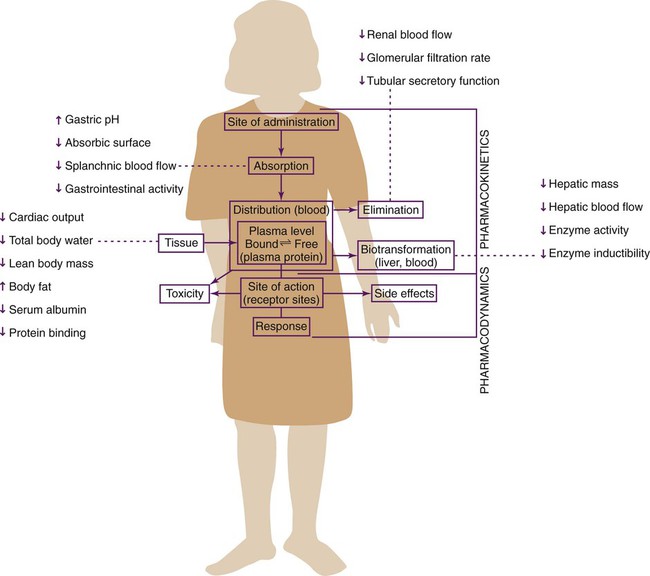
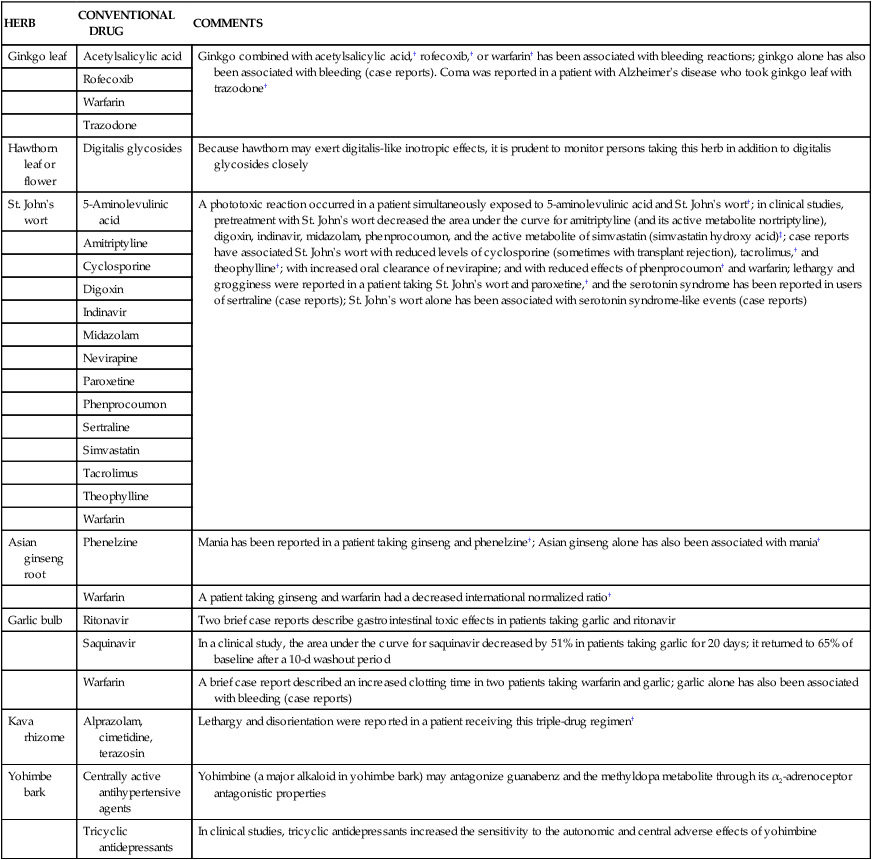
On completion of this chapter, the reader will be able to: 1. Describe the pharmacokinetic changes that occur as a result of normal changes with aging. 2. Describe potential problems associated with drug therapy in late life. 3. Identify medications that are more commonly used in late life. 4. Describe medications and side effects of those more commonly used as psychotherapeutic agents. 5. Identify inappropriate drug use and its application in gerontological nursing. 6. Identify the early signs of adverse drug reactions and strategies to prevent these. 7. Discuss barriers to medication adherence in elders. 8. Discuss the role of the health care professional in assisting elders with adherence to medication regimens. 9. Develop a nursing plan to promote safe medication practices and prevent drug toxicity. Special thanks to Gregory Gulick, MD, who contributed to this chapter in a previous edition. In the United States, persons 65 years of age and older are the largest users of prescription and over-the-counter (OTC) medications. Although making up only about 12% of the population, they consume about one third of all prescriptions drugs and one half of those available OTC (Beyth and Shorr, 2007). The majority (94%) regularly takes prescription medications, 46% take OTCs, and 53% take dietary supplements such as herbs (Qato et al., 2008). Although the statistics vary from study to study, the increase in number of medications with the number of years lived, and chronic conditions acquired, is consistent. The most commonly prescribed and used drugs in the ambulatory older population are cardiovascular drugs, diuretics, nonopioid analgesics, anticoagulants, and antiepileptics (Field et al., 2004). Gastrointestinal preparations and analgesics are the most-used OTC medications, followed by cough products, eye washes, and vitamins. According to a report of the Agency for Healthcare Research and Quality, Medicare beneficiaries spent about $82 billion in 2007 on medications, one fourth of this or about $19 billion, on those for cholesterol and diabetes (Agency for Healthcare Quality Research, 2010). Pharmacokinetics is the study of the movement and action of a drug in the body. Pharmacokinetics determines the concentration of drugs in the body, which in turn determines effect. The concentration of the drug at different times depends on how the drug is taken into the body (absorption), where the drug is dispersed (distribution), how the drug is broken down (metabolism), and how the body gets rid of the drug (excretion). It is important for the gerontological nurse to understand how pharmacokinetics may differ in an older adult (Figure 9-1). There does not seem to be conclusive evidence that absorption in older adults is changed appreciably. However, we do know that diminished salivary secretion and esophageal motility may interfere with swallowing some medications, which could in turn lead to erosions if adequate fluids are not taken with the medications (Gore and Mouzon, 2006). Decreased gastric acid, common in the elderly, will retard the action of acid-dependent drugs. Delayed stomach emptying may diminish or negate the effectiveness of short-lived drugs that could become inactivated before reaching the small intestine. Some enteric-coated medications, such as enteric-coated aspirin, which are specifically meant to bypass stomach acidity, may be delayed so long in older adults that their action begins in the stomach and may produce undesirable effects, such as gastric irritation or nausea. Lipophilic (fat-soluble) drugs pass through capillary membranes more easily than do hydrophilic (water-soluble) drugs, resulting in more rapid tissue distribution and a greater volume of distribution. Lipophilic