Chapter 14 Hematologic Malignancies
Insider’s Guide to Hematologic Malignancies for the USMLE Step 1
 Know all of the chromosomal translocations mentioned in this chapter and First Aid. Board exams love to test students on these points.
Know all of the chromosomal translocations mentioned in this chapter and First Aid. Board exams love to test students on these points.
 Pay careful attention to patient ages whenever they are given in the clinical history. Age can be very helpful in distinguishing various types of hematologic malignancies. You should especially memorize the age ranges for the most common types of leukemias. Acute lymphoblastic leukemia (ALL) occurs between the ages of 0 to 15, acute myelogenous leukemia (AML) occurs between the ages of 15 to 59, chronic myelogenous leukemia (CML) occurs between the ages of 40 to 59, and chronic lymphocytic leukemia (CLL) occurs after the age of 60 years. Keep in mind that boards will provide you with classic presentations for diseases, so memorizing particular rules like this one for the USMLE can be extremely helpful.
Pay careful attention to patient ages whenever they are given in the clinical history. Age can be very helpful in distinguishing various types of hematologic malignancies. You should especially memorize the age ranges for the most common types of leukemias. Acute lymphoblastic leukemia (ALL) occurs between the ages of 0 to 15, acute myelogenous leukemia (AML) occurs between the ages of 15 to 59, chronic myelogenous leukemia (CML) occurs between the ages of 40 to 59, and chronic lymphocytic leukemia (CLL) occurs after the age of 60 years. Keep in mind that boards will provide you with classic presentations for diseases, so memorizing particular rules like this one for the USMLE can be extremely helpful.
 Many high-yield images derive from this section. You should know how to diagnose different leukemias and lymphomas from images of peripheral blood smears or bone marrow aspirates. You should also know how to recognize Auer rods and Reed-Sternberg cells, two especially high-yield images covered in this section.
Many high-yield images derive from this section. You should know how to diagnose different leukemias and lymphomas from images of peripheral blood smears or bone marrow aspirates. You should also know how to recognize Auer rods and Reed-Sternberg cells, two especially high-yield images covered in this section.
 When learning the various hematologic malignancies, focus on the information that helps you differentiate these cancers from one another. Sometimes, this is all you need to know for boards. A great example is hairy cell leukemia, for which you should know that these cells have hairlike projections and stain positively with tartrate-resistant acid phosphatase (TRAP). These are the two most unique facts about hairy cell leukemia, and at least one of them is guaranteed to be provided in any question stem you may receive on this topic. It’s as simple as that. Use the information in this chapter (especially the tables) to guide what you should take away from each individual disease.
When learning the various hematologic malignancies, focus on the information that helps you differentiate these cancers from one another. Sometimes, this is all you need to know for boards. A great example is hairy cell leukemia, for which you should know that these cells have hairlike projections and stain positively with tartrate-resistant acid phosphatase (TRAP). These are the two most unique facts about hairy cell leukemia, and at least one of them is guaranteed to be provided in any question stem you may receive on this topic. It’s as simple as that. Use the information in this chapter (especially the tables) to guide what you should take away from each individual disease.
Basic concepts
2 What categories of hematologic malignancy arise from the lymphoid lineage?
 The lymphomas, including Hodgkin’s lymphoma and the various types of non–Hodgkin’s lymphoma (NHL)
The lymphomas, including Hodgkin’s lymphoma and the various types of non–Hodgkin’s lymphoma (NHL)
 The lymphocytic leukemias, including acute lymphoblastic leukemia (ALL) and chronic lymphocytic leukemia (CLL)
The lymphocytic leukemias, including acute lymphoblastic leukemia (ALL) and chronic lymphocytic leukemia (CLL)
 Tumors of plasma cells (antibody-secreting B cells), which include multiple myeloma and lymphoplasmacytic lymphoma
Tumors of plasma cells (antibody-secreting B cells), which include multiple myeloma and lymphoplasmacytic lymphoma
4 What is the distinction between small cell lymphocytic lymphoma (SLL) and (B-cell) chronic lymphocytic leukemia (B-CLL)?
Note: Smudge cells are a characteristic feature of CLL on a peripheral smear.
5 What categories of hematologic neoplasms arise from the myeloid lineage?
 Acute myelogenous leukemia (AML), which has multiple subclassifications
Acute myelogenous leukemia (AML), which has multiple subclassifications
 Myelodysplastic syndromes, all potential precursors of AML
Myelodysplastic syndromes, all potential precursors of AML
 Myeloproliferative disorders, including polycythemia vera (PV), chronic myelogenous leukemia (CML), and essential thrombocythemia
Myeloproliferative disorders, including polycythemia vera (PV), chronic myelogenous leukemia (CML), and essential thrombocythemia
11 How does the leukocyte alkaline phosphatase level help differentiate reactive leukocytosis from a true leukemia?
12 Quick review! Cover the right column in Table 14-1 and attempt to list the cell type and pertinent high-yield facts regarding the hematologic malignancies in the left column
| Disorder | Cell Type/Comments |
|---|---|
| Lymphoid Lineage | |
| Acute lymphoblastic leukemia | Precursor B or T lymphocytes (lymphoblasts) |
| Chronic lymphocytic leukemia/small lymphocytic lymphoma | B cells, smudge cells on peripheral smear |
| Hodgkin’s lymphoma | Reed-Sternberg cells |
| Lymphoplasmacytoma | Plasma cells (mature B cells—IgM-secreting); a common cause of Waldenström’s macroglobulinemia |
| Multiple myeloma | Plasma cells (mature B cells—IgG- and IgA-secreting) |
| Non-Hodgkin’s lymphoma | Multiple types, which generally are classified according to site in lymph node they resemble (e.g., follicular, mantle zone, marginal zone) |
| Myeloid Lineage | |
| Acute myelogenous leukemia | Cells of early myeloid lineage |
| Histiocytosis | Langerhans cell (of monocyte-macrophage origin) |
| Myelodysplastic syndromes | Hematopoietic stem cell with ineffective hematopoiesis that replaces bone marrow |
| Myeloproliferative syndromes | Clonal expansion of a multipotent hematopoietic stem cell, ultimately giving rise to excess numbers of one or more final products of the myeloid lineage |
IgA, IgG, IgM, immunoglobulins A, G, and M.
13 Quick review! Cover the right column in Table 14-2 and attempt to define the hematologic terms in the left column
Table 14-2 Hematologic Terminology
| Term | Definition |
|---|---|
| Leukemia | Malignant proliferation of blood cells within the bone marrow and circulatory system |
| Leukemoid reaction | Abnormally high WBC count, similar to that occurring in various forms of leukemia, but not as the result of leukemia (typically in response to infection) |
| Lymphoma | Proliferating mass of lymphocytic cells: B cells (most common), T cells, NK cells |
| Myelofibrosis | Fibrosis of bone marrow, often causing extramedullary hematopoiesis that results in hepatosplenomegaly |
| Myelophthisic anemia | Anemia that arises from a space-occupying lesion that displaces normal hematopoietic elements |
NK, natural killer; WBC, white blood cell.
14 What are the genetic alterations in the following non-Hodgkin’s lymphomas?
Table 14-3 Genetic Alterations in Non-Hodgkin’s Lymphoma
| Non-Hodgkin’s Lymphoma | Genetic Alterations |
|---|---|
| Burkitt’s lymphoma | Translocation between chromosomes 8 and 14, involves c-myc activation on chromosome 8; often associated with HIV infection; EBV infection common in African Burkitt’s (patients present with jaw mass) Sporadic form is associated with pelvic and abdominal lesions Look for characteristic “starry sky” appearance of Burkitt’s type, due to sheets of neoplastic lymphocytes infiltrated with occasional macrophages |
| Follicular lymphoma | Translocation between chromosomes 14 and 18 involving BCL2 activation (antiapoptosis gene) Associated with painless, generalized lymphadenopathy, primarily in adults |
| Mantle cell lymphoma | Translocation between chromosomes 11 and 14, which increases cyclin D expression and promotes cell cycle progression Associated with CD5 expression Usually fatal, occurs in adults Cells resemble mantle zone cells that surround follicular centers |
EBV, Epstein-Barr virus; HIV, human immunodeficiency virus.
15 What are some characteristics of the other non-Hodgkin’s lymphomas?
Table 14-4 Characteristics of Non-Hodgkin’s Lymphoma (NHL)
| NHL Type | Description |
|---|---|
| Cutaneous T-cell lymphoma | Caused by a T-cell dyscrasia, unlike most NHLs, which are B cell in origin Examples are mycosis fungoides and Sézary syndrome T-cell lymphomas are associated with cutaneous lesions |
| Diffuse large B-cell lymphoma | Very aggressive lymphoma occurring mostly in older adults but sometimes in children Associated with BCL6 overexpression, which silences p53 Early stage is responsive to treatment |
| Marginal zone lymphoma (MALToma) | Begins as reactive polyclonal B cell proliferation, culminating in monoclonal B-cell neoplasm |
16 Quick review with high-yield word associations: Cover the right column of Table 14-5 and attempt to list the associated diseases
Table 14-5 High-Yield Word Associations
| Description | Disease |
|---|---|
| >30% myeloid blasts in bone marrow | Acute myelogenous leukemia (AML) |
| 8:14 translocation | Burkitt’s lymphoma |
| 14:18 translocation involving BCL2 | Follicular lymphoma |
| Auer bodies | Acute myelogenous leukemia |
| Bence Jones proteinuria | Multiple myeloma |
| Massive splenomegaly, B-cell proliferation, and presence of tartrate-resistant acid phosphatase in B cells | Hairy cell leukemia |
| Philadelphia chromosome | Chronic myelogenous leukemia (CML) |
| Reed-Sternberg (lacunar) cells | Hodgkin’s lymphoma |
| Smudge cells on peripheral blood smear | Chronic lymphocytic leukemia (CLL) |
1 What is the differential diagnosis for back pain in an older patient?
Case 14-1 continued:
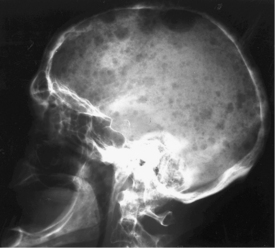
An x-ray film of the skull for evaluation of his sinus infections is shown in Figure 14-1. Serum protein electrophoresis reveals an M spike. A urine dipstick test is negative for proteinuria, but a 24-hour urine protein collection reveals marked proteinuria.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree