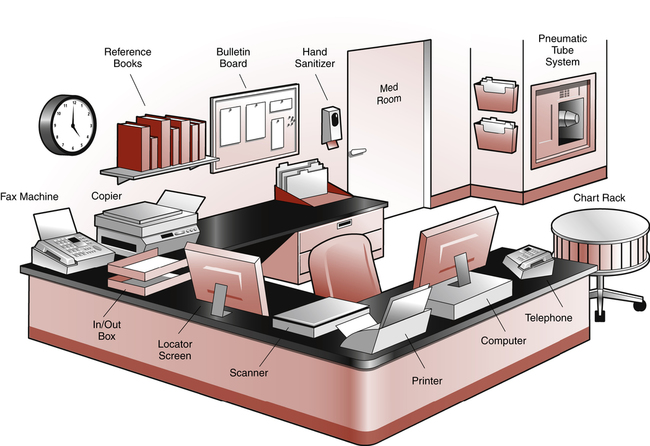
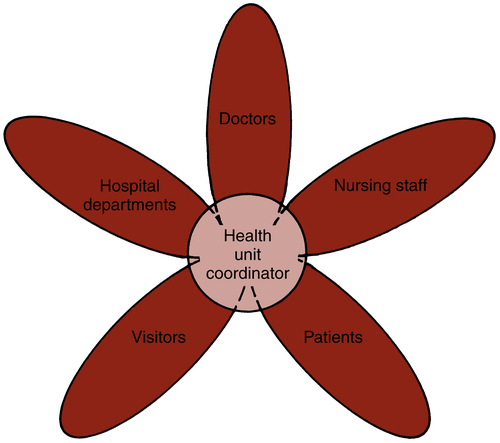
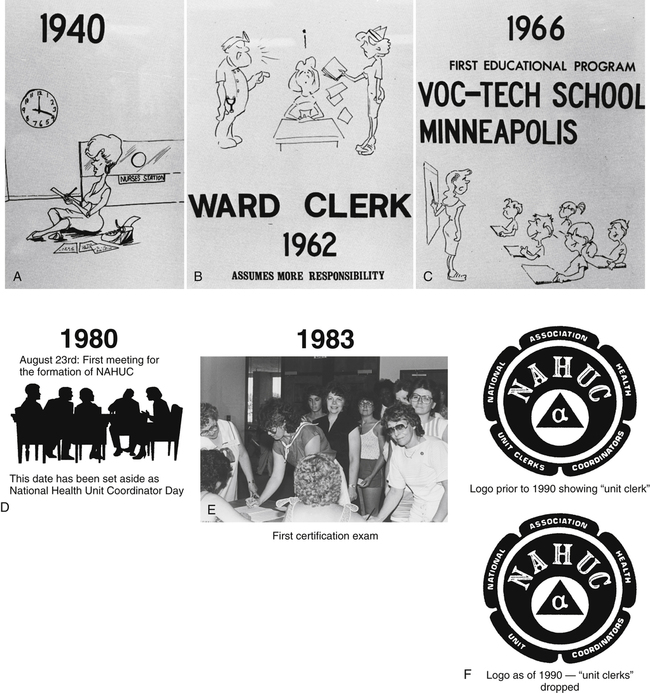
On completion of this chapter, you will be able to: 1. Define the terms in the vocabulary list. 2. Write the meaning of the abbreviations in the abbreviations list. 3. Identify four stages that health professions have traditionally gone through to become a profession. 4. Explain the events that led up to creating the position that eventually became known as health unit coordinator (HUC). 5. List five benefits of being a member of the National Association of Health Unit Coordinators. 6. List five benefits of becoming a certified HUC. 7. List three tasks that the HUC would perform related to each of the following: nursing personnel, doctors, hospital departments, patients, and hospital visitors. 8. Discuss the benefits of using the electronic medical record (EMR), computer physician order entry (CPOE) with e-prescribing, and clinical decision support system (CDSS). 9. Identify four ways to prepare for the changing HUC position with the use of EMR and six things that the HUC can do to stay current in the position. 10. Demonstrate use of the Internet and search engines to locate information on the Web. 11. List three positions in which the HUC may be cross-trained. 12. List two possible nonclinical career choices for the health unit coordinator. A computer program that allows one to search for and view (or hear) various kinds of information on the Web, such as websites, videos, and audio files. The process of testifying that a person has met certain standards, or endorsing him or her as having met them. Certified Health Unit Coordinator (CHUC) A health unit coordinator who has passed the national certification examination sponsored by the National Association of Health Unit Coordinators (NAHUC). Clinical Decision Support System (CDSS) An interactive decision support system (DSS) computer program designed to assist physicians at the point of order entry. Tasks performed at the bedside or in direct contact with the patient (direct patient care). Computer Physician Order Entry (CPOE) A computerized program into which physicians directly enter patient orders; replaces handwritten orders on an order sheet or prescription pad. A person licensed to practice medicine (used interchangeably with the term physician throughout this textbook). The health care that a doctor prescribes in writing for a hospitalized patient. Electronic Medical Record (EMR) An electronic record of patient health information generated by one or more encounters in any care delivery setting. E-Prescribing (electronic prescribing) The electronic transmission of prescription information from the prescriber’s computer (hospital or doctor’s office) to a pharmacy computer. The health care team member who performs nonclinical patient care tasks for the nursing unit (also may be called unit clerk or unit secretary). Divisions within the hospital that specialize in services, such as the nutritional care department, which plans and prepares meals for patients, employees, and visitors. A company that provides Internet connections and services to individuals and organizations for a monthly fee. Use of certified electronic medical record (EMR) technology in ways that can be measured significantly in quality and in quantity. Tasks performed away from the bedside (indirect patient care). The desk area of a nursing unit. A group of nursing staff members who care for patients on a nursing unit. An area within the hospital that includes equipment and nursing personnel available for the care of a given number of patients (also may be referred to as a wing, floor, pod, ward, or station). A person who receives health care, including preventive, promotional, acute, and chronic, and all other services in the continuum of care. Information such as guidelines for practice and hospital regulations found online or in a manual. A process by which certified health unit coordinators exhibit continued personal and professional growth and current competency to practice in the field. A website that collects and organizes content from all over the Web. Using different search engines on the Web to locate information. A process used to communicate the doctors’ orders to the nursing staff and other hospital departments; computers or handwritten requisitions are used. Web Address (uniform resource locator [URL]) A series of characters (often preceded by “http://www”) that, when entered into the address bar of an Internet browser will take the user to a specified location, referred to as a website. The health unit coordinator (HUC) is usually the first person encountered when one walks onto a hospital nursing unit. The HUC has always been considered essential to the nursing team and to the effectiveness of the unit. The HUC coordinates activities on the unit, monitors the electronic medical record (EMR), or transcribes handwritten or preprinted doctor’s orders, and functions under the direction of the nurse manager or unit manager. The overall job is nonclinical in nature, and the work area is the nurses’ station (Fig. 1-1). Most everyone who works on or visits the nursing unit depends on the HUC for information and assistance. Comments often heard in the hospital include the following: • “We are so disorganized if the HUC isn’t here.” • “The HUC creates the attitude for the entire unit.” • “The HUC sets the pace for the day’s work.” Working on a nursing unit can be very fast paced and stressful; the HUC must possess a calming, pleasant, and professional attitude, because the HUC sets the tone for the unit. Whether an efficient HUC is working on a nursing unit is usually obvious to anyone who walks onto that unit. If the HUC is having a bad day or is in a bad mood, the whole unit is affected because everyone has to interact with the HUC. It is important for staff members to maintain a positive, friendly attitude when working on the nursing unit. The HUC can enhance or inhibit the delivery of health care to patients on the unit. The position involves many responsibilities associated with assisting the nursing staff, doctors, hospital departments, patients, and visitors to the nursing unit (Fig. 1-2). Many health care facilities require the HUC to wear scrubs, sometimes in a particular color, whereas other facilities opt for professional, nonclinical dress. In some facilities, HUCs may be cross-trained and may alternate working as HUCs, a nonclinical position—away from the patient bedside—and as certified nursing assistants (CNAs; discussed in Chapter 3), a clinical position—at the patient (pt) bedside. HUCs also may be employed in doctors’ offices, clinics, and long-term care facilities to assist with clerical or management duties related to patients’ health records. After World War II ended, the nursing shortage was not as critical; however, as technology advanced and the workload of the doctor increased, many tasks shifted to the nursing staff (e.g., taking blood pressure and starting intravenous therapy). Hospitals were becoming larger and more complex; there were more specialists, who were ordering newly available tests and treatments. Federally sponsored health programs required more detailed record keeping, and nonclinical demands for every hospitalized patient increased proportionately, so the need to employ HUCs continued. Today HUCs remain valued members of the hospital’s health care team, and the role continues to change and expand. HUCs were trained on the job for longer than 20 years (Fig. 1-3, A and B). In 1966 a research project led to the implementation of one of the first educational programs for health unit coordinating at a vocational school in Minneapolis (Fig. 1-3, C). An article published in Nursing Outlook authored by Ruth Stryker described the project and recommended that the title “ward” or “unit clerk” be changed to “station coordinator” because the data showed that the unit clerk did a great deal of managing in the form of coordinating activities. Ruth Stryker later wrote one of the first textbooks for health unit coordinating, The Hospital Ward Clerk, which was published by the C.V. Mosby Company in 1970. Today, before employment, most HUCs are educated in one of the many community colleges or vocational technical schools nationwide that offer HUC educational programs. The individual who completes a program emerges with better preparation for the job and a greater knowledge base on which to build. Educational programs outline the competencies or job skills that students are expected to acquire by the time they have completed the program (Box 1-1, Example of Competencies for an Educational Program for the Student Health Unit Coordinator). The first organizational meeting was held in Phoenix, Arizona, on August 23, 1980. This date has since been proclaimed National Health Unit Coordinator Day by the national association. The 10 founding members who represented both education and practice (Box 1-2, Founding Members of the National Association of Health Unit Coordinators) declared the formation of a national association for health coordinators to be called the National Association of Health Unit Coordinators (NAHUC) (Fig. 1-3, D). A new title, Health Unit Clerk/Coordinator, was created for the position; the title would be updated and used consistently nationwide. Because “unit clerk” was the most popular title nationwide in 1980, it was included in the title with the intent that it would be dropped when the term “coordinator” became recognized. In 1990, the national association became the National Association of Health Unit Coordinators, after “clerk” was dropped from its name (Fig. 1-3, F).
Health Unit Coordinating
An Allied Health Career
Abbreviation
Meaning
CDSS
clinical decision support system
CHUC
certified health unit coordinator
CPOE
computer physician order entry
EMR or EHR
electronic medical (health) record
HIMSS
Healthcare Information and Management Systems Society
HUC
health unit coordinator
SHUC
student health unit coordinator
pt
patient
www
World Wide Web
Introduction to Health Unit Coordinating
History of Health Unit Coordinating
On-the-Job-Training
Formal Education
Professional Association
Health Unit Coordinating: An Allied Health Career
Get Clinical Tree app for offline access