Health and Wellness
Objectives
• List the two general Healthy People 2020 public health goals for Americans.
• Discuss the definition of health.
• Describe variables influencing health beliefs and practices.
• Describe health promotion, wellness, and illness prevention activities.
• Discuss the three levels of preventive care.
• Describe four types of risk factors.
• Discuss risk factor modification and changing health behaviors.
• Describe variables influencing illness behavior.
• Describe the impact of illness on the patient and family.
Key Terms
Active strategies of health promotion, p. 71
Acute illness, p. 74
Chronic illness, p. 74
Health, p. 66
Health behavior change, p. 73
Health behaviors, p. 66
Health belief model, p. 66
Health promotion, p. 70
Holistic health model, p. 67
Illness, p. 73
Illness behavior, p. 74
Illness prevention, p. 71
Passive strategies of health promotion, p. 71
Primary prevention, p. 71
Risk factor, p. 71
Secondary prevention, p. 71
Tertiary prevention, p. 71
Wellness, p. 71
![]()
In the past most individuals and societies viewed good health, or wellness, as the opposite or absence of disease. This simple attitude ignores states of health between disease and good health. Health is a multidimensional concept and is viewed from a broader perspective. An assessment of the patient’s state of health is an important aspect of nursing.
Models of health offer a perspective to understand the relationships between the concepts of health, wellness, and illness. Nurses are in a unique position to help patients achieve and maintain optimal levels of health. They need to understand the challenges of today’s health care system and embrace the opportunities to promote health and wellness and prevent illness. In an era of cost containment and advanced technology, nurses are a vital link to the improved health of individuals and society. They identify actual and potential risk factors that predispose a person or a group to illness. In addition, the nurse uses risk factor modification strategies to promote health and wellness and prevent illness.
Different attitudes cause people to react in different ways to illness or the illness of a family member. Medical sociologists call this reaction illness behavior. Nurses who understand how patients react to illness can minimize its effects and help patients and their families maintain or return to the highest level of functioning.
Healthy People Documents
Healthy People provides science-based, 10-year national objectives for promoting health and preventing disease. In 1979 an influential document, Healthy People: the Surgeon General’s Report on Health Promotion and Disease Prevention, was published; it introduced a goal for improving the health of Americans by 1990. The report outlined priority objectives for preventive services, health protection, and health promotion that addressed improvements in health status, risk reduction, public and professional awareness of prevention, health services and protective measures, and surveillance and evaluation. The report served as a framework for the 1990s as the United States increased the focus on health promotion and disease prevention instead of illness care. The strategy announced by the Secretary of Health and Human Services required a cooperative effort by government, voluntary and professional organizations, businesses, and individuals. Widely cited by popular media, in professional journals, and at health conferences, it has inspired health promotion programs throughout the country.
Healthy People 2000: National Health Promotion and Disease Prevention Objectives, published in 1990, identified health improvement goals and objectives to be reached by the year 2000 (U.S. Department of Health and Human Services [USDHHS, Public Health Service], 1990). Healthy People 2010, published in 2000, served as a road map for improving the health of all people in the United States for the first decade of the twenty-first century (USDHHS, 2000). This edition emphasized the link between individual health and community health and the premise that the health of communities determines the overall health status of the nation. Healthy People 2020 was approved in December 2010. Healthy People 2020 promotes a society in which all people live long, healthy lives. There are four overarching goals: (1) attain high-quality, longer lives free of preventable disease, disability, injury, and premature death; (2) achieve health equity, eliminate disparities, and improve the health of all groups; (3) create social and physical environments that promote good health for all; and (4) promote quality of life, healthy development, and healthy behaviors across all life stages (USDHHS, 2011).
Definition of Health
Defining health is difficult. The World Health Organization (WHO) defines health as a “state of complete physical, mental, and social well-being, not merely the absence of disease or infirmity” (WHO, 1947). Many other aspects of health need to be considered. Health is a state of being that people define in relation to their own values, personality, and lifestyle. Each person has a personal concept of health. Pender, Murdaugh, and Parsons (2011) define health as the actualization of inherent and acquired human potential through goal-directed behavior, competent self-care, and satisfying relationships with others while adjustments are made as needed to maintain structural integrity and harmony with the environment.
Individuals’ views of health vary among different age-groups, genders, races, and cultures (Pender, Murdaugh, and Parsons, 2011). Pender (1996) explains that “all people free of disease are not equally healthy.” Views of health have broadened to include mental, social, and spiritual well-being and a focus on health at the family and community levels (Pender, Murdaugh, and Parsons, 2006).
To help patients identify and reach health goals, nurses discover and use information about their concepts of health. Pender, Murdaugh, and Parsons (2011) suggest that for many people conditions of life rather than pathological states define health. Life conditions can have positive or negative effects on health long before an illness is evident (Pender, Murdaugh, and Parsons, 2011). Life conditions include socioeconomic variables such as environment, diet, and lifestyle practices or choices and many other physiological and psychological variables.
Health and illness are defined according to individual perception. Health often includes conditions previously considered to be illness. For example, a person with epilepsy who has learned to control seizures with medication and who functions at home and work may no longer consider himself or herself ill. Nurses need to consider the total person and the environment in which the person lives to individualize nursing care and enhance meaningfulness of the patient’s future health status.
Models of Health and Illness
A model is a theoretical way of understanding a concept or idea. Models represent different ways of approaching complex issues. Because health and illness are complex concepts, models are used to understand the relationships between these concepts and the patient’s attitudes toward health and health behaviors.
Health beliefs are a person’s ideas, convictions, and attitudes about health and illness. They may be based on factual information or misinformation, common sense or myths, or reality or false expectations. Because health beliefs usually influence health behavior, they can positively or negatively affect a patient’s level of health. Positive health behaviors are activities related to maintaining, attaining, or regaining good health and preventing illness. Common positive health behaviors include immunizations, proper sleep patterns, adequate exercise, stress management, and nutrition. Negative health behaviors include practices actually or potentially harmful to health such as smoking, drug or alcohol abuse, poor diet, and refusal to take necessary medications.
Nurses developed the following health models to understand patients’ attitudes and values about health and illness and to provide effective health care. These nursing models allow you to understand and predict patients’ health behavior, including how they use health services and adhere to recommended therapy.
Health Belief Model
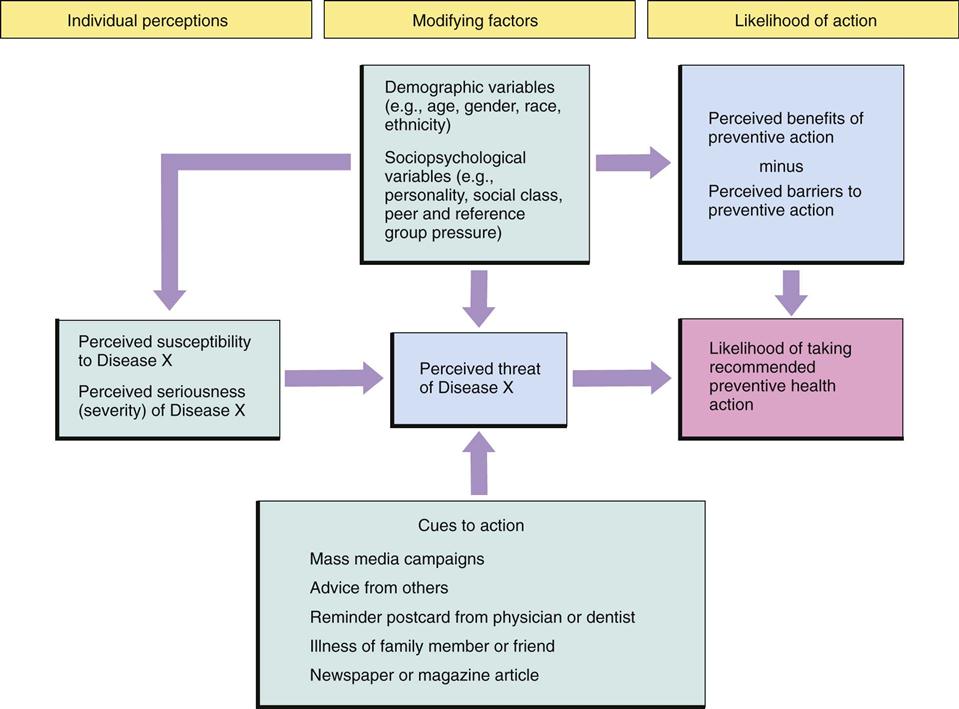
Rosenstoch’s (1974) and Becker and Maiman’s (1975) health belief model (Fig. 6-1) addresses the relationship between a person’s beliefs and behaviors. The health belief model helps you understand factors influencing patients’ perceptions, beliefs, and behavior to plan care that will most effectively assist patients in maintaining or restoring health and preventing illness (Box 6-1).
The first component of this model involves an individual’s perception of susceptibility to an illness. For example, a patient needs to recognize the familial link for coronary artery disease. After this link is recognized, particularly when one parent and two siblings have died in their fourth decade from myocardial infarction, the patient may perceive the personal risk of heart disease.
The second component is an individual’s perception of the seriousness of the illness. This perception is influenced and modified by demographic and sociopsychological variables, perceived threats of the illness, and cues to action (e.g., mass media campaigns and advice from family, friends, and medical professionals). For example, a patient may not perceive his heart disease to be serious, which may affect the way he takes care of himself.
The third component—the likelihood that a person will take preventive action—results from a person’s perception of the benefits of and barriers to taking action. Preventive actions include lifestyle changes, increased adherence to medical therapies, or a search for medical advice or treatment. A patient’s perception of susceptibility to disease and his or her perception of the seriousness of an illness help to determine the likelihood that the patient will or will not partake in healthy behaviors.
Health Promotion Model
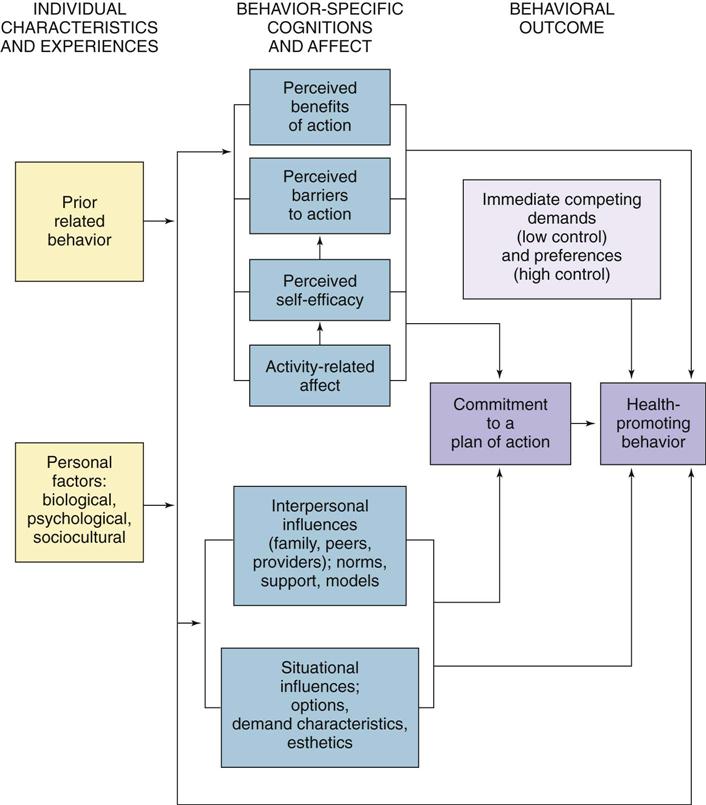
The health promotion model (HPM) proposed by Pender (1982; revised, 1996) was designed to be a “complementary counterpart to models of health protection” (Fig. 6-2). It defines health as a positive, dynamic state, not merely the absence of disease (Pender, Murdaugh, and Parsons, 2011). Health promotion is directed at increasing a patient’s level of well-being. The HPM describes the multidimensional nature of persons as they interact within their environment to pursue health (Pender, 1996; Pender, Murdaugh, and Parsons, 2011). The model focuses on the following three areas: (1) individual characteristics and experiences, (2) behavior-specific knowledge and affect, and (3) behavioral outcomes. The HPM notes that each person has unique personal characteristics and experiences that affect subsequent actions. The set of variables for behavioral-specific knowledge and affect have important motivational significance. These variables can be modified through nursing actions. Health-promoting behavior is the desired behavioral outcome and is the end point in the HPM. Health-promoting behaviors result in improved health, enhanced functional ability, and better quality of life at all stages of development (Pender, Murdaugh, and Parsons, 2011) (Box 6-2).
