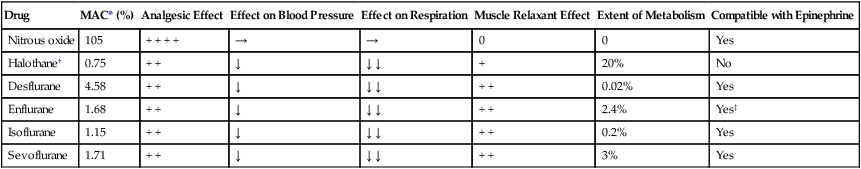
CHAPTER 27 General anesthetics are drugs that produce unconsciousness and a lack of responsiveness to all painful stimuli. In contrast, local anesthetics do not reduce consciousness, and they blunt sensation only in a limited area (see Chapter 26). From a clinical perspective, knowledge of the MAC of an anesthetic is of great practical value: The MAC tells us approximately how much anesthetic the inspired air must contain to produce anesthesia. A low MAC indicates that the inspired air need contain only low concentrations of the anesthetic to produce surgical anesthesia. The opposite is true for drugs with a high MAC. Fortunately, most inhalation anesthetics have low MACs (Table 27–1). However, one important agent—nitrous oxide—has a very high MAC. The MAC is so high, in fact, that surgical anesthesia cannot be achieved using nitrous oxide alone. TABLE 27–1 Properties of the Major Inhalation Anesthetics *Minimum alveolar concentration. †No longer used in the United States and Canada. ‡Enflurane sensitizes the myocardium to catecholamines, but less so than halothane. Malignant hyperthermia is a rare but potentially fatal reaction that can be triggered by all inhalation anesthetics (except nitrous oxide). Predisposition to the reaction is genetic. Malignant hyperthermia is characterized by muscle rigidity and a profound elevation of temperature—sometimes to as high as 43°C (109°F). Left untreated, the reaction can rapidly prove fatal. The risk of malignant hyperthermia is greatest when an inhalation anesthetic is combined with succinylcholine, a neuromuscular blocker that also can trigger the reaction. Diagnosis and management of malignant hyperthermia are discussed in Chapter 16. Clonidine is used for hypertension and pain reduction. When administered prior to surgery, the drug reduces anxiety and causes sedation. In addition, it permits a reduction in anesthetic and analgesic dosages. Analgesic properties of clonidine are discussed further in Chapter 28; antihypertensive properties are discussed in Chapters 19 and 47. The formulation used for analgesia is marketed under the trade name Duraclon; the formulation for hypertension is marketed as Catapres. Dexmedetomidine [Precedex] is a highly selective alpha2-adrenergic agonist currently approved only for short-term sedation in critically ill patients. However, the drug is also used for other purposes, including enhancement of sedation and analgesia in patients undergoing anesthesia. The pharmacology of dexmedetomidine is discussed further in Chapter 28.
General anesthetics
Inhalation anesthetics
Basic pharmacology
Minimum alveolar concentration

Drug
MAC* (%)
Analgesic Effect
Effect on Blood Pressure
Effect on Respiration
Muscle Relaxant Effect
Extent of Metabolism
Compatible with Epinephrine
Nitrous oxide
105
+ + + +
→
→
0
0
Yes
Halothane†
0.75
+ +
↓
↓ ↓
+
20%
No
Desflurane
4.58
+ +
↓
↓ ↓
+ +
0.02%
Yes
Enflurane
1.68
+ +
↓
↓ ↓
+ +
2.4%
Yes‡
Isoflurane
1.15
+ +
↓
↓ ↓
+ +
0.2%
Yes
Sevoflurane
1.71
+ +
↓
↓ ↓
+ +
3%
Yes
Adverse effects
Malignant hyperthermia.
Adjuncts to inhalation anesthesia
Preanesthetic medications
Alpha2-adrenergic agonists.
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


General anesthetics
Only gold members can continue reading. Log In or Register to continue
Get Clinical Tree app for offline access