drugs concentrate in adipose tissue to a greater extent than in the vasculature or other tissues. As adipose tissue nearly doubles in healthy older men and increases by one half in older women, the risk for accumulation and potentially fatal overdoses is increased. Drugs that are highly lipid soluble are stored in the fatty tissue, thus extending and possibly increasing the drug effect, depending on the level of adiposity (Masoro and Austed, 2003). In contrast, decreased body water in normal aging leads to higher serum levels of water-soluble drugs, such as digoxin, ethanol, and aminoglycosides. This can result in a higher relative volume of lipophilic drugs (e.g., diazepam, lorazepam) and a decreased relative volume of hydrophilic drugs (e.g., cimetidine, morphine) (Burchum, 2011). The healthy elder shows either no or only an insignificant change in plasma binding proteins. However, albumin may be significantly reduced in those with malnutrition, an acute illness, or a long-standing chronic condition, common among those in need of skilled care at home or in long-term care settings. Unpredictable concentrations of drug are especially dangerous in those with narrow therapeutic windows such as salicylates, lorazepam, diazepam, chlorpromazine, phenobarbital, or haloperidol. Basic drugs (e.g., lidocaine, propranolol) will show increased protein binding and less effect, and acidic drugs (e.g., warfarin, phenytoin) will show decreased protein binding and greater effect because of decreased plasma albumin (Burchum, 2011). This is especially relevant to nurses working with medically fragile elders, such as in the acute care setting. Metabolism occurs in two phases—phase I (oxidative) and phase II (conjugative). Conjugation reactions primarily convert drugs and their metabolites to glucuronides. Glucuronides are very hydrophilic and are more readily excreted in the urine or bile. The oxidative metabolizing enzymes are known as the cytochrome P450 (CYP450) monooxygenase system. The human CYP450 system is composed of about 50 isoforms (e.g., CYP3A3/4), each of which can perform a specific chemical reaction (Wilkinson, 2001). These isoforms metabolize the parent compound by adding or subtracting a part of the drug molecule (e.g., adding an oxygen atom or subtracting a methyl group), thereby changing the molecule into a more hydrophilic (polar) compound. Eight to ten of these isoforms are responsible for the majority of all drug metabolism. Several of the metabolizing enzymes (CYP450 isoforms) show genetic differences. It has been found that people from different global regions tend to metabolize at different levels of efficiency: there are poor metabolizers, normal metabolizers, rapid metabolizers, and ultrarapid metabolizers (Box 9-1). Although differences in metabolism are important with any class of drugs, they are of particular note in relation to psychotropic and pain medications addressed elsewhere in this chapter. Because of the high level of variability in metabolism from individual to individual, it is difficult to ascribe decreased drug-metabolizing capability to increased age. Studies have shown no decrease in either conjugative metabolism or CYP450 system function as a result of age. However, with aging, liver activity, mass, and volume and blood flow are diminished, with resultant decreases in hepatic exposure. Drugs that do not undergo significant first-pass metabolism are not affected by the aging liver, but those that undergo extensive first-pass metabolism may exhibit decreased metabolism, increased bioavailability, and a decreased rate of biotransformation (Beyth and Shorr, 2007). Renal drug excretion occurs when the drug passes through the kidneys; it involves glomerular filtration, active tubular secretion, and passive tubular reabsorption. Glomerular filtration depends on both the rate and the extent of protein binding of the drug. The process involves passive filtration, and only unbound drugs are filtered. Because kidney function declines in many older persons, so does the ability to excrete or eliminate drugs in a timely manner. The glomerular filtration rate, renal plasma flow, tubular function, and reabsorptive capacity decline. The significantly decreased glomerular filtration rate leads to prolongation of the half-life of drugs eliminated through the renal system, resulting in more opportunities for accumulation and potential toxicity or other adverse events. Although renal function cannot be estimated on the basis of the serum creatinine level, it can be approximated by calculating creatinine clearance. There are a number of online ways to calculate creatinine clearance (e.g., see Chapter 8 or http://www.nephron.com/cgi-bin/CGSIdefault.cgi). The doses of many drugs eliminated through the renal system are based on the patient’s measured or estimated creatinine clearance. Reductions in dosages for drugs eliminated through the renal system (e.g., allopurinol, vancomycin) are needed when the creatinine clearance is reduced (see also Chapter 4). The older a person gets, the more likely he or she will have altered and unreliable pharmacodynamics. Although it is not always possible to explain or predict the alteration, several are known. Those of special note in the elderly are related to drugs with anticholinergic side effects (Box 9-2), which significantly increase the risk for accidental injury and associated with geriatric syndromes. Baroreceptor reflex responses decrease with age. This causes increased susceptibility to positional changes (orthostatic hypotension) and volume changes (dehydration). Age-related increases in sympathetic nervous system activity occur as a result of decreased myocardial sensitivity to catecholamines (e.g., norepinephrine, epinephrine) (Hämmerlein et al., 1998). A decreased responsiveness of the α-adrenergic system results in decreased sensitivity to β-agonists and β-antagonists (β-blockers). Because of the decreased effectiveness of β-blockers and increased sensitivity to diuretics, thiazide diuretics and not β-blockers are recommended for first-line treatment of hypertension in the elderly (Beyth and Shorr, 2007). Polypharmacy has been defined in many ways: as simply the use of multiple medications, or as the use of multiple medications for the same problem (Planton and Edlund, 2010). Either way, it is extremely common among older adults and a source of potential morbidity and mortality. Steinman and Hanlon (2010) reported that nearly 20% of community-living adults at least 65 years of age took 10 or more medications, and this number is significantly higher among those living in long-term care settings. In a study of 1002 disabled older women living in the community, 60% were taking at least 5 different medications and almost 12% were taking at least 10, when OTCs and prescription medications were combined (Crentsil et al., 2010). Simple polypharmacy may be necessary if the patient has multiple chronic conditions, even if the provider is following evidence-based guidelines, and especially when no “double-dipping” of medications is possible. Or it may occur unintentionally, especially if an existing drug regimen is not considered when new prescriptions are given, or any number of the thousands of OTC preparations and supplements are added to those prescribed. Polypharmacy is exacerbated by the combination of a high use of specialists and a reluctance of prescribers to discontinue potentially unnecessary drugs that have been prescribed by someone else; therefore treatments are continued longer than necessary (Randall and Bruno, 2006). When communication between patients, nurses, and other health care providers and caregivers becomes fragmented the risk for duplicative medications, inappropriate medications, potentially unsafe dosages, and potentially preventable interactions is accentuated. The two major concerns with polypharmacy are the increased risk for drug interactions and the increased risk for adverse events. As the popularity of medicinal herbs and other dietary supplements rises, so does the risk for interaction with prescribed medications and other treatments. Although much remains unknown, new knowledge is added almost daily from which the gerontological nurse bases her or his practice. For example, although St. John’s wort has been found to have some therapeutic effect on mild to moderate depression, it also may decrease digoxin levels (Scott and Elmer, 2002). Taking warfarin (Coumadin) at the same time as Ginkgo biloba may artificially increase the international normalized ratio (INR) and lead to inappropriate and potentially dangerous dosing (Valli and Giardina, 2002). These interactions represent only a small fraction of the many real and potential nutritional supplement–drug interactions. Because of inadequate labeling requirements, drug interactions may not be listed on the product labels of these supplements. Patients, prescribers, and nurses administering medications need to be aware of the potential interactions of the herbal preparation or nutritional supplement used to the extent possible (Table 9-1) (see also Chapter 10). TABLE 9-1 POTENTIAL INTERACTIONS BETWEEN HERBS AND CONVENTIONAL DRUGS* *The full version of this table is available from the National Auxiliary Publications Service (NAPS). (See NAPS document no. 05609 for 33 pages of supplementary material. To order, contact NAPS, c/o Microfiche Publications, 248 Hempstead Turnpike, West Hempstead, NY 11552.) Interactions associated with multiple herb therapies are not included. Case reports do not always provide adequate evidence that the remedy in question was labeled correctly. As a result, it is possible that some of the interactions reported for a specific herb were actually due to a different, unidentified botanical or to another adulterant or contaminant. †A single case was reported without reference to previous cases. ‡With the exception of phenprocoumon, these drugs are all substrates for cytochrome P450 3A, P-glycoprotein, or both. From de Smet PA: Herbal remedies, New England Journal of Medicine 347:2048, 2002. Foods may interact with drugs, producing increased, decreased, or variable effects. Foods can bind to drugs, affecting their absorption. For example, calcium in dairy products will bind levothyroxine, tetracycline, and ciprofloxacin, greatly decreasing their absorption; lovastatin absorption is increased by a high-fat, low-fiber meal. Grapefruit juice contains substances that inhibit CYP3A4-mediated metabolism in the gut (Byrd and Luther, 2010). Blood levels of amiodarone, lovastatin, simvastatin, and buspirone are greatly increased when the drugs are taken on the same day as grapefruit (Greenblatt et al., 2001). Certain foods antagonize the therapeutic action of a drug. The vitamin K in leafy green vegetables antagonizes the anticoagulant effects of warfarin (Burchum, 2011) (Table 9-2). It is recommended that patients taking warfarin ingest a consistent amount of greens to avoid variations in coagulability. Spironolactone, prescribed for end-stage heart failure, increases potassium (K+) reabsorption by the renal tubule. If a patient ingests a diet high in potassium (e.g., KCl salt substitute, molasses, oranges, bananas) while taking spironolactone or other potassium-sparing agents, toxic K+ levels can quickly occur. TABLE 9-2 COMMON DRUG–FOOD INTERACTIONS IN OLDER ADULTS From Meiner SE: Gerontologic Nursing, ed 3, St. Louis, MO, 2011, Mosby.
Geropharmacology
![]() http://evolve.elsevier.com/Ebersole/TwdHlthAging
http://evolve.elsevier.com/Ebersole/TwdHlthAging
Pharmacokinetics
Absorption
Distribution
Metabolism
Excretion
Pharmacodynamics
Issues in Medication Use
Polypharmacy
Drug Interactions
Drug–Supplement Interactions
HERB
CONVENTIONAL DRUG
COMMENTS
Ginkgo leaf
Acetylsalicylic acid
Ginkgo combined with acetylsalicylic acid,† rofecoxib,† or warfarin† has been associated with bleeding reactions; ginkgo alone has also been associated with bleeding (case reports). Coma was reported in a patient with Alzheimer’s disease who took ginkgo leaf with trazodone†
Rofecoxib
Warfarin
Trazodone
Hawthorn leaf or flower
Digitalis glycosides
Because hawthorn may exert digitalis-like inotropic effects, it is prudent to monitor persons taking this herb in addition to digitalis glycosides closely
St. John’s wort
5-Aminolevulinic acid
A phototoxic reaction occurred in a patient simultaneously exposed to 5-aminolevulinic acid and St. John’s wort†; in clinical studies, pretreatment with St. John’s wort decreased the area under the curve for amitriptyline (and its active metabolite nortriptyline), digoxin, indinavir, midazolam, phenprocoumon, and the active metabolite of simvastatin (simvastatin hydroxy acid)‡; case reports have associated St. John’s wort with reduced levels of cyclosporine (sometimes with transplant rejection), tacrolimus,† and theophylline†; with increased oral clearance of nevirapine; and with reduced effects of phenprocoumon† and warfarin; lethargy and grogginess were reported in a patient taking St. John’s wort and paroxetine,† and the serotonin syndrome has been reported in users of sertraline (case reports); St. John’s wort alone has been associated with serotonin syndrome-like events (case reports)
Amitriptyline
Cyclosporine
Digoxin
Indinavir
Midazolam
Nevirapine
Paroxetine
Phenprocoumon
Sertraline
Simvastatin
Tacrolimus
Theophylline
Warfarin
Asian ginseng root
Phenelzine
Mania has been reported in a patient taking ginseng and phenelzine†; Asian ginseng alone has also been associated with mania†
Warfarin
A patient taking ginseng and warfarin had a decreased international normalized ratio†
Garlic bulb
Ritonavir
Two brief case reports describe gastrointestinal toxic effects in patients taking garlic and ritonavir
Saquinavir
In a clinical study, the area under the curve for saquinavir decreased by 51% in patients taking garlic for 20 days; it returned to 65% of baseline after a 10-d washout period
Warfarin
A brief case report described an increased clotting time in two patients taking warfarin and garlic; garlic alone has also been associated with bleeding (case reports)
Kava rhizome
Alprazolam, cimetidine, terazosin
Lethargy and disorientation were reported in a patient receiving this triple-drug regimen†
Yohimbe bark
Centrally active antihypertensive agents
Yohimbine (a major alkaloid in yohimbe bark) may antagonize guanabenz and the methyldopa metabolite through its α2-adrenoceptor antagonistic properties
Tricyclic antidepressants
In clinical studies, tricyclic antidepressants increased the sensitivity to the autonomic and central adverse effects of yohimbine
Drug–Food Interactions
FOOD
DRUG
POTENTIAL EFFECT
Caffeine
Theophylline
Increased potential for toxicity
Fatty food
Griseofulvin
Increased absorption of drug
Blue cheese
Penicillin
Antagonistic action
Fiber
Digoxin
Absorption of drug into fiber, reducing drug action
Vitamin K foods: cabbage, greens, egg yolk, fish, rice
Warfarin
Decreased effect of drug, inhibiting anticoagulation
Food
Many antibiotics
Reduced absorption rate of drug
Mineral oil
Oil-soluble vitamins
Fat-soluble vitamins dissolve in oil; deficiency possible
Tyramine foods: aged cheese, wines, pickled herring, chocolate
Monoamine oxidase (MAO) inhibitors (phenelzine [Nardil], tranylcypromine [Parnate]), St. John’s wort
May precipitate hypertensive crisis
Vitamin B6 supplements
Levodopa-carbidopa
Reverses antiparkinsonian effect
Grapefruit juice
Cisapride, calcium channel blockers, quinidine
Altered metabolism and elimination can increase concentration of drug
Citrus juice
Calcium channel blockers
Gastric reflux exacerbated
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Geropharmacology
Get Clinical Tree app for offline access