Maslow’s Hierarchy of Needs
Basic human needs are elements that are necessary for human survival and health (e.g., food, water, safety, and love). Although each person has other unique needs, all people share the basic human needs, and the extent to which basic needs are met is a major factor in determining a person’s level of health.
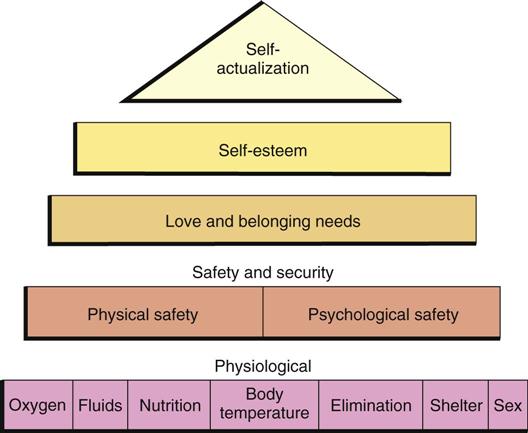
Maslow’s hierarchy of needs is a model that nurses use to understand the interrelationships of basic human needs (Fig. 6-3). According to this model, certain human needs are more basic than others (i.e., some needs must be met before other needs [e.g., fulfilling the physiological needs before the needs of love and belonging]). Self-actualization is the highest expression of one’s individual potential and allows for continual discovery of self. Maslow’s model takes into account individual experiences, always unique to the individual (Ebersole et al., 2008).
The hierarchy of needs model provides a basis for nurses to care for patients of all ages in all health settings. However, when applying the model, the focus of care is on the patient’s needs rather than on strict adherence to the hierarchy. It is unrealistic to always expect a patient’s basic needs to occur in the fixed hierarchical order. In all cases an emergent physiological need takes precedence over a higher-level need. In other situations a psychological or physical safety need takes priority. For example, in a house fire fear of injury and death takes priority over self-esteem issues. Although it would seem that a patient who has just had surgery might have the strongest need for pain control in the psychosocial area, if the patient just had a mastectomy, her main need may be in the areas of love, belonging, and self-esteem. It is important not to assume the patient’s needs just because other patients reacted in a certain way. Maslow’s hierarchy can be very useful when applied to each patient individually. To provide the most effective care, you need to understand the relationships of different needs and the factors that determine the priorities for each patient.
Holistic Health Models
Health care has begun to take a more holistic view of health by considering emotional and spiritual well-being and other dimensions of an individual as important aspects of physical wellness. The holistic health model of nursing attempts to create conditions that promote optimal health. In this model, nurses using the nursing process consider patients to be the ultimate experts concerning their own health and respect patients’ subjective experience as relevant in maintaining health or assisting in healing. In the holistic health model patients are involved in their healing process, thereby assuming some responsibility for health maintenance (Edelman and Mandle, 2010).
Nurses using the holistic nursing model recognize the natural healing abilities of the body and incorporate complementary and alternative interventions such as music therapy, reminiscence, relaxation therapy, therapeutic touch, and guided imagery because they are effective, economical, noninvasive, nonpharmacological complements to traditional medical care (see Chapter 32). These holistic strategies, which can be used in all stages of health and illness, are integral in the expanding role of nursing.
Nurses use holistic therapies either alone or in conjunction with conventional medicine. For example, they use reminiscence in the geriatric population to help relieve anxiety for a patient dealing with memory loss or for a cancer patient dealing with the difficult side effects of chemotherapy. Music therapy in the operating room creates a soothing environment. Relaxation therapy is frequently useful to distract a patient during a painful procedure such as a dressing change. Breathing exercises are commonly taught to help patients deal with the pain associated with labor and delivery.
Variables Influencing Health and Health Beliefs and Practices
Many variables influence a patient’s health beliefs and practices. Internal and external variables influence how a person thinks and acts. As previously stated, health beliefs usually influence health behavior or health practices and likewise positively or negatively affect a patient’s level of health. Therefore understanding the effects of these variables allows you to plan and deliver individualized care.
Internal Variables
Internal variables include a person’s developmental stage, intellectual background, perception of functioning, and emotional and spiritual factors.
Developmental Stage
A person’s thought and behavior patterns change throughout life. The nurse considers the patient’s level of growth and development when using his or her health beliefs and practices as a basis for planning care. The study of development involves finding patterns or general principles that apply to most people most of the time (Murray et al., 2008). The concept of illness for a child, adolescent, or adult depends on the individual’s developmental stage. Fear and anxiety are common among ill children, especially if thoughts about illness, hospitalization, or procedures are based on lack of information or lack of clarity of information. Emotional development may also influence personal beliefs about health-related matters. For example, you use different techniques for teaching about contraception to an adolescent than you use for an adult. Knowledge of the stages of growth and development helps predict the patient’s response to the present illness or the threat of future illness. Adapt the planning of nursing care to these expectations and to the patient’s abilities to participate in self-care.
Intellectual Background
A person’s beliefs about health are shaped in part by the person’s knowledge, lack of knowledge, or incorrect information about body functions and illnesses, educational background, and past experiences. These variables influence how a patient thinks about health. In addition, cognitive abilities shape the way a person thinks, including the ability to understand factors involved in illness and apply knowledge of health and illness to personal health practices. Cognitive abilities also relate to a person’s developmental stage. A nurse considers intellectual background so these variables can be incorporated into nursing care (Edelman and Mandle, 2010).
Perception of Functioning
The way people perceive their physical functioning affects health beliefs and practices. When you assess a patient’s level of health, gather subjective data about the way the patient perceives physical functioning such as level of fatigue, shortness of breath, or pain. Then obtain objective data about actual functioning such as blood pressure, height measurements, and lung sound assessment. This information allows you to more successfully plan and implement individualized care.
Emotional Factors
The patient’s degree of stress, depression, or fear can influence health beliefs and practices. The manner in which a person handles stress throughout each phase of life influences the way he or she reacts to illness. A person who generally is very calm may have little emotional response during illness, whereas an individual unable to cope emotionally with the threat of illness may either overreact to it and assume that it is life threatening or deny the presence of symptoms and not take therapeutic action (see Chapter 37).
Spiritual Factors
Spirituality is reflected in how a person lives his or her life, including the values and beliefs exercised, the relationships established with family and friends, and the ability to find hope and meaning in life. Spirituality serves as an integrating theme in people’s lives (see Chapter 35). Religious practices are one way that people exercise spirituality. Some religions restrict the use of certain forms of medical treatment. You need to understand patients’ spiritual dimensions to involve patients effectively in nursing care.
External Variables
External variables influencing a person’s health beliefs and practices include family practices, socioeconomic factors, and cultural background.
Family Practices
The way that patients’ families use health care services generally affects their health practices. Their perceptions of the seriousness of diseases and their history of preventive care behaviors (or lack of them) influence how patients think about health. For example, if a young woman’s mother never had annual gynecological examinations or Papanicolaou (Pap) smears, it is unlikely that the daughter will have annual Pap smears.
Socioeconomic Factors
Social and psychosocial factors increase the risk for illness and influence the way that a person defines and reacts to illness. Psychosocial variables include the stability of the person’s marital or intimate relationship, lifestyle habits, and occupational environment. A person generally seeks approval and support from social networks (neighbors, peers, and co-workers), and this desire for approval and support affects health beliefs and practices.
Social variables partly determine how the health care system provides medical care. The organization of the health care system determines how patients can obtain care, the treatment method, the economic cost to the patient, and potential reimbursement to the health care agency or patient.
Like social variables, economic variables often affect a patient’s level of health by increasing the risk for disease and influencing how or at what point the patient enters the health care system. A person’s compliance with a treatment designed to maintain or improve health is also affected by economic status. A person who has high utility bills, a large family, and a low income tends to give a higher priority to food and shelter than to costly drugs or treatment or expensive foods for special diets. Some patients decide to take medications every other day rather than every day as prescribed to save money, which greatly affects the effectiveness of the medications.
Cultural Background
Cultural background influences beliefs, values, and customs. It influences the approach to the health care system, personal health practices, and the nurse-patient relationship. Cultural background also influences an individual’s beliefs about causes of illness and remedies or practices to restore health (Box 6-3). If you are not aware of your own cultural patterns of behavior and language, you will have difficulty recognizing and understanding your patient’s behaviors and beliefs. You will also probably have difficulty interacting with patients. As with family and socioeconomic variables, you need to incorporate cultural variables into a patient’s care plan (see Chapter 9).