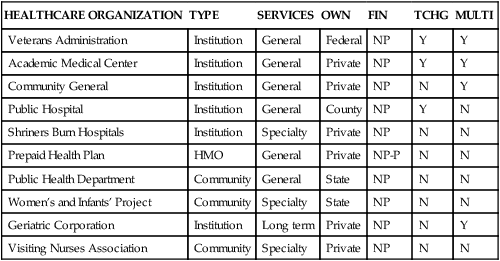
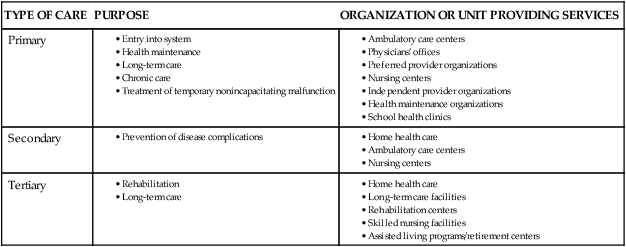
• Identify and compare characteristics that are used to differentiate healthcare organizations. • Classify healthcare organizations by major types. • Analyze economic, social, and demographic forces that drive the development of healthcare organizations. • Describe the impact of the evolution of healthcare organizations on nursing leadership and management roles. Another characteristic that is used to differentiate healthcare organizations is the duration of the care provided. According to the American Hospital Association (AHA) (2009), most hospitals are acute care facilities giving short-term, episodic care. The AHA defined an acute care hospital as a facility in which the average length of stay is less than 30 days. Chronic care or long-term facilities provide services for patients who require care for extended periods in excess of 30 days. In acute care institutions, patients are discharged as soon as their conditions are stabilized. An example of a long-term care facility is a geriatric organization that provides care services from onset of impairment until death. Many institutions have components of both short-term and long-term services. They may provide acute care, home care, hospice care, ambulatory clinic care, day surgery, and an increasing number of other services, such as day care for dependent children and adults or focused services such as Meals-on-Wheels. The term healthcare network refers to interconnected units that either are owned by the institution or have cooperative agreements with other institutions to provide a full spectrum of wellness and illness services. The spectrum of care services provided are typically described as primary care (first-access care), secondary care (disease-restorative care), and tertiary care (rehabilitative or long-term care). Table 7-1 describes the continuum of care and the units of healthcare organizations that provide services in the three phases of the continuum. TABLE 7-1 CONTINUUM OF HEALTHCARE ORGANIZATIONS Ownership is another characteristic used to classify healthcare organizations. Ownership establishes the organization’s legal, business, and mission-related imperative. Healthcare organizations have three basic ownership forms: public, private non-profit, and for-profit. Public institutions provide health services to individuals under the support and/or direction of local, state, or federal government. These organizations must answer directly to the sponsoring government agency or boards and are indirectly responsible to elected officials and taxpayers who support them. Examples of these service recipients at the federal level are veterans, members of the military, Native Americans and prisoner healthcare organizations. State-supported organizations may be health service teaching facilities, chronic care facilities, and prisoner facilities. Locally supported facilities include county-supported and city-supported facilities. Table 7-2 shows how several common healthcare organizations are classified. Private non-profit (or not-for-profit) organizations—often referred to as voluntary agencies—are controlled by voluntary boards or trustees and provide care to a mix of paying and charity patients. In these organizations, excess revenue over expenses is redirected into the organization for maintenance and growth rather than returned as dividends to stockholders. These organizations are required to serve people regardless of their ability to pay. Non-profit organizations located in impoverished urban and rural areas are often economically disadvantaged by the amount of uncompensated care that they provide. In 2007, roughly 60% of uncompensated care in the United States was provided by 14% of hospitals (United States Department of the Treasury, 2009). Some states, such as New York, have created charity pools to which all non-profit organizations in the state are required to contribute to offset financial problems of the disadvantaged institutions. Historically, non-profit organizations have been exempt from paying taxes as they commit to providing an important community service. The owners of such organizations include churches, communities, industries, and special interest groups such as the Shriners. It is important for nurses to understand the impact of ownership on how organizations are structured, the services they provide, and the patients they serve. Teaching status is a characteristic that can differentiate healthcare organizations. The term teaching institution is applied to academic health centers (those directly affiliated with a school of medicine and at least one other health profession school) and affiliated teaching hospitals (those that provide only the clinical portion of a medical school teaching program). Studies have shown that although care is usually more costly at teaching hospitals than at non-teaching hospitals (estimates range from 12% more expensive in Canada to 27% in the United States), teaching hospitals generally offer better care because of their access to state-of-the-art technology and researchers. The higher costs of teaching hospitals have been attributed to the unique missions these institutions tend to pursue, including graduate medical education, biomedical research, and the maintenance of stand-by capacity for highly specialized patient care (Flatt & Rahal, 2006). Whether or not a healthcare organization has been accredited by an external body as having the structure and process necessary to provide high quality care is another characteristic that can be used to distinguish one organization from another. Private organizations play significant roles in establishing standards and ensuring care delivery compliance with standards by accrediting healthcare organizations. Examples of these organizations are The Joint Commission and The National Committee for Quality Assurance (NCQA). The Joint Commission provides accreditation programs for ambulatory care, behavioral health care, acute care and critical access hospitals, laboratory services, long-term care, and hospital-based surgery. The NCQA is a non-profit organization that accredits, certifies, and recognizes a wide variety of healthcare organizations, services, and providers. More information on accrediting organizations is provided in the “Accrediting Bodies” section on pp. 125-126.
Healthcare Organizations

Characteristics and Types of Organizations
Institutional Providers
Length of Direct Care Services Provided
TYPE OF CARE
PURPOSE
ORGANIZATION OR UNIT PROVIDING SERVICES
Primary
Secondary
Tertiary
Ownership
Teaching Status
Accreditation Status
Healthcare Organizations
Get Clinical Tree app for offline access