Hygiene
Objectives
• Describe factors that influence personal hygiene practices.
• Discuss the role that critical thinking plays in providing hygiene.
• Conduct a comprehensive assessment of a patient’s total hygiene needs.
• Discuss conditions that place patients at risk for impaired skin integrity.
• Discuss factors that influence the condition of the nails and feet.
• Explain the importance of foot care for the patient with diabetes.
• Discuss conditions that place patients at risk for impaired oral mucous membranes.
• List common hair and scalp problems and their related interventions.
• Describe how hygiene care for the older adult differs from that for the younger patient.
• Discuss different approaches used in maintaining a patient’s comfort and safety during hygiene care.
• Adapt hygiene care for a patient who is cognitively impaired.
Key Terms
Acne, p. 771
Alopecia, p. 776
Caries, p. 772
Cerumen, p. 776
Complete bed bath, p. 783
Cuticle, p. 769
Dental caries, p. 770
Edentulous, p. 772
Effleurage, p. 785
Enucleation, p. 790
Epidermis, p. 769
Gingivitis, p. 770
Glossitis, p. 775
Halitosis, p. 775
Mucositis, p. 779
Partial bed bath, p. 783
Pediculosis capitis, p. 776
Perineal care, p. 784
Stomatitis, p. 786
Xerostomia, p. 770
![]()
Personal hygiene affects patients’ comfort, safety, and well-being. Hygiene care includes cleaning and grooming activities that maintain personal body cleanliness and appearance. Personal hygiene activities such as taking a bath or shower, brushing and flossing the teeth, washing and grooming the hair, and performing nail care promote comfort and relaxation, foster a positive self-image, promote healthy skin, and help prevent infection and disease. Healthy people fulfill their own hygiene needs; but when ill or physically or emotionally challenged, people often require some degree of assistance with hygiene care. A variety of personal, social, and cultural factors influence hygiene practices.
In both agency and home care settings, determine a patient’s ability to perform self-care and provide hygiene care according to individual needs and preferences. In addition, in the home setting help the patient and family adapt hygiene techniques and approaches. Use the close contact required for hygiene care to promote a caring therapeutic relationship and provide needed patient teaching and counseling. Integrate other nursing activities during hygiene care, including assessment and interventions such as range-of-motion (ROM) exercises, application of dressings, or inspection and care of intravenous (IV) sites. During hygiene care preserve as much of the patient’s independence as possible, assess his or her ability to perform hygiene care, ensure privacy, convey respect, and foster his or her physical comfort.
Scientific Knowledge Base
Proper hygiene care requires an understanding of the anatomy and physiology of the skin, nails, oral cavity, eyes, ears, and nose. The skin and mucosal cells exchange oxygen, nutrients, and fluids with underlying blood vessels. The cells require adequate nutrition, hydration, and circulation to resist injury and disease. Good hygiene techniques promote the normal structure and function of these tissues.
Apply knowledge of pathophysiology to provide preventive hygiene care. Recognize disease states that create changes in the integument, oral cavity, and sensory organs. For example, diabetes mellitus often results in chronic vascular changes that impair healing of the skin and mucosa. In the early stages of acquired immunodeficiency syndrome (AIDS), fungal infections of the oral cavity are common. Paralysis of the trigeminal nerve (cranial nerve V) eliminates the blink reflex, causing risk of corneal drying. In the presence of conditions such as these, adapt hygiene practices to minimize injury. Use time spent providing hygiene care to identify abnormalities and initiate appropriate actions to prevent further injury to sensitive tissues.
The Skin
The skin serves several functions, including protection, secretion, excretion, body temperature regulation, and cutaneous sensation (Table 39-1). It consists of two primary layers: the epidermis and the dermis. Just beneath the skin lies the subcutaneous tissue (also known as the hypodermis), which shares some of the protective functions of the skin.
TABLE 39-1
Function of the Skin and Implications for Care
| FUNCTION/DESCRIPTION | IMPLICATIONS FOR CARE |
| Protection | |
| Epidermis is relatively impermeable layer that prevents entrance of microorganisms. Although microorganisms reside on skin surface and in hair follicles, relative dryness of surface of skin inhibits bacterial growth. Sebum removes bacteria from hair follicles. Acidic pH of skin further retards bacterial growth. | Weakening of epidermis occurs by scraping or stripping its surface (e.g., use of dry razors, tape removal, improper turning or positioning techniques). Excessive dryness causes cracks and breaks in skin and mucosa that allow bacteria to enter. Emollients soften skin and prevent moisture loss, soaking skin improves moisture retention, and hydrating mucosa prevents dryness. However, constant exposure of skin to moisture causes maceration or softening, interrupting dermal integrity and promoting ulcer formation and bacterial growth. Keep bed linen and clothing dry. Misuse of soap, detergents, cosmetics, deodorant, and depilatories cause chemical irritation. Alkaline soaps neutralize the protective acid condition of skin. Cleaning skin removes excess oil, sweat, dead skin cells, and dirt, which promote bacterial growth. |
| Sensation | |
| Skin contains sensory organs for touch, pain, heat, cold, and pressure. | Minimize friction to avoid loss of stratum corneum, which results in development of pressure ulcers. Smoothing linen removes sources of mechanical irritation. Remove rings from fingers to prevent accidentally injuring patient’s skin. Make sure that bath water is not excessively hot or cold. |
| Temperature Regulation | |
| Radiation, evaporation, conduction, and convection control body temperature. | Factors that interfere with heat loss alter temperature control. Wet bed linen or gowns interfere with convection and conduction. Excess blankets or bed coverings interfere with heat loss through radiation and conduction. Coverings promote heat conservation. |
| Excretion and Secretion | |
| Sweat promotes heat loss by evaporation. Sebum lubricates skin and hair. | Perspiration and oil harbor microorganisms. Bathing removes excess body secretions; although, if excessive, it causes dry skin. |
Several thin layers of epithelial cells comprise the outer layer, or epidermis; these cells shield underlying tissue against water loss and injury and prevent entry of disease-producing microorganisms. The innermost layer of the epidermis generates new cells to replace the dead cells that the outer surface of the skin continuously sheds. Bacteria commonly reside on the outer epidermis. These resident bacteria are normal flora (see Chapter 28) that do not cause disease but instead inhibit the multiplication of disease-causing microorganisms.
Bundles of collagen and elastic fibers form the thicker dermis that underlies and supports the epidermis. Nerve fibers, blood vessels, sweat glands, sebaceous glands, and hair follicles run through the dermal layers. Sebaceous glands secrete sebum, an oily, odorous fluid, into the hair follicles. Sebum softens and lubricates the skin and slows water loss from the skin when the humidity is low. More important, sebum has bactericidal action.
The subcutaneous tissue layer contains blood vessels, nerves, lymph, and loose connective tissue filled with fat cells. The fatty tissue functions as a heat insulator for the body. Subcutaneous tissue also supports upper skin layers to withstand stresses and pressure without injury and anchors the skin loosely to underlying structures such as muscle. Very little subcutaneous tissue underlies the oral mucosa.
The skin often reflects a change in physical condition by alterations in color, thickness, texture, turgor, temperature, and hydration (see Chapter 30). As long as the skin remains intact and healthy, its physiological function remains optimal. Hygiene practices frequently influence skin status and can have both beneficial and negative effects on the skin. For example, too-frequent bathing and use of hot water frequently leads to dry, flaky skin and loss of protective oils.
The Feet, Hands, and Nails
The feet, hands, and nails often require special attention to prevent infection, odor, and injury. The condition of a patient’s hands and feet influences the ability to perform hygiene care. Without the ability to bear weight, ambulate, or manipulate the hands, the patient is at risk for losing self-care ability.
A wide range of dexterity exists in the hand because of the movement between the thumb and fingers. Any condition that interferes with movement of the hand (e.g., superficial or deep pain or joint inflammation) impairs a patient’s self-care abilities. Foot pain often changes the patient’s gait, causing strain on different joints and muscle groups. Discomfort while standing or walking limits self-care abilities.
The nails grow from the root of the nail bed, which is located in the skin at the nail groove, hidden by the fold of skin called the cuticle. A scalelike modification of the epidermis forms the visible part of the nail (nail body), which has a crescent-shaped white area known as the lunula. Under the nail lies a layer of epithelium called the nail bed. A normal healthy nail appears transparent, smooth, and convex, with a pink nail bed and translucent white tip. Disease causes changes in the shape, thickness, and curvature of the nail (see Chapter 30).
The Oral Cavity
The oral cavity consists of the lips surrounding the opening of the mouth, the cheeks running along the sidewalls of the cavity, the tongue and its muscles, and the hard and soft palate. The mucous membrane, continuous with the skin, lines the oral cavity. The floor of the mouth and the undersurface of the tongue are richly supplied with blood vessels. Normal oral mucosa glistens and is pink, soft, moist, smooth, and without lesions. Ulcerations or trauma frequently result in significant bleeding. Several glands within and outside the oral cavity secrete saliva. Saliva cleanses the mouth, dissolves food chemicals to promote taste, moistens food to facilitate bolus formation, and contains enzymes that start breakdown of starchy foods. The effects of medications, exposure to radiation, dehydration, and mouth breathing impair salivary secretion in the mouth. Strong sympathetic nervous system stimulation almost completely inhibits the release of saliva and results in xerostomia or dry mouth.
The teeth lie in sockets in the gum-covered mandible and maxilla; they tear and grind ingested food so it can be mixed with saliva and swallowed for digestion. A normal tooth consists of the crown, neck, and root. The enamel-covered crown extends above the gingiva or gum, which normally surrounds the tooth like a tight collar. A constricted portion of the tooth called the neck connects the crown and the root; the root is embedded in the jawbone. The periodontal membrane lies just below the gum margins, surrounds a tooth, and holds it firmly in place. Healthy teeth appear white, smooth, shiny, and properly aligned.
Difficulty in chewing develops when surrounding gum tissues become inflamed or infected or when teeth are lost or become loosened. Regular oral hygiene helps to prevent gingivitis (i.e., inflammation of the gums) and dental caries (i.e., tooth decay produced by interaction of food with bacteria).
The Hair
Hair growth, distribution, and pattern indicate a person’s general health status. Hormonal changes, nutrition, emotional and physical stress, aging, infection, and some illnesses affect hair characteristics. The hair shaft itself is lifeless, and physiological factors do not directly affect it. However, hormonal and nutrient deficiencies of the hair follicle cause changes in hair color or condition.
The Eyes, Ears, and Nose
When providing hygiene care, the eyes, ears, and nose require careful attention. Chapter 30 describes the structure and function of these organs. Clean the sensitive sensory tissues in a way that prevents injury and discomfort for a patient, such as using care not to get soap in his or her eyes. In addition, the time you spend with your patient during hygiene provides an excellent opportunity to ask if there are any changes in vision, hearing, or sense of smell.
Nursing Knowledge Base
A number of factors influence personal preferences for hygiene and the ability to maintain hygiene practices. Since no two individuals perform hygiene care in the same manner, you individualize patient care based on learning about his or her unique hygiene practices and preferences. Individualized hygiene care requires use of therapeutic communication skills to promote the therapeutic relationship. In addition, use the opportunity provided during hygiene care to assess a patient’s health promotion practices, emotional status, and health care education needs. Be aware that developmental changes influence the need and preferences for type of hygiene care.
Factors Influencing Hygiene
Social Practices
Social groups influence hygiene preferences and practices, including the type of hygiene products used and the nature and frequency of personal care practices. Parents and caregivers perform hygiene care for infants and young children. Family customs play a major role during childhood in determining hygiene practices such as the frequency of bathing, the time of day bathing is performed, and even whether certain hygiene practices such as brushing of the teeth or flossing are performed. As children enter adolescence, peer groups and media often influence hygiene practices. For example, some young girls become more interested in their personal appearance and begin to wear makeup. During the adult years involvement with friends and work groups shape the expectations that people have about personal appearance. Some older adults’ hygiene practices change because of changes in living conditions and available resources.
Personal Preferences
Patients have individual desires and preferences about when to perform hygiene and grooming care. Some patients prefer to shower, whereas others prefer to bathe. Patients select different hygiene and grooming products according to personal preferences. Knowing patients’ personal preferences promotes individualized care. Help the patient develop new hygiene practices when indicated by an illness or condition. For example, you need to teach a patient with diabetes proper foot hygiene. Safe and effective patient-centered nursing care elicits individual preferences, allows patients to make personal choices whenever possible, and promotes patient involvement and independence (Cronenwett et al., 2007).
Body Image
Body image is a person’s subjective concept of his or her body, including physical appearance, structure, or function (see Chapter 33). Body image affects the way in which individuals maintain personal hygiene. If a patient maintains a neatly groomed appearance, be sure to consider the details of grooming when planning care and consult with the patient before making decisions about how to provide hygiene care. Patients who appear unkempt or uninterested in hygiene sometimes need education about its importance or further assessment regarding their ability to participate with daily hygiene.
Surgery, illness, or a change in emotional or functional status often affects a patient’s body image. Discomfort and pain, emotional stress, or fatigue diminish the ability or desire to perform hygiene self-care and require extra effort to promote hygiene and grooming.
Socioeconomic Status
A person’s economic resources influence the type and extent of hygiene practices used. Be sensitive in considering that the patient’s economic status influences the ability to regularly maintain hygiene. He or she may not be able to afford desired basic supplies such as deodorant, shampoo, and toothpaste. A patient may need to modify the home environment by adding safety devices such as nonskid surfaces and grab bars in the bath to perform hygiene self-care safely. When he or she lacks socioeconomic resources, it becomes difficult to participate and take a responsible role in health promotion activities such as basic hygiene.
Health Beliefs and Motivation
Knowledge about the importance of hygiene and its implications for well-being influences hygiene practices. However, knowledge alone is not enough. Motivation also plays a key role in a patient’s hygiene practices. Patient teaching is often needed to foster hygiene self-care. Provide information that focuses on a patient’s health-related issues relevant to the desired hygiene care behaviors. Patient perceptions of the benefits of hygiene care and the susceptibility to and seriousness of developing a problem affect the motivation to change behavior (Pender, Murdaugh, and Parsons, 2011). For example, do patients perceive that they are at risk for dental disease, that dental disease is serious, and that brushing and flossing are effective in reducing risk? When they recognize that there is a risk and that they can take reasonable action without negative consequences, they are more likely to be receptive to nurses’ counseling and teaching efforts.
Cultural Variables
Cultural beliefs and personal values influence hygiene care (Box 39-1). People from diverse cultural backgrounds frequently follow different self-care practices (see Chapter 9). Maintaining cleanliness does not hold the same importance for some ethnic or social groups as it does for others (Galanti, 2008). In North America it is common to bathe or shower daily and use deodorant to prevent body odors. However, people from some cultures are not sensitive to body odors, prefer to bathe less frequently, and do not use deodorant. Some homeless people believe that a layer of dirt helps protect them from becoming sick (Galanti, 2008). Do not express disapproval when caring for patients whose hygiene practices differ from yours. Avoid forcing changes in hygiene practices unless the practices affect the patient’s health. In these situations use tact, provide information, and allow choices. Religious beliefs associated with culture sometimes influence hygiene practices. Facilitate a patient’s religious practices whenever possible. For example, Muslim patients often remove their shoes and assume different positions for prayer. This increases the risk of developing foot pathology such as calluses on the toes and lateral ankles. When caring for Muslim patients who have diabetes mellitus, you need to be supportive of religious practices while also stressing the need to be diligent in inspecting the feet after prayer sessions for any blisters or calluses.
Developmental Stage
The normal process of aging influences the condition of body tissues and structures. A patient’s developmental stage affects the ability of the patient to perform hygiene care and the type of care needed. Apply knowledge of developmental changes as you assess your patients and plan, implement, and evaluate hygiene care.
Skin
The neonate’s skin is relatively immature at birth. The epidermis and dermis are loosely bound together, and the skin is very thin. Friction against the skin layers causes bruising. Handle the neonate carefully during bathing. Any break in the skin easily results in an infection.
A toddler’s skin layers become more tightly bound together. Thus the child has a greater resistance to infection and skin irritation. However, because of his or her more active play and the absence of established hygiene habits, parents and caregivers need to provide thorough hygiene and teach good hygiene habits.
During adolescence the growth and maturation of the integument increases. In girls estrogen secretion causes the skin to become soft, smooth, and thicker with increased vascularity. In boys male hormones produce an increased thickness of the skin with some darkening in color. Sebaceous glands become more active, predisposing adolescents to acne (i.e., active inflammation of the sebaceous glands accompanied by pimples). Sweat glands become fully functional during puberty. Adolescents usually begin to use antiperspirants. More frequent bathing and shampooing also become necessary to reduce body odors and eliminate oily hair.
The condition of the adult’s skin depends on hygiene practices and exposure to environmental irritants. Normally the skin is elastic, well hydrated, firm, and smooth. When an adult bathes frequently or is exposed to an environment with low humidity, it becomes dry and flaky. With aging the rate of epidermal cell replacement slows, and the skin thins and loses resiliency. Moisture leaves the skin, increasing the risk for bruising and other types of injury. As the production of lubricating substances from skin glands decreases, the skin becomes dry and itchy (Meiner, 2011). These changes warrant caution when turning and repositioning older adults and when bathing. Too-frequent bathing and bathing with hot water or harsh soap cause the skin to become excessively dry (American Academy of Dermatology, 2009).
Feet and Nails
With aging and continued exposure the patient is more likely to develop chronic foot problems as a result of poor foot care, improper fit of footwear, and systemic disease. Older adults do not always have the strength, flexibility, visual acuity, or manual dexterity to care for their feet and nails. Long or roughened nails lead to traumatic nail avulsions in which the nail plate is torn from the nail bed (Berridge, 2009).
Older adults often have dry feet because of a decrease in sebaceous gland secretion and dehydration of epidermal cells. Common problems of the feet affecting older adults include corns, calluses, bunions, hammertoe, and fungal infections (Wright, 2009). Older adults frequently complain of foot pain (Meiner, 2011). Painful feet result from a variety of congenital deformities, weak structure, injuries, and diseases such as diabetes and rheumatoid arthritis.
The Mouth
At approximately 6 to 8 months of age, infants begin teething. The first permanent (secondary) teeth erupt at about 6 years of age (Hockenberry and Wilson, 2011). From adolescence, when all of the permanent teeth are in place, through middle adulthood, the teeth and gums remain healthy if a person follows healthy eating patterns and dental care. Avoiding fermentable carbohydrates and sticky sweets helps to keep the teeth free of caries. In addition, regular brushing and flossing help to prevent caries and periodontal disease.
As a person ages, numerous factors result in poor oral health. These include age-related changes of the mouth, chronic disease such as diabetes, physical disabilities involving hand grasp or strength affecting the ability to perform oral care, lack of attention to oral care, and prescribed medications that have oral side effects. Gums lose vascularity and tissue elasticity, which causes dentures to fit poorly. If the older adult becomes edentulous (i.e., without teeth) and wears complete or partial dentures, include assessment of underlying gums and palate.
Hair
Throughout life changes in the growth, distribution, and condition of the hair influence hair hygiene. As males reach adolescence, shaving becomes a part of routine grooming. Young girls who reach puberty often begin to shave their legs and axillae. With aging, as scalp hair becomes thinner and drier, shampooing is usually performed less frequently.
Eyes, Ears, and Nose
Chapter 49 addresses changes in hearing, vision, and olfaction across the life span as a result of growth and development. Alterations in sensory function often require modifications in hygiene care. Use your knowledge of developmental changes when planning hygienic care.
Physical Condition
Patients with certain types of physical limitations or disabilities associated with disease and injury lack the physical energy and dexterity to perform hygiene self-care safely. A patient whose arm is in a cast or who has an IV line needs help with hygiene care. A weakened grasp resulting from arthritis, stroke, or muscular disorders makes using a toothbrush, washcloth, or hairbrush difficult or ineffective. Sensory deficits not only alter a patient’s ability to perform care but also place the patient at risk for injury. Safety is a priority for a patient with a sensory deficit. For example, the inability to feel that the water is too hot can lead to a burn injury during bathing.
Chronic illnesses such as cardiac disease, cancer, neurological disorders, and some mental health illnesses often exhaust or incapacitate patients. Patients who become fatigued frequently need to have complete hygiene care provided. Include periods of rest during care to allow patients who are fatigued the opportunity to participate in their care. Pain often accompanies illness and injury, limiting a patient’s ability to tolerate hygiene and grooming activities or perform self-care. Pain frequently limits ROM, resulting in impaired use of the arms or hands or limited ability to move about in the environment, impairing the ability to perform hygiene self-care. Sedation and drowsiness associated with analgesics used for pain management also limit a patient’s ability to safely participate in care.
Limited mobility caused by a variety of factors (e.g., physical injury, weakness, surgery, pain, prolonged inactivity, medication effect, and presence of indwelling catheter or IV line) decreases a patient’s ability to perform hygiene self-care activities safely. Individualized care considers a patient’s ability to perform care, the amount of assistance needed, and the need for assistive and safety devices to facilitate safe hygiene care.
Acute and chronic cognitive impairments such as stroke, brain injury, psychoses, and dementia often result in the inability to perform self-care independently. When people with cognitive impairments are unaware of their hygiene and grooming needs, they become fearful and agitated during hygiene care, resulting in aggressive behavior (Hoeffer et al., 2006). Safe, effective patient care takes the effect of cognitive impairment on hygiene care into consideration and allows for appropriate modifications.
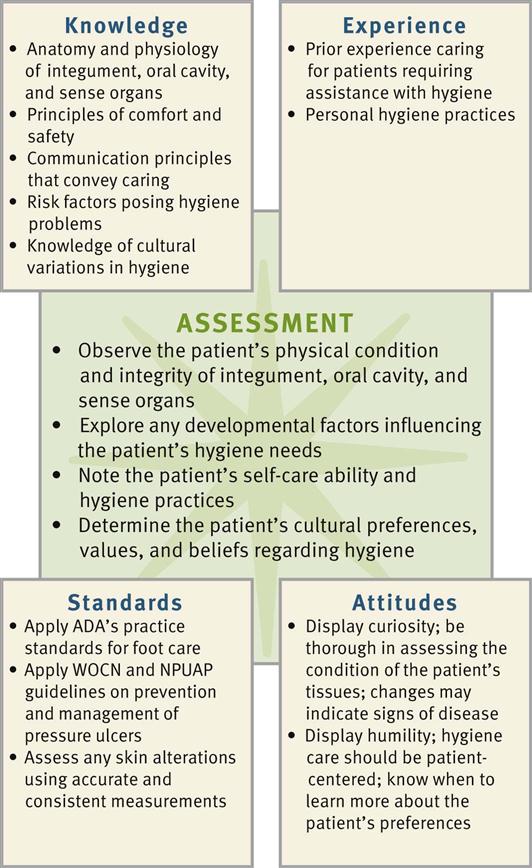
Critical Thinking
Effective critical thinking requires synthesis of knowledge, experience, information gathered from patients, critical thinking attitudes, and intellectual and professional standards. Clinical judgments require you to anticipate the information necessary to analyze data and make decisions regarding care. A patient’s condition is always changing, requiring ongoing critical thinking. During assessment consider all elements that build toward making appropriate nursing diagnoses (Fig. 39-1). Apply the elements of critical thinking as you use the nursing process to meet patients’ hygiene needs.
Integrate nursing knowledge with knowledge from other disciplines. For example, the patient with diabetes mellitus has special needs for nail and foot care. Knowledge about the pathophysiology of diabetes and its potential effects on his or her peripheral circulation and sensory status provides the scientific knowledge base needed to implement safe and effective foot care. In addition, integrate knowledge about developmental and cultural influences as you identify and meet hygiene needs.
Be aware of the impact of critical thinking attitudes as you plan and implement care. For example, think creatively to help patients adapt existing hygiene practices or develop new hygiene practices when illness or loss of function impairs self-care abilities. Be nonjudgmental and confident when providing care. Because of variations in individual patients’ physical status and hygiene practices, you need to approach care with an attitude of flexibility. For example, when caring for a patient who is fatigued, you pace activities and plan rest periods during hygiene care to prevent exhaustion.
Draw on your own experiences as you assist with your patients’ hygiene care. Reflect on times when you helped family members or others close to you with their hygiene. Usually an early clinical experience involves providing or assisting with hygiene care for a patient. Finally rely on professional standards such as those for skin and foot care from the American Diabetes Association (ADA) and specialty nursing groups such as Wound Ostomy Continency Nurses (WOCN) when planning care to meet a patient’s hygiene needs. As your experience and knowledge grow, your comfort and expertise in meeting the individualized hygiene needs of your patients increase.
Nursing Process
Apply the nursing process and use a critical thinking approach in your care of patients. The nursing process provides a clinical decision-making approach for you to develop and implement an individualized plan of care.
Assessment
During the assessment process thoroughly assess each patient and critically analyze findings to ensure that you make patient-centered clinical decisions required for safe nursing care. Assessment of a patient’s hygiene status and self-care abilities requires you to complete a nursing history and perform a physical assessment. You do not routinely assess all body regions before providing hygiene. However, you need to conduct a brief history to determine priority areas and help you plan individualized hygiene care. Assessment of a patient’s ability to provide hygiene self-care helps you make decisions about the kind and amount of hygiene care to provide and how much the patient can be encouraged to participate in care.
Through the Patient’s Eyes
Providing safe, quality hygiene care requires a complete awareness of the patient’s perspective. Because patients have varying expectations, you need to avoid making personal hygiene care a simple routine. Complete a nursing history that not only elicits personal preferences but also addresses the patient’s cultural or religious customs and beliefs.
Explore the patient’s viewpoint regarding hygiene care by asking him or her about preferred personal hygiene and grooming practices. Ask about personal care products desired and preferences such as frequency, time of day, and amount of assistance needed. Also ask questions such as “To make you most comfortable and feel at home, how can I best perform your bath and personal care?” Determine the patient’s awareness of any hygiene-related problems and his or her knowledge and ability to perform hygiene care measures (Box 39-2). Learning a patient’s expectations and applying them in practice fosters a caring relationship. Fully individualizing hygiene care shows the nurse’s respect for the patient’s needs. As you learn what the patient expects, you incorporate this information into a plan of care.
Assessment of Self-Care Ability
Assess a patient’s physical status as it relates to ability to perform or assist with hygiene care safely and efficiently; include assessment of the patient’s muscle strength, flexibility, balance, visual acuity, and ability to detect thermal and tactile stimuli. Determine your patient’s mental status, including orientation and cognitive function (see Chapter 30). The patient with impaired cognitive function may be unaware of hygiene care needs or less able to follow instructions and assist with care. Observe the patient performing hygiene care, noting complaints or physical manifestations that suggest activity intolerance. Assess respiratory rate and effort, skin color, and pulse rate. Ask questions to assess the patient for dizziness, weakness, or fatigue. To determine the amount of assistance the patient needs, observe him or her performing care activities such as brushing teeth or combing hair (Fig. 39-2). Patients who have limited upper-extremity mobility, reduced vision, fatigue, or inability to grasp small objects require assistance. For example, current evidence shows that older adults who have poor hand function have more dental plaque when they perform their own oral care (Padilha et al., 2007). Also note the presence of equipment such as IV lines or urinary catheters. When patients have self-care limitations, family may assist with care. Determine how the family can help the patient, how often they can provide this assistance, and what their feelings are about being caregivers. In addition, assess the home environment and its influence on the patient’s hygiene practices. Are there barriers in the home that affect his or her self-care abilities? Water faucets that are too tight to adjust easily, bathtubs with high sides, and a bathroom too small to fit a chair in front of a sink are a few examples.
Assessment of the Skin
Perform an assessment of the skin (see Chapter 30), noting color, texture, thickness, turgor, temperature, and hydration. In the healthy person the skin is smooth, warm, and supple with good turgor. Pay special attention to the presence and condition of any lesions. Note dryness of the skin indicated by flaking, redness, scaling, and cracking. Discovering manifestations of common skin problems influences how you administer hygiene care (Table 39-2).
TABLE 39-2
| CHARACTERISTICS | IMPLICATIONS | INTERVENTIONS |
| Dry Skin | ||
| Flaky, rough texture on exposed areas such as hands, arms, legs, or face | Skin becomes infected if epidermal layer cracks. | Bathe less frequently and rinse body of all soap because residue left on skin can cause irritation and breakdown. Add moisture to air with use of humidifier. Increase fluid intake when skin is dry. Use moisturizing cream to aid healing. (Cream forms protective barrier and helps maintain fluid within skin.) Use creams to clean skin that is dry or allergic to soaps and detergents. |
| Acne | ||
| Inflammatory, papulopustular skin eruption, usually involving bacterial breakdown of sebum; appears on face, neck, shoulders, and back | Infected material within pustule spreads if area is squeezed or picked. Permanent scarring can result. | Wash hair and skin thoroughly each day with warm water and soap to remove oil. Use cosmetics sparingly because oily cosmetics or creams accumulate in pores and tend to make condition worse. Implement dietary restrictions if necessary. (Eliminate foods that aggravate condition from diet.) Use prescribed topical antibiotics for severe forms of acne. |
| Skin Rashes | ||
| Skin eruptions that result from overexposure to sun or moisture or from allergic reaction (flat or raised, localized or systemic, pruritic or nonpruritic) | If skin is continually scratched, inflammation and infection may occur. Rashes also cause discomfort. | Wash area thoroughly and apply antiseptic spray or lotion to prevent further itching and aid in healing process. Apply warm or cold soaks to relieve inflammation if indicated. |
| Contact Dermatitis | ||
| Inflammation of skin characterized by abrupt onset with erythema; pruritus; pain; and appearance of scaly, oozing lesions (seen on face, neck, hands, forearms, and genitalia) | Dermatitis is often difficult to eliminate because person is usually in continual contact with substance causing skin reaction. Substance is often hard to identify. | Avoid causative agents (e.g., cleansers and soaps). |
| Abrasion | ||
| Scraping or rubbing away of epidermis that results in localized bleeding and later weeping of serous fluid | Infection occurs easily because of loss of protective skin layer. | Be careful not to scratch patient with jewelry or fingernails. Wash abrasions with mild soap and water; dry thoroughly and gently. Observe dressing or bandage for retained moisture because it increases risk of infection. |
Determine the degree of cleanliness by observing the appearance of the skin and detecting body odors that possibly indicate inadequate cleansing or excessive perspiration caused by fever or pain. Inspect less obvious or difficult-to-reach skin surfaces such as under the breasts or scrotum, around the female patient’s perineum, or in the groin for redness, excessive moisture, and soiling or debris. Separate skinfolds for observation and palpation.
Be attentive to characteristics of skin problems most influenced by hygiene measures. Is the skin dry from too much bathing or from use of hot water or irritating soap? Does the patient have a rash caused by an allergic reaction to a skin care product? Certain conditions place patients at risk for impaired skin integrity (Box 39-3). Because of increased risk be particularly alert when assessing patients with reduced sensation, impaired circulation, nutrition or hydration alterations, body secretions, incontinence, altered cognition, external devices, and decreased mobility. Patients may be unaware of skin problems because they are unable to feel pain or pressure or see their skin in some places (e.g., the back or the feet). Carefully assess the skin under orthopedic devices (braces, splints, casts) and beneath items such as antiembolic stockings and tape. Assess the condition and cleanliness of the perineal and anal areas during hygiene care and when the patient requires toileting assistance. When prolonged contact of urine or feces occurs such as with diarrhea or incontinence, skin breakdown often results. Most people consider these areas to be private. Use sensitivity in your approach.
When caring for patients with dark skin pigmentation, be aware of assessment techniques and skin characteristics unique to highly pigmented skin (see Chapter 30). Carefully assess the skin in dark-skinned patients at risk for pressure ulcers (see Chapter 48).
Assessment of the Feet and Nails
A variety of common foot and nail problems can be caused by inadequate hygiene and are actually detected during hygiene care. Problems sometimes result from abuse or poor care of the feet and hands such as nail biting or trimming nails improperly, exposure to harsh chemicals, and wearing poorly fitting shoes. Question the patient to determine type of footwear and usual foot and nail care practices.
Examine all skin surfaces of the feet, including the areas between the toes and over the entire sole of the foot. Poorly fitting shoes often irritate the heels, soles, and sides of the feet. Inspection of the feet for lesions includes noting areas of dryness, inflammation, or cracking. Chronic foot problems are common in older adults who often experience dry feet because of a decrease in sebaceous gland secretion, dehydration, or poor condition of footwear.
People are often unaware of foot or nail problems until pain or discomfort occurs. Assess patients with diseases that affect peripheral circulation and sensation for the adequacy of circulation and sensation of the feet. Foot ulceration is the most common single precursor to lower-extremity amputations among people with diabetes (Frykberg et al., 2006). Daily inspection and preventive foot care help maintain ulcer-free feet. Palpate the dorsalis pedis and posterior tibial pulses and assess for intact sensation to light touch, pinprick, and temperature (see Chapter 30).
Observe the patient’s gait. Painful foot disorders or decreased sensation cause limping or an unnatural gait. Ask whether the patient has foot discomfort and determine factors that aggravate the pain. Foot problems sometimes result from bone or muscular alterations or wearing poorly fitting footwear.
Inspect the condition of the fingernails and toenails, looking for lesions, dryness, inflammation, or cracking, which are often associated with a variety of common nail problems (Table 39-3). The cuticle that surrounds the nail can grow over it and become inflamed if nail care is not performed correctly and periodically. Ask women whether they frequently polish their nails and use polish remover because chemicals in these products cause excessive nail dryness. Disease changes the shape and curvature of the nails (see Chapter 30). Inflammatory lesions and fungus of the nail bed cause thickened, horny nails that separate from the nail bed.
TABLE 39-3
| CHARACTERISTICS | IMPLICATIONS | INTERVENTIONS |
| Callus | ||
| Thickened portion of epidermis consists of mass of horny, keratotic cells. Callus is usually flat, painless, and found on undersurface of foot or palm of hand. | Local friction or pressure causes callus formation, which causes discomfort when wearing tight shoes. | Soft-sole shoes with insoles are recommended. Advise patient to wear gloves when using tools or objects that create friction on palmar surfaces. Advise patients, especially with callus formation, not to self-treat but seek interventions from a podiatrist. |
| Corns | ||
| Friction and pressure from ill-fitting or loose shoes causes keratosis. It is seen mainly on or between toes, over bony prominence. Corn is usually cone shaped, round, and raised. Soft corns are macerated. | Compresses the underlying dermis, making it thin and tender. Pain is aggravated when wearing tight shoes. Tissue becomes attached to bone if allowed to grow. Patient suffers alteration in gait resulting from pain. | Surgical removal is necessary, depending on severity of pain and size of corn. Avoid use of oval corn pads, which increase pressure on toes and reduce circulation. Warm water soaks soften corns before gentle rubbing with a callus file or pumice stone (consult with health care provider). Wider and softer shoes, especially shoes with a wider toe box, are helpful. |
| Plantar Warts | ||
| Fungating lesion appears on sole of foot and is caused by the papilloma virus. | Some warts are contagious. They are painful and make walking difficult. | Treatment ordered by health care provider often includes applications of salicylic acid, electrodessication (burning with electrical spark), or freezing with solid carbon dioxide. |
| Athlete’s Foot (Tinea Pedis) | ||
| Athlete’s foot is fungal infection of foot; scaling and cracking of skin occurs between toes and on soles of feet. Small blisters containing fluid appear. | Athlete’s foot spreads to other body parts, especially hands. It is contagious and frequently recurs. | Make sure that feet are well ventilated. Drying feet well after bathing and applying powder help prevent infection. Wearing clean socks or stockings reduces incidence. Health care provider orders application of griseofulvin, miconazole, or tolnaftate. |
| Ingrown Nails | ||
| Toenail or fingernail grows inward into soft tissue around nail. Ingrown nail often results from improper nail trimming. | Ingrown nails cause localized pain when pressure is applied. | Treatment is frequent hot soaks in antiseptic solution and removal of part of nail that has grown into skin. Instruct patient in proper nail-trimming techniques and refer to podiatrist. |
| Foot Odors | ||
| Foot odors are result of excess perspiration, promoting microorganism growth. | Condition causes discomfort because of excess perspiration. | Frequent washing, use of foot deodorants and powders, and wearing clean footwear prevent or reduce problem. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree