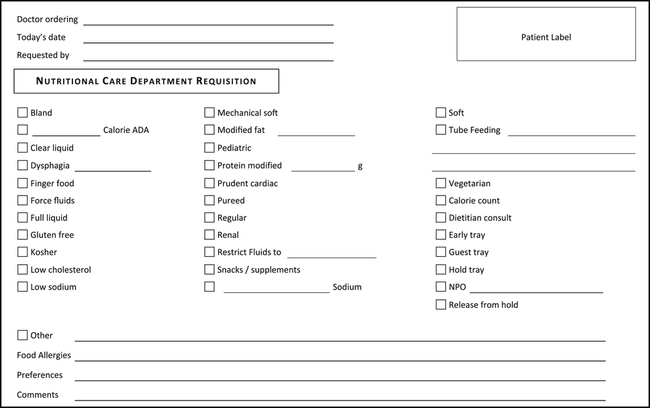
On completion of this chapter, you will be able to: 1. Define the terms listed in the vocabulary list. 2. Write the meaning of the abbreviations in the abbreviations list. 3. Explain the importance of communicating diet changes and patient food allergies to the nutritional care department. 4. Discuss the methods that may be used by the health unit coordinator (HUC) to order a late tray for a patient. 5. Discuss two eating disorders and other factors that a doctor would need to consider when ordering a hospitalized patient’s diet. 6. List three groups of diets that may be ordered for the hospitalized patient. 7. List five consistency changes that can be made to a standard diet, and explain what is included in each. 8. List four diet options that may be selected for the patient who has started on clear liquids and has an order for diet as tolerated, and explain how the selection would be made. 9. Identify two diets that may be requested by patients. 10. Identify at least five therapeutic diets that the patient’s doctor may order. 11. Discuss the reasons a patient would require a tube feeding, and list three methods of administering tube feedings. 12. List three items a HUC may need to order when transcribing an order for tube feeding. 13. Explain the purpose of the doctors’ orders force fluids, limit fluids, and calorie count, and discuss the importance of sending all doctors’ orders regarding a patient’s diet or modifications to a patient’s diet to the nutritional care department. 14. Discuss the importance of sending total parenteral nutrition (TPN) orders to the pharmacy in a timely manner. Condition characterized by intense fear of gaining weight or becoming fat, although underweight. Rounded mass of food formed in the mouth and ready to be swallowed; also defined as a concentrated dose of medication or fluid, frequently given intravenously (discussed in Chapter 13). A measurement of energy generated in the body by the heat produced after food is eaten. A doctor’s order that states the type and quantity of food and liquids the patient may receive. Dietary Reference Intake (DRI) Difficulty eating and swallowing. The provision of liquid formulas into the gastrointestinal tract by tube or by mouth. Inflammation of the stomach and intestines. Adequate water in the intracellular and extracellular compartments of the body. The act of taking in food by mouth. A brand name of a feeding pump used to administer tube feeding. An excess of body fat that threatens necessary body functions such as respiration. Having an excess amount of body fat, usually defined by body mass index. Condition characterized by an excess amount of body fat, usually defined by body mass index. Partial Parenteral Nutrition (PPN) Percutaneous Endoscopic Gastrostomy Insertion of a tube through the abdominal wall into the stomach under endoscopic guidance. Recommended Dietary Allowance (RDA) A diet that consists of all foods and is designed to provide good nutrition. Total Parenteral Nutrition (TPN) The provision of all necessary nutrients via veins (discussed in detail in Chapter 13). Administration of liquids into the stomach, duodenum, or jejunum through a tube. If the computer system is unavailable, the diet is ordered from the nutritional care department via a written downtime requisition. The diet order is later entered into the computer to maintain a record (Fig. 12-1).
Nutritional Care Orders
Abbreviation
Meaning
Example of Usage on a Doctor’s Order Sheet
ADA
American Diabetes Association
1200 cal ADA diet
ADD
attention-deficit disorder
ADD diet
AHA
American Heart Association
Follow AHA diet
BMI
body mass index
Calculate BMI
cal
calorie
1800 cal diet
CHO
carbohydrate
High-protein, low-CHO diet
chol
cholesterol
Low-chol diet
cl
clear
Cl liq diet
DAT
diet as tolerated
Advance DAT
FF
force fluids
Soft diet FF
FS
full strength
Jevity FS @ 50 mL/hr
K or K+
potassium
Low K+ diet
Liq
liquid
Full liq diet
MN
midnight
NPO MN
Na or Na+
sodium
2000 mg Na diet (2000 mg/2 g)
NAS
no added salt
Reg diet, NAS
NPO
nothing by mouth
NPO after midnight
NSA
no salt added (same as NAS)
PEG
percutaneous endoscopic gastrostomy
PEG in a.m.
RD
registered dietitian
RD consult requested
reg
regular
Reg diet
Communication with the Nutritional Care Department
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nurse Key
Fastest Nurse Insight Engine
Get Clinical Tree app for offline access
