational, and speech therapies.
Standing Orders
A standing order is a preprinted document containing orders for the conduct of routine therapies, monitoring guidelines, and/or diagnostic procedures for specific patients with identified clinical problems. A standing order directs the conduct of patient care in a specific clinical setting. Licensed prescribing health care providers in charge of care at the time of implementation approve and sign standing orders. These orders are common in critical care settings and other specialized practice settings where patients’ needs change rapidly and require immediate attention. An example of such a standing order is one specifying certain medications such as lidocaine or propranolol for an irregular heart rhythm. After assessing the patient and identifying the irregular rhythm, the critical care nurse gives the specified medication without first notifying the physician. The physician’s initial standing order covers the nurse’s action. After completing a standing order, the nurse notifies the physician. Standing orders are common in the community health setting, where the nurse faces situations that do not permit immediate contact with a health care provider. Standing orders give the nurse legal protection to intervene appropriately in the patient’s best interest.
NIC Interventions
The NIC system developed by the University of Iowa helps to differentiate nursing practice from that of other health care professionals (Box 19-2). The NIC interventions offer a level of standardization to enhance communication of nursing care across settings and to compare outcomes. By using NIC nurses learn the common interventions recommended for various NANDA International nursing diagnoses. Nurses also learn the numerous care activities for each NIC intervention. Recently the NIC interventions have been used for work complexity assessment, a process that helps nurses identify interventions performed on a routine basis for their patient populations (Scherb and Weydt, 2009). Chapter 18 describes the NIC system in more detail.
Standards of Practice
The ANA Standards of Professional Nursing Practice (ANA, 2010) are to be used as evidence of the standard of care that registered nurses provide their patients (see Chapter 1). The standards are formally reviewed on a regular basis. The newest standards include competencies for establishing professional and caring relationships, using evidence-based interventions and technologies, providing holistic care across the life span to diverse groups, and using community resources and systems. In addition, the standards emphasize implementing a timely plan following patient safety goals (ANA, 2010).
Implementation Process
Preparation for implementation ensures efficient, safe, and effective nursing care. Five preparatory activities include reassessing the patient, reviewing and revising the existing nursing care plan, organizing resources and care delivery, anticipating and preventing complications, and implementing nursing interventions.
Tonya returns to Mr. Jacobs’ room 30 minutes after administering a dose of IV morphine for his incisional pain. She notices that he is more relaxed and turning a bit on his own. She asks him to rate his pain on a scale of 0 to 10, and he responds that it is now a 3. With the pain currently under control, Tonya decides to get the patient up in a chair to begin increasing his activity level. While Mr. Jacobs is in the chair, Tonya gets the teaching booklets she wants to use to prepare the patient for wound and catheter care in the home. She knows that Mrs. Jacobs is due to arrive at any time; thus she plans to include her in the discussion. Tonya also knows that this is Mr. Jacobs’ first time up in the chair; thus she anticipates monitoring him closely and judging if he is alert and comfortable enough to begin the planned instruction.
Reassessing the Patient
Assessment is a continuous process that occurs each time you interact with a patient. When you collect new data about a patient, you sometimes identify a new nursing diagnosis or determine the need to modify the care plan. During the initial phase of implementation reassess the patient. The reassessment often focuses on one primary nursing diagnosis, or one dimension of the patient such as level of comfort, or one system such as the cardiovascular system. The reassessment helps you decide if the proposed nursing actions are still appropriate for the patient’s level of wellness. Reassessment is not the evaluation of care (see Chapter 20), but it is the gathering of additional information to ensure that the plan of care is appropriate. For example, Tonya plans to talk with Mr. Jacobs about surgery and what to expect during recovery. However, she learns from Mr. Jacobs that Mrs. Jacobs’ visit has been delayed until lunchtime. She knows that Mrs. Jacobs is an important resource for Mr. Jacobs’ recovery, but she decides to get Mr. Jacobs up in a chair and focus on how he tolerates the activity anyway. Pain control is still a priority. Tonya will help Mr. Jacobs back to bed after about 30 minutes, allow him to rest until lunchtime, and then begin her instruction.
Reviewing and Revising the Existing Nursing Care Plan
After reassessing a patient, review the care plan and compare assessment data to validate the nursing diagnoses and determine whether the nursing interventions remain the most appropriate for the clinical situation. If the patient’s status has changed and the nursing diagnosis and related nursing interventions are no longer appropriate, modify the nursing care plan. An out-of-date or incorrect care plan compromises the quality of nursing care. Review and modification enable you to provide timely nursing interventions to best meet the patient’s needs.
After reviewing the care plan, Tonya made a few revisions to Mr. Jacobs’ concept map (Fig. 19-2). Tonya notices that eye contact with Mr. Jacobs has improved; trust is building. Mr. Jacobs’ pain has also lessened. She modifies her plan for reducing anxiety by planning a discussion with Mr. and Mrs. Jacobs together and consulting with the surgeon.
Modification of an existing written care plan includes four steps:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree