Chapter 7 Hepatology
Basic concepts
1 Review the anatomy of the hepatic lobule and portal triad. In what manner do blood and bile flow through a lobule?
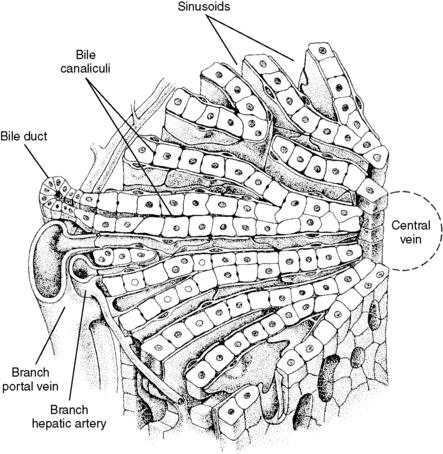
A central hepatic vein is located at the center of each hepatic lobule. Multiple portal triads (hepatic artery, portal venule, bile duct) surround this central vein. Hepatocytes are arranged in sheets of single-cell thickness and are surrounded by blood-filled sinusoids. Blood flows from the hepatic artery and portal vein toward the central vein through the sinusoids. Bile is formed by the hepatocytes and emptied into bile canuliculi in the lateral wall of the hepatocyte. The bile flows from here toward the bile ducts (Fig. 7-1).
2 What is the chemical difference between conjugated and unconjugated bilirubin and how are these substances formed?
4 What are the main causes of jaundice and how does each affect the type of hyperbilirubinemia observed?
See Table 7-1 for the causes of jaundice and the characteristics of each.
You should be able to differentiate between the causes and presentations of conjugated and unconjugated hyperbilirubinemias shown in Table 7-1. This is a commonly tested principle on boards. For those of you who do not fully understand the details of Table 7-1, we have provided our handy approach to reasoning through the causes of jaundice.
Secret to diagnosing common causes of jaundice
Now that you have the background on bilirubin formation and excretion, we can begin to explore the causes of jaundice. Jaundice may be the result of any abnormality along the aforementioned pathway. It can therefore occur as a result of (1) excessive bilirubin production, (2) decreased hepatic uptake or conjugation of indirect bilirubin, (3) decreased hepatocellular secretion of bilirubin into bile, or (4) impaired or obstucted bile flow. If this makes sense to you, it becomes very formulaic to tease apart the various causes of jaundice. All you have to do is match the various causes of jaundice listed in Table 7-1 to these basic mechanisms.
The final cause of jaundice mentioned in Table 7-1 is obstructive jaundice. Obstructive jaundice results when conjugated bilirubin is unable to be excreted into the gut either due to impaired liver secretion of bile (see item 3) or impaired bile flow (see item 4). The most common cause of obstructive jaundice is bile duct obstruction (e.g., gallstones, pancreatic tumor). Although conjugated bilirubin is produced and secreted into bile, the bile is unable to be secreted into the gut lumen due to an obstruction in the bile duct system. Bile backs up into the liver, causing engorgement and rupture of intrahepatic ducts. This leads to spillage of conjugated bilirubin into sinusoidal blood and, ultimately, the systemic circulation. Thus, conjugated bilirubin levels become elevated while urobilinogen levels decrease due to inadequate concentrations of conjugated bilirubin in the gut lumen. Urine color remains normal (conjugated bilirubin in the systemic circulation is water soluble and can be excreted by the kidneys), but stool becomes clay-colored due to lack of urobilinogen excretion into feces.
Now that you have a better understanding of the causes of jaundice, revisit Table 7-1 and attempt to fill it in on your own.
6 What are the symptoms of portal hypertension?
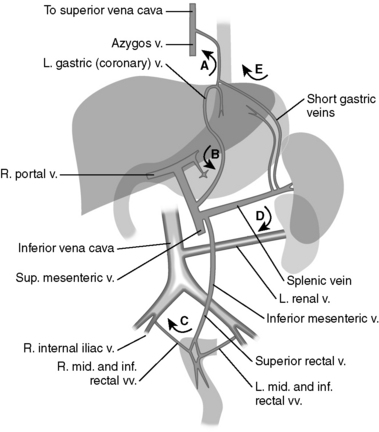
Portal hypertension leads to increased resistance to flow in the systemic venous system. As a result, blood cannot pass freely from the portal system to the systemic system and backs up into the portacaval anastomoses, which causes them to become engorged, dilated, or varicose. The location of these anastomoses determines the specific symptoms that result from portal hypertension. These symptoms and signs are listed in Table 7-2. General symptoms of portal hypertension include ascites (secondary to increased hydrostatic pressure), spontaneous bacterial peritonitis (note that ascitic fluid is a wonderful culture medium for bacteria), hepatorenal syndrome, and splenomegaly due to decreased drainage of venous blood from the spleen. Splenomegaly can result in anemia, thrombocytopenia, or pancytopenia due to cellular sequestration within the engorged spleen.
Table 7-2 Portal Hypertension: Anastomoses and Related Signs
| Portacaval Anastomosis | Clinical Sign |
|---|---|
| Left gastric vein with esophageal vein (branch of azygos vein) | Esophageal varices (leading to heavy bleeding/hematemesis) |
| Paraumbilical vein with epigastric vessels | Caput medusae |
| Superior rectal vein with middle and inferior rectal veins | Internal hemorrhoids (unlike external hemorrhoids, these are not painful because the visceral nerves that are above the dentate line sense pressure and not pain) |
4 To confirm your suspicion about severe liver disease in this patient, what physical examination findings might you expect and why?
Gynecomastia and testicular atrophy can be present, resulting from impaired ability of the damaged liver to metabolize estrogen. Estrogen also weakens vascular walls, leading to spider angiomata with increased estrogen levels. Hemorrhoids may result from a portacaval anastomosis between the superior rectal vein and the inferior rectal vein, and a caput medusae (engorged veins radiating from the umbilicus) can result from blood being diverted from the portal vein into the periumbilical veins that run along the round ligament of the liver to the anterior abdominal wall (see Table 7-2). An enlarged liver may be palpated with alcoholic hepatitis, but once cirrhosis develops, the liver will become firm and shrunken. A spleen tip may be palpable, as congestive splenomegaly may occur with portal hypertension because the splenic vein drains into the portal vein.
6 What is the pathogenesis of the suspected cause of hematemesis in this patient?
He most likely has ruptured esophageal varices (see Table 7-2). This patient has portal hypertension secondary to alcohol-induced cirrhosis. This creates portacaval anastomoses, in which the pressure in the portal venous system diverts blood from the portal system into the systemic circulation at sites where there are anastomoses. In this patient’s case, blood from the gastric veins backed up into his esophageal tributaries, which became distended and eventually ruptured (Fig. 7-2).
7 What is the value of the following tests: hepatitis serology, serum iron, ceruloplasmin, and antimitochondrial antibodies?
8 Assuming he is not taking any anticoagulants, what is the most likely reason this patient developed a large hematoma at the intravenous site?
9 List all the laboratory findings you would expect in a patient with liver failure
See Table 7-3 for the laboratory findings in liver failure and their underlying mechanisms.
Table 7-3 Common Findings in Patients With Liver Failure
| Laboratory Value | Mechanism |
|---|---|
| Elevated or normal LFT values | Liver enzymes may be elevated during initial damage, but if cirrhosis is present or the liver shrinks over time, liver enzyme levels may appear normal in the context of decreased hepatic tissue. |
| Elevated PT | The liver is the site of coagulation factor production. With severe liver damage, PT becomes elevated. |
| Elevated serum bilirubin concentration | The liver is responsible for bilirubin uptake. Liver failure causes a spike in serum bilirubin concentration due to decreased hepatic uptake. |
| Hypoalbuminemia | The liver is the predominant site of albumin production. Decreased serum protein concentration may clinically manifest as ascites. |
| Fasting hypoglycemia | Impaired gluconeogenesis and glycogenolysis during fasting. |
| Elevated estrogen levels | The liver is the site of estrogen breakdown. Liver damage elevates estrogen levels, which can lead to testicular atrophy and formation of spider angiomata. |
| Elevated ammonia levels with decreased BUN | The liver produces the enzymes involved in the urea cycle, which converts ammonia to urea. Elevated ammonia levels can result in hepatic encephalopathy, marked by confusion, loss of consciousness, asterixis, irritability, tremor, and coma. Increased ammonia also can result in fetor hepaticus (“breath of the dead”), which is characteristic of liver disease. |
ADH, antidiuretic hormone; BUN, blood urea nitrogen; LFT, liver function test; PT, prothrombin time.
10 Would you expect the ascitic fluid to be a transudate or an exudate?
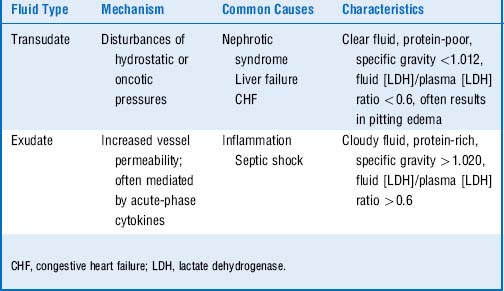
A transudate develops as a result of fluid moving across a membrane as a result of hemodynamic forces. Because there is no alteration in the permeability of the membranes that the fluid is moving across, the fluid that accumulates has low protein content. In contrast, exudates are fluid collections that develop because of alterations in membrane/vessel permeability, so proteins and cells accumulate in these fluid collections. Because this ascites is caused by lowered oncotic pressure (secondary to hypoalbuminemia) and portal hypertension, both of which alter hemodynamic forces but not vessel permeability, the result is a transudate. Table 7-4 lists the differences between transudates and exudates.
11 How does liver cirrhosis cause the following abnormalities?
The liver is a major site of amino acid metabolism and is the site of the urea cycle. Reduced output of the urea cycle because of hepatocyte destruction results in a lower BUN. Because the urea cycle is also the major site of ammonia detoxification, elevated blood ammonia levels become detectable as a sweet odor in the breath (fetor hepaticus). The elevated blood ammonia, which can enter the brain, can alter cerebral metabolism and contribute to confusion (hepatic encephalopathy) (see Table 7-3).
13 How does chronic alcohol consumption lead to a more rapid catabolism of ingested alcohol?
Alcohol can be degraded by two separate metabolic pathways, as shown in Figure 7-3.

Figure 7-3 The two pathways for alcohol metabolism. MEOS, microsomal ethanol-oxidizing system.
(Courtesy of Gloria Yueh, PhD, Midwestern University.)
14 Why are ethanol and fomepizole used to treat methanol poisoning and ethylene glycol poisoning?
Summary Box: Alcoholic Hepatitis and Ruptured Esophageal Varices
 The pathogenesis of hepatic damage in chronic alcohol abuse is poorly understood, but the result is often hepatic cirrhosis and portal hypertension.
The pathogenesis of hepatic damage in chronic alcohol abuse is poorly understood, but the result is often hepatic cirrhosis and portal hypertension.
 Alcoholic steatohepatitis (fatty liver) is initially reversible but can progress to cirrhosis with continued alcohol abuse. Cirrhosis is irreversible.
Alcoholic steatohepatitis (fatty liver) is initially reversible but can progress to cirrhosis with continued alcohol abuse. Cirrhosis is irreversible.
 Ruptured esophageal varices and Mallory-Weiss tears are uncommon in the general population but are often associated with alcoholic liver disease.
Ruptured esophageal varices and Mallory-Weiss tears are uncommon in the general population but are often associated with alcoholic liver disease.
 Ascitic fluid resulting from portal hypertension is a transudate. It has a low protein concentration and results from alterations in hemodynamic forces. Exudates have higher protein content and result from alterations in vessel permeability, and most commonly result from infection.
Ascitic fluid resulting from portal hypertension is a transudate. It has a low protein concentration and results from alterations in hemodynamic forces. Exudates have higher protein content and result from alterations in vessel permeability, and most commonly result from infection.
 Hepatic encephalopathy is in part caused by increased levels of plasma ammonia. Because dietary protein increases production of ammonia, patients with cirrhosis may be placed on a low-protein diet to minimize the risk of hepatic encephalopathy.
Hepatic encephalopathy is in part caused by increased levels of plasma ammonia. Because dietary protein increases production of ammonia, patients with cirrhosis may be placed on a low-protein diet to minimize the risk of hepatic encephalopathy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree