Environmental Health Risks
At Home, at Work, and in the Community
Barbara Sattler*
Focus Questions
Key Terms
Body burden
Brownfield
Dose response
Ecology
Environmental health
Environmental justice
Environmental Protection Agency (EPA)
Exposure assessment
Fate and transport
Hazardous waste
Household hazards
Material safety data sheets (MSDS)
Multiple chemical sensitivity (MCS)
National Institute for Occupational Safety and Health (NIOSH)
Occupational Safety and Health Administration (OSHA)
Precautionary Principle
Right to know
Risk communication
Superfund
Toxicology
Volatile organic compounds (VOCs)
Overview of environmental health
Environmental health comprises those aspects of human health, including quality of life, that are determined by physical, chemical, biological, social, and psychological problems in the environment. It also refers to the theory and practice of assessing, correcting, controlling, and preventing those factors in the environment that can potentially affect adversely the health of present and future generations.
In this chapter, the influence of the environment on human health is examined, and the responsibilities of the community health nurse in relation to occupational and environmental health are defined. Understanding the effects of environmental factors on health and disease requires an appreciation of the complex interplay of many factors. Social, cultural, political, economic, and physical forces (chemical, radiological, and biological) interact with the psychological and physiological elements that form the foundation of human existence. In keeping with this assertion, this chapter examines a conceptual model of environmental health and uses this model to present an analysis and overview of factors affecting the connection between the environment and health. It is hoped that the discussion in this chapter will assist the reader in recognizing the environment as an important contributor to the health and well-being of individuals and populations.
Definition of Environmental Health
The Institute of Medicine (IOM) defines environmental health as “freedom from illness or injury related to exposure to toxic agents and other environmental conditions that are potentially detrimental to human health” (IOM, 1995, p. 15). Because of the multifactorial nature of environmental exposures and the myriad potential health effects, it is almost impossible to attribute a disease or health effects to a single exposure. Despite these difficulties, it is essential that health professionals consider the environment in relation to the health of their clients and to understand the nature of risk as it pertains to the environment. Nursing assessments that ignore occupational and environmental risk factors may miss an important clue to a patient’s or a population’s health risks.
All nursing models ask us to consider the environment as a predictor of health. There are many ways in which to frame environmental health, including the following:
It is important to note how we begin to understand the relationship between environmental chemical exposures and their potential for harm. There are several ways in which we have historically made such discoveries, including the following:
However, the most common way in which the relationships between chemical exposures and health risks are determined is when toxicologists study the harmful effects of chemicals on animals and we then estimate what the effects might be on humans. This estimation process is called “extrapolation.” There have been over 100,000 man-made chemical compounds developed and introduced into our environment since World War II; we are most often reliant on the data that are created in animal studies to warn us about their potential toxicity to humans. For many chemicals, no toxicity data are available because toxicological research is not required.
Historical Perspective
Florence Nightingale was a great proponent of clean water and fresh air as key elements in promoting the public’s health. Her practice improved the health of British soldiers in the Crimean War and reduced the high infant death rate in London. Nightingale identified the need for a clean environment with five points: pure air, pure water, efficient drainage (sewage), cleanliness, and light (Nightingale, 1860).
Some of the most significant public health success stories have resulted from eliminating environmental exposures. The greatest strides in the control of widespread disease occurred after the acceptance of the germ theory in the late 19th century (Last, 1998). Such advances in scientific knowledge about the causes of disease led to the development of sewage and water treatment systems, which greatly contributed to the control of some of the worst threats to long life and good health, including typhoid, typhus, and other water-borne diseases (Newsome, 2005). Globally, many of these health concerns persist.
While some of the former health concerns persist, the 20th century brought a whole new set of environmental concerns resulting from climate change, energy production, the unfettered development of chemicals and products, increasing demands by population growth, antibiotic-resistant strains of infectious diseases, and the introduction of new technologies. In our poorest communities, there are additional risks from substandard housing, lack of healthy foods, inadequate access to health care, and higher probability of working in unhealthy jobs.
Nursing Involvement in Environmental Issues
In the 21st century the relationship between the environment and human health will play a significant role in how we assess and address public health and the delivery of health care services. Global climate change creates both ecological changes and threats to human health. The legacy and continued use of hundreds of thousands of potentially toxic chemicals is already affecting our health status. The need for preparedness from natural and man-made disasters is essential. And engagement in the policy arena will be critical to insure that we create laws and regulations that afford the most protection to ecological and human health.
Nursing practice is not currently aligned with the depth and breadth of the current state of environmental health science. It is critical that nurses integrate knowledge from the mounting science regarding the relationship between environmental exposures and human health effects into our education, practice, research, and policy/advocacy work (IOM, 1995). As nurses, we learn to assess, plan, implement, and evaluate. If we do not include environmental health in our assessments (individual, family, and/or community) we will have missed an important opportunity to prevent or address environmentally related health risks and disease.
In 2010, the American Nurses Association (ANA) recognized this critical need and included an Environmental Health Standard in Nursing: Scope and Standards of Practice (ANA, 2010). This ANA document clearly pronounces that environmental health is an essential component for all professional nursing practice. Public health nurses have been proactive in their integration of environmental health, and through the Public Health Nursing Section of the American Public Health Association they adopted a set of environmental principles to guide public health nursing practice (Box 9-1).
There are many ways in which environmental health can be approached from a nursing perspective. We can look at it from a traditional environmental perspective that categorizes exposures by media—air, water, soil, food, products. We can sort by chemical, biological, or radiological exposures. We can examine exposures from the perspective of where we live (home), work, learn (school), and play (community). We can categorize types of chemicals—heavy metals (lead, mercury), pesticides, solvents, etc. Or we can look at human development and see how we are vulnerable to environmental risks during different developmental stages of life—embryonic/fetal, childhood, adult, and older adult. Looking at these different approaches we quickly see that environmental health is complex and wide in scope. In this chapter we will look at environmental health from a variety of approaches.
Today, all nurses are challenged to address environmental problems. The Healthy People 2020 objectives (U.S. Department of Health and Human Services [USDHHS], 2010a) address a great many occupational and environmental health issues (see the Healthy People 2020 box). For example, one objective is to reduce asthma rates, another is to reduce lead poisoning in children, and another is to reduce water-borne illnesses.
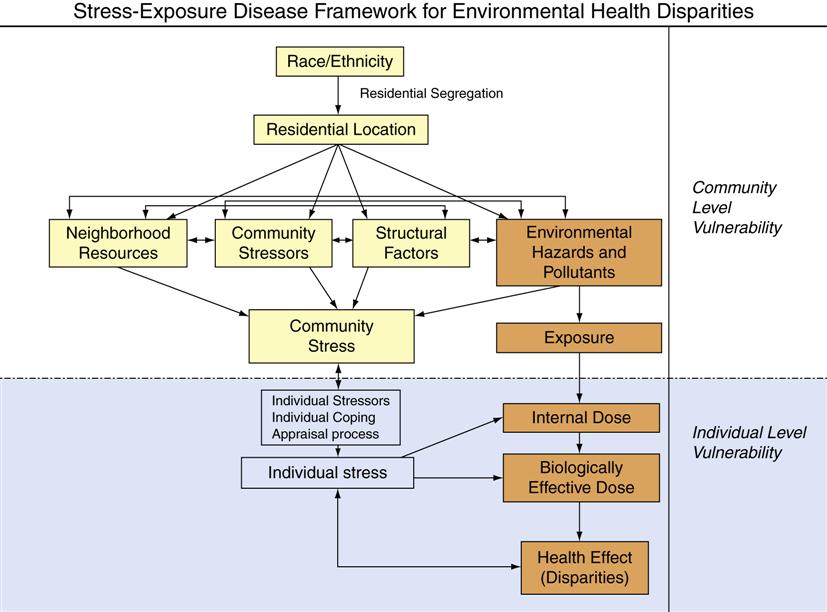
Poverty and race play an important role in health status. The same is true for environmental health status. The concept of environmental justice refers to the disproportionately high exposures of low-income and minority populations to environmental health hazards, such as air pollution, hazardous waste sites, pesticides, lead exposure, and unsafe drinking water (Bullard, 2005; Bullard, 2007; Sattler & Lipscomb, 2003). Such additional exposures further contribute to the health disparities that might otherwise be experienced in poor and stressed communities. Dr. Devon Payne-Sturges of the U.S. Environmental Protection Agency (EPA) has created a useful model to consider the many factors affecting environmental justice and health disparities (Figure 9-1).
Institute of Medicine Report
In the early 1990s, a group of nurses and others were convened by the National Academy of Science Institute of Medicine to assess the integration of environmental health into nursing education, practice, research, and policy/advocacy. The group authored a report in 1995 entitled Nursing, Health, and the Environment (Pope et al., 1995). It continues to serve as a blueprint for efforts to enhance nurses’ capacity to address current and emerging environmental health issues. The following competencies were recognized as essential for all nurses:
All nurses should understand the scientific principles and underpinnings of the relationship between individuals or populations and the environment (including the work environment). This understanding includes the basic mechanism and pathways of exposure to environmental health hazards, basic prevention and control strategies, the interdisciplinary nature of effective interventions, and the role of research.
All nurses should be able to successfully complete an environmental health history, recognize potential environmental hazards and sentinel illnesses, and make appropriate referrals for conditions with probable environmental causes. An essential component is the ability to access and provide information to clients and communities and to locate referral sources.
All nurses should be able to demonstrate knowledge of the role of advocacy (case and class), ethics, and risk communication in client care and community intervention with respect to the potential adverse effects of the environment on health.
All nurses should understand the policy framework and major pieces of legislation and regulations related to environmental health.
In the years since the IOM report, there has been much progress in the nursing profession regarding environmental health.
Multidisciplinary Approaches
Two important scientific disciplines for understanding environmental health are toxicology and epidemiology. Epidemiology is discussed in Chapter 7. Toxicology is the study of chemicals and their potential to make humans (and other life forms) sick. When studying toxic chemicals, scientists work with in vitro (working with cultures or cells) and in vivo models (working with live organisms, such as mice or primates).
While there is no expectation that nurses become toxicologists, it is important for us to know the basic principles of toxicology, as it is a keystone science of environmental health. Table 9-1 contains a side-by-side comparison of a science that is well known to nurses—pharmacology—and the lesser known science of toxicology. We can easily see that toxicology is very similar to pharmacology. Both require an understanding of dose/response and both require us to consider host factors.
Table 9-1
Comparison of Pharmacology and Toxicology
| Pharmacology | Toxicology |
| Pharmacology is the scientific study of the origin, nature, chemistry, effects, and use of drugs. | Toxicology is the science that investigates the adverse effects of chemicals on health. |
| Dose refers to the amount of a drug absorbed from an administration. | Dose refers to the amount of a chemical absorbed into the body from a chemical exposure. |
| A drug can be administered one time, short term, or long term. | Exposure is the actual contact that a person has with a chemical. Exposure can be one time, short term, or long term. |
| A dose-response curve graphically represents the relationship between the dose of a drug and the response elicited. | A dose-response curve describes the relationship of the body’s response to different amounts of an agent such as a drug or toxin. |
| Routes of administration include oral, intramuscular, intravenous, dermal, or topical. | Routes of entry are ingestion, inhalation, or dermal absorption. |
| With drugs there are therapeutic responses (desirable) and side effects (undesirable). Beyond the therapeutic dose, a drug may become toxic. | In toxicology, only the toxic effects are of concern. Toxicity is the ability of a chemical to damage an organ system, disrupt a biochemical process, or disturb an enzyme system. |
| Potency refers to the relative amount of drug required to produce the desired response. | The potency of a toxic chemical refers to the relative amount it takes to elicit a toxic effect compared with other chemicals. |
| Biologic monitoring is done for some drugs: clotting time is monitored in patients taking anticoagulants such as warfarin. Actual drug levels are measured for some drugs such as digoxin. | Biologic monitoring is done for some toxic exposures, such as blood lead levels or metabolites of chemicals such as cotinines for environmental tobacco smoke. |
From Sattler, B. (1998). Environmental Health Education Center, University of Maryland School of Nursing. Used with permission.
Where toxicology and pharmacology differ substantially is in the regulatory arena. Pharmaceuticals are highly regulated from the moment a scientist even considers the development of a drug through its final stages of clinical trials and into the market. For chemicals that are not pharmaceuticals and their associated products (such as personal care products, lawn and pet products, and cleaning solutions) there is virtually no regulatory oversight. We will see later in this chapter how this lack of oversight is impacting human health.
Another area of environmental science that is relevant to environmental health is the study of the fate and transport of chemicals. This refers to the way in which pollutants migrate from one place to another. For example, the mercury released into the air from a coal-fired power plant can wind up in the water, where the microorganisms convert the mercury to organic mercury (which is toxic). These microorganisms are then eaten by larger and larger marine animals, which in turn are eaten by humans. Another example is when potentially toxic agricultural chemicals leach into the ground water, which contaminates wells from which the community draws its drinking water. Understanding fate and transport can help public health nurses to consider the best ways to help communities and individuals avert harmful exposures.
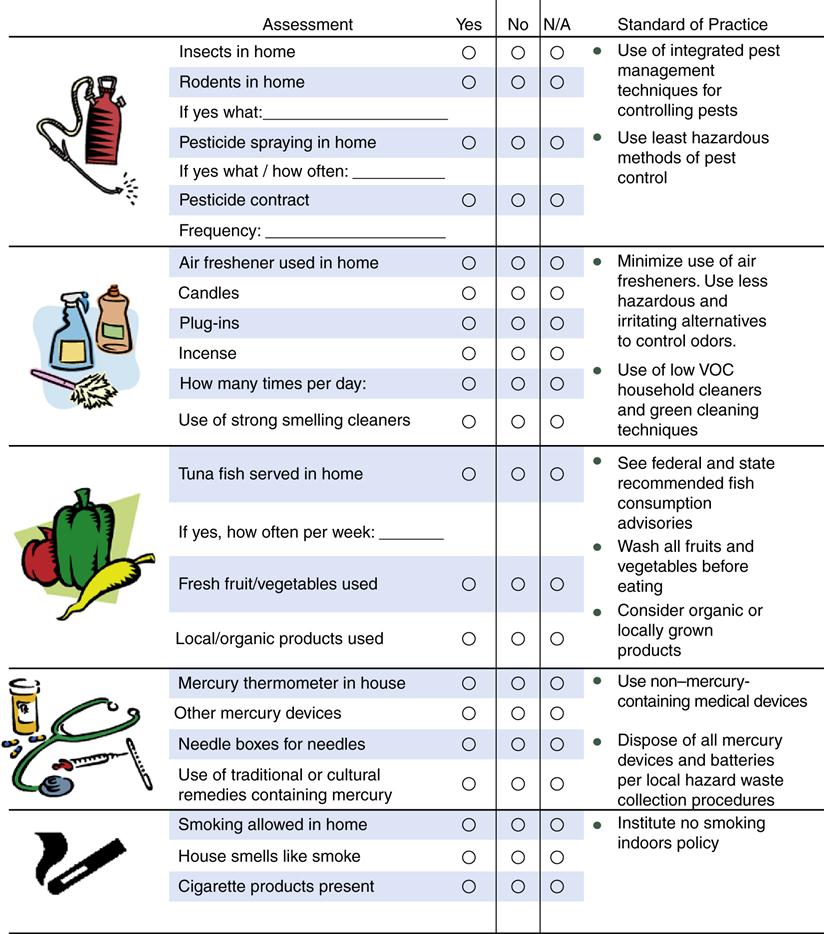
In workplaces, occupationally related exposures are often assessed by industrial hygienists, a group of professionals who measure air quality, noise levels, and temperature in order to determine the level of risk to workers. They address exposures using a tool called the “Industrial Hygiene Hierarchy of Controls” (Figure 9-2). This rubric for decision making is a useful tool for other environmental exposures, in addition to occupational exposures.
In the Industrial Hygiene Hierarchy of Controls, the first line of defense starts with the question: Do we need this toxic chemical (or product) in the first place? Can it be eliminated? The second question is: Is there a safe(r) substitute that could be used? Next, we look at opportunities to modify the workplace with engineering controls such as exhaust hoods that pull potentially toxic fumes up and away from the workers. We also look at ways to completely contain hazards in contained areas. A home-based example of containment is the use of “roach hotels” that have small amounts of pesticides within an enclosed box versus spraying pesticides throughout a whole room. The next defense against toxic chemicals in workplaces is ventilation. Circulating increased volumes of outside air into a workplace dilutes the chemicals inside. Increasing air exchange is often an important activity when addressing indoor air pollution, even in homes and schools. By changing work practices, we can reduce the amount of exposure to any given worker. For example, we can limit the amount of time any given worker has to spend in an area with known toxic exposures. This is done with radiation and is why people who work around x-rays monitor their exposures. When they have reached a certain level of exposure, they can no longer work in the areas where they might continue to be exposed. The final and least effective of the choices is retrofitting the worker with personal protective equipment (PPE) such as gloves, masks, respirators, and protective clothing. When selecting an intervention, the most effective choices are at the top of the hierarchy and they become less effective as you move down the list.
Assessment, prevention, and protection in environmental health are the job of a great many disciplines. Toxicologists, along with a wide array of basic and applied scientists (e.g., geologists, biologists, geographers, neurobiologists) help to provide some of the scientific underpinnings for our understanding of how human health, ecological health, and the environment are all interconnected and impact each other. In the applied arena, there are sanitarians (who are currently renaming themselves “environmental professionals”) who often work in the public sector, especially in local health departments. They are often involved in food safety, vector control, housing-related environmental risks, and other of the environmental programs typically found in local health departments.
In the applied arena there are professionals and technicians who specialize in water quality, air quality, and other media-specific areas. Such specialists may work in the public sector (e.g., state health and environmental departments, the federal Environmental Protection Agency). They may also work in industry and in the nonprofit world, where they help to determine necessary environmental controls or advocate for enhanced environmental protection.
In workplace health settings, occupational health nurses work very closely with industrial hygienists and have some overlapping roles; however, nurses have the distinct role in physical assessments of the workers, maintaining health records, and other human health-specific work. Both occupational health nurses and industrial hygienists are responsible for knowing the laws and regulations regarding workplace health and safety.
Another occupational health specialty is ergonomics, the study of the interface between people and their physical environment. Ergonomists address issues related to work stations and how well they “fit” the worker, in order to reduce or eliminate muscular strain, vision problems, and other stressors.
Nursing’s role has been evolving in terms of our responsibilities in environmental health. In the state of Vermont, every political jurisdiction has an “environmental health nurse” who has been cross-trained beyond general community/public health to a wider range of environmental health issues. In the Los Angeles Health Department, a new role has been created for environmental health nurses. At the University of Maryland Medical Center a role has been created for a nurse (Denise Choiniere, MS, RN) to lead environmental health and sustainability work at the hospital. While these positions are still rare, it indicates a growing understanding of how important nurses’ skills can be harnessed to address environmental health challenges.
More often what we are seeing is the integration of environmental health principles and practices into existing nursing work, particularly public health nursing. For example, it is quite common to have a nurse directing the lead poisoning activities within a health department or to have nurses involved in risk communication, such as when a swimming area is compromised with pathogens. It is equally common to see school nurses involved in indoor air quality issues or concerned about the pesticides that are used on the children’s playing fields.
Conceptual Model of Ecological Systems
Ecology refers to the study of living things in relationship to their environment. The major impetus in the development of ecology was from the biological sciences. As early as 1859, Charles Darwin identified the “web of life” and recognized the highly complex set of interrelationships that were present between organisms and their environments. The word ecology was first used in 1868 by Ernst Haeckel, a German biologist. The term human ecology was coined in the 1920s in a sociological text in an attempt to systematically apply a basic theoretical scheme of plant and animal ecology to the study of human communities (Hawley, 1950). Cultural and sociological dimensions, as well as spatial distribution, were later included in the field of human ecology.
Ecological systems generally have several different levels (Bronfenbrenner, 1979). The simplified version illustrated in Figure 9-3 consists of two levels. The level of system closest to the human population is the microsystem. The microsystem includes the environment immediately surrounding the person (e.g., the family and the home). The macrosystem is the larger context in which the microsystem is embedded. Culture, traditions, customs, societal norms, governmental agencies, schools, organizations, economic policies, and the physical environment constitute the macrosystem.
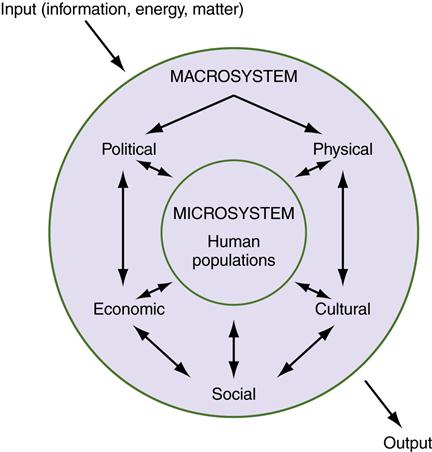
The basic principles of ecological systems are similar to Commoner’s laws of ecology—everything is connected to everything else and everything must go somewhere (Commoner, 1972). Because of the interrelationships and interactions among the different aspects of a system, change in any portion of a system might affect change in other parts of the system. (See Chapter 1 for a discussion of general systems theory.) In other words, systems are dynamic, and change is constant. For example, the microsystem or the family of a daycare worker might become infected with Giardia through an infected child at the daycare center who drank contaminated water when on a hike with the parents. The child was infected with the Giardia organism from the macrosystem (a mountain stream). The organism then crossed the boundaries from the macrosystem to the microsystem (the child in daycare) and infected the worker.
An ecological system includes all the physical, social, cultural, political, and economic conditions that influence the lives of individuals, groups, and communities. As with other areas of nursing, the focus of nurses in environmental health is to promote, maintain, and support health, and specifically to explain how the environment affects well-being (Butterfield, 2002). Kleffel (1996) has proposed that nurses move toward an ecocentric perspective that emphasizes the linkages and interrelationships among global conditions, environmental hazards, and human health. In environmental health, particular attention is given to the identification of both positive and negative factors in the environment that might affect human beings.
Since 1999, the Centers for Disease Control and Prevention (CDC) has been studying the presence of toxic chemicals in the blood and urine of a representative sample of American residents. This is a relatively new addition to the long-standing National Health and Nutrition Exam Study (NHANES) (CDC, 2011a). Approximately 5000 people are selected who have their health history taken, are given a physical exam, and provide urine and blood samples. The concept that everything must go somewhere is alarmingly demonstrated by the amount of toxic chemicals that are being found in our urine and blood. The Fourth National Report on Human Exposure to Environmental Chemicals 2009 summarizes the findings from this and past studies during which time 219 potentially toxic chemicals were examined (CDC, 2011a).
The chemicals that the CDC is measuring do not belong in the human body. They are the result of pollutants and potentially toxic chemicals that are found in our air, water, food, soil, and products. Many of them persist in the environment because they do not break down. For some persistent chemicals the human body does not have an effective physiological excretion mechanism and therefore they accumulate in our bodies. These chemicals include fire retardants, solvents, pesticides, and other potentially toxic substances. The list of health risks that are associated with these chemicals is long and includes neurotoxicity (e.g., learning disabilities, behavioral problems, Parkinsonism), reproductive health problems (e.g., infertility, endometriosis), endocrine disruption, and carcinogenicity.
In the CDC study, three common, toxic chemicals were found in almost everyone they tested. These chemicals include polybrominated diphenyl ethers (PBDE), a fire retardant that is used in textiles, computers/electronics and other products; bisphenol A (BPA), a reproductive toxicant that is found in plastics, cosmetics and other products; and perfluorooctanoic acid (PFOA), a chemical used on nonstick surfaces like frying pans. For women, body burdens of potentially toxic chemicals can be unwittingly shared with the developing fetus, as most of these chemicals cross the placental barrier.
In a 2005 study, scientists assayed the cord blood of newborns to see what potentially hazardous chemicals could be found in the blood that had been circulating in the baby immediately before birth. Many of the same industrial chemicals were found in cord blood (Houlihan et al., 2005). The evidence of our body burden of chemicals is a sign of failed chemical policies and a call to action for all nurses to integrate environmental health and precautionary principles into our professional practice. This will require us to consider how we can integrate primary and secondary prevention into our work. To do this, we will need to integrate environmental health into our individual, family, and community assessments and learn about the resources that are available to all of us. The presence of the Web can catalyze our efforts, as the evidence that we need to underpin our decisions and practice is now often readily available.
Assessment of environmental health hazards
By its very nature, environmental health requires a public health approach to disease because environments affect many people simultaneously. An exposure assessment of the potential environmental hazards should be included in every individual’s health history (Sattler & Lipscomb, 2003). Box 9-2 presents questions that should be part of this assessment. The primary environments for most individuals can be divided into three broad areas: the home (Davis, 2007), the work site (Guenther & Hall, 2007; Sattler, 2003; Sattler & Hall, 2007; Shaner-McRae et al., 2007), and the community (Gilden, 2003). In the sections that follow, these environments are described. Other chapters cover related topics, such as violence (see Chapter 23).
There are a number of environmental assessment tools that can be used to supplement the basic community health assessment in order to identify environmental health threats within a community. On the website http://www.enviRN.org, you can find a number of assessment tools. The National Library of Medicine created ToxTown to help identify and address public and environmental health risks and link the information to their wealth of databases and peer-reviewed articles (http://toxtown.nlm.nih.gov/). Note that ToxTown allows the viewer to choose between a town, city, farm, U.S./Mexico border community, or port, providing a great range of environmental health information. Skin Deep is an excellent database created by the Environmental Working Group that specifies the health risks associated with personal care products (http://www.ewg.org/skindeep/). The Household Products Database created by the National Library of Medicine provides information on the ingredients and potential health effects from products ranging from cleaning, automotive, lawn care, and personal care products to pet supplies (http://hpd.nlm.nih.gov/).
When doing a community-wide assessment, environmental questions to ask are as follows: What is the air quality in the community? What is the water quality (both drinking water and recreational)? Are agricultural and/or lawn chemicals a part of the landscape (e.g., pesticides, herbicides)? Has the land/soil been contaminated by previous or current use? Are pests a problem (e.g., mosquitoes, rodents, deer)? Is the housing stock sound and healthy? Are there major roadways in the community that may contribute to air pollution and particulate matter? Also note that a neighborhood assessment should include the positive environmental attributes that contribute to health and quality of life. Examples of questions about environmental attributes include the following: Is the community “walkable”; is it served by good public transportation; and does it have parks, green spaces, community gardens, and/or trees? Is there access to affordable, healthy foods and fresh produce? Does the community have access to a farmers’ market during the growing season?
Environmental Hazards at Home
While we would like to think of our homes as safe and healthy havens, they may have hidden risks that we can often easily reduce or eliminate. These risks may be associated with the building itself, such as formaldehyde, which is commonly used to bind wood chips in pressboard, or with lead-based paint, commonly found in housing stock build before the 1950s and sometimes found in houses built before 1978, when lead-based paint was banned from use in house paint.
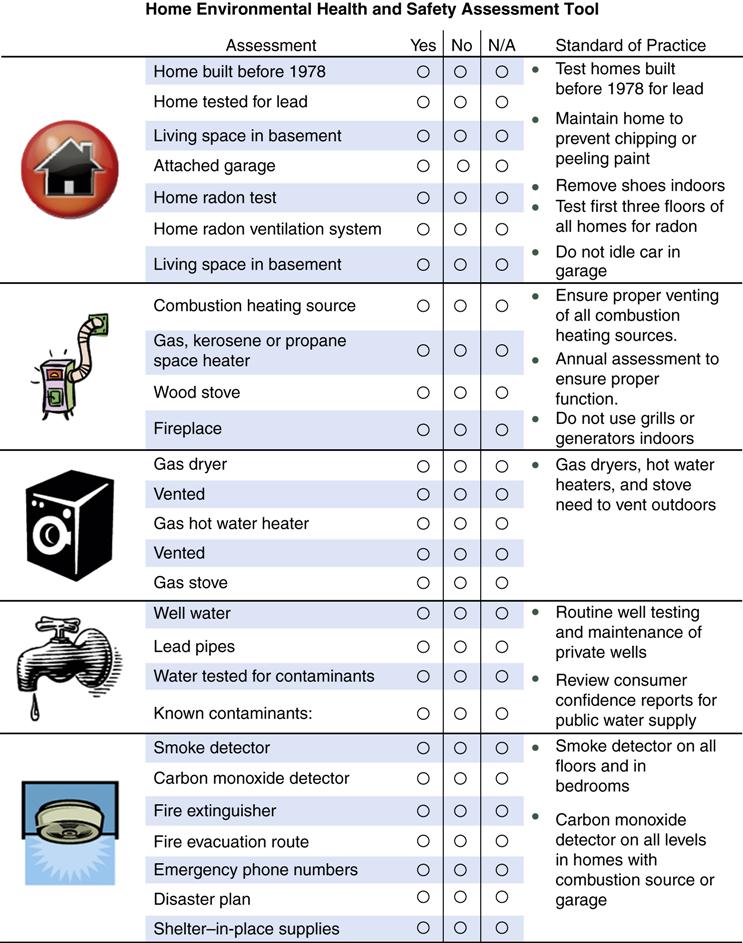
There are many assessment tools that have been developed to determine environmental health risks. Dr. Allison Davis developed a home assessment when she was a graduate nursing student that she used to determine the types of environmental health risks that might be experienced by staff and residents in group homes for people with developmental disabilities (Figure 9-4). This quick and easy assessment tool can help to guide any type of home assessment. Using this tool in combination with the National Library of Medicine’s ToxTown and the Household Products Database will help to determine some of the most common health risks that are associated with most homes. They can help to determine areas for remediation, product substitution, and general environmental health education. Table 9-2 discusses common sources of home pollution.
Table 9-2
Common Sources of Home Pollution
| Agent | Description | Sources in Home |
| Radon | Colorless, odorless, radioactive gas from the natural breakdown (radioactive decay) of uranium; it is estimated that radon causes up to 36,000 lung cancer deaths per year | Soil or rock under the home, well water, building materials |
| Asbestos | Mineral fiber used extensively in building materials for insulation and as a fire retardant; asbestos should be removed by a professional if it has deteriorated; exposure to asbestos fibers can cause irreversible and often fatal lung diseases, including cancer | Sprayed-on acoustical ceilings or textured paint, pipe and furnace insulation materials, floor tiles, automobile brakes and clutches |
| Biological contaminants | Include bacteria, mold and mildew, viruses, animal dander and saliva, dust mites, and pollen; these contaminants can cause infectious diseases or allergic reactions; moisture and dust levels in the home should be kept as low as possible | Mold and mildew, standing water or water-damaged materials, humidifiers, house plants, household pets, ventilation systems, household dust |
| Indoor combustion | Produces harmful gases (carbon monoxide, nitrogen dioxide), particles, and organic compounds (benzene); health effects range from irritation to the eyes, nose, and throat, to lung cancer; ventilation of gas appliances to the outdoors will minimize risks | Tobacco smoke, unvented kerosene or gas space heaters, unvented kitchen gas stoves, wood stoves or fireplaces, leaking exhaust flues from gas furnaces and clothes dryers, car exhaust from an attached garage |
| Household products | Can contain potentially harmful organic compounds; health effects vary greatly; the elimination of household chemicals through the use of nontoxic alternatives or by using only in well-ventilated rooms or outside will minimize risks | Cleaning products; paint supplies; stored fuels; hobby products; personal care products; mothballs; air fresheners; dry-cleaned clothes |
| Formaldehyde | Widely used chemical that is released to the air as a colorless gas; it can cause eye, nose, throat, and respiratory system irritation, headaches, nausea, and fatigue; might be a central nervous system depressant and has been shown to cause cancer in laboratory animals; remove sources of formaldehyde from the home if health effects occur | Particleboard, plywood, and fiberboard in cabinets, furniture, subflooring, and paneling; carpeting, durable-press drapes, other textiles; urea-formaldehyde insulation; glues and adhesives |
| Pesticides | Including insecticides, termiticides, rodenticides, and fungicides, all of which contain organic compounds; exposure to high levels of pesticides might cause damage to the liver and the central nervous system and increase cancer risks; when possible, nonchemical methods of pest control should be used; if the use of pesticides is unavoidable they should be used strictly according to the manufacturer’s directions | Contaminated soil or dust that is tracked in from outside; stored pesticide containers; residue if used inside |
| Lead | A long-recognized harmful environmental pollutant; fetuses, infants, and children are more vulnerable to toxic effects; if the community health nurse suspects that a home has lead paint, it should be tested | Lead-based paint that is peeling, sanded, or burned; automobile exhaust; lead in drinking water; contaminated soil; food contaminated by lead from lead-based ceramic cookware or pottery; lead-related hobbies or occupations; folk remedies |
Hygiene and Sanitation
Hygiene and household cleanliness contribute to the maintenance of family health. Maintaining a clean home and using closed containers for food sources can significantly reduce the risk of insects such as roaches and ants, as well as rodents (mice/rats), thus avoiding the need for pest control measures.
With population increasing, especially in urban areas, the need to manage waste is an important part of environmental health (Morgan, 2003). Daily, each American produces approximately 4.5 pounds of solid waste, such as food scraps and paper (USDHHS, 1998). One objective of Healthy People 2020 is to decrease overall waste and increase recycling. We can decrease our waste by requesting less packaging on our products, buying in bulk when possible, using reusable shopping bags and recycling. In some cities, like San Francisco, there is now curbside pickup of “compostables”—kitchen waste and green waste from the garden. This significantly decreases the overall waste that must be sent to a landfill or waste incinerator. Many cities and counties have regular or periodic collection centers for household hazardous wastes such as batteries and paints, which should never be thrown in the regular garbage. A detailed case study about disposable diaper use is provided in Website Resource 9A.![]() Hazardous wastes are discussed later in this chapter.
Hazardous wastes are discussed later in this chapter.
Radon
Radon (whose chemical initial is Rn) is an odorless, colorless, and tasteless naturally occurring radioactive gas that is the by-product of decaying uranium in the soil. Exposure to radon, which is commonly from home exposures, is second only to smoking as the leading cause of lung cancer in the U.S. (EPA, 2011). Reducing exposure to radon is a Healthy People 2020 objective. Because it comes from the soil, it is most likely to come into the basements of homes, particularly if there are cracks or crevices. If the basement provides living space for family members it is particularly important to test for radon. Inexpensive tests for radon can be found at hardware stores and building supply stores. The EPA provides excellent guidance to homeowners who discover that they have unhealthy levels of radon. Radon can also get into ground water and, in turn, into well water. It is important to include radon in the battery of tests done on well water. Certain parts of the country are more likely to have radon. Maps from the EPA (see Community Resources for Practice) show areas of high concentration.
Lead
The reduction of childhood lead poisoning is one of the most significant public health achievements in recent years. Leaded gasoline and lead-based paint were both banned in the 1970s. In the years following the ban on leaded gasoline there was a dramatic reduction in the average blood lead level of children in the U.S. Lead-based paint continues to be found in most homes built before 1950. While paint surfaces that are well maintained do not create a risk, chipping and peeling paint and paint dust that is created by friction points, such as double hung windows and sills, continue to contribute to the persistent problem of lead poisoning in children. Despite the removal of lead from paint, gasoline, and food cans, lead persists in the paint and plumbing of many older structures, and in contaminated soil (Sanborn et al., 2002). The Centers for Disease Control is now more concerned about the health effects of lower blood lead levels than they were in the past. Scientific evidence shows us that smaller and smaller amounts of lead can contribute to a range of health threats, particularly neurological effects in children.
In early 2012, the Advisory Committee on Childhood Lead Poisoning Prevention (ACCLPP) of the Centers for Disease Control and Prevention (CDC) recommended that the CDC encourage more focus on primary prevention of lead poisoning in children. This is because research in large, diverse populations of children indicates that all levels of lead have unhealthy effects. There is no “safe” level of lead and the effects appear irreversible. Effects at blood lead levels (BLLs) < 10 μg/dL include IQ deficits and “other behavioral domains, particularly attention-related behaviors and academic achievement. New findings suggest that the adverse health effects of BLLs less than 10 μg/dL in children extend beyond cognitive function to include cardiovascular, immunological, and endocrine effects” (ACCLPP, 2012, p. ix).
Therefore, we should not wait until children are exposed to lead. Primary prevention should focus on improving the housing in which children live. One-third of the dwellings in the United States have lead-based paint hazards. “Housing policies to protect children against lead exposure must target the highest risk properties for priority action; ensure that lead-safe practices are followed during renovation, repair and painting of pre-1978 homes; and prohibit lead-based paint hazards, including deteriorated paint, in pre-1978 homes” (ACCLPP, 2012, p. x).
Secondary prevention should be initiated at the “97.5th percentile of NHANES-generated distribution of children 1-5 years old (currently 5 μg/dL)” (ACCLPP, 2012, p. x). Treatment should include lead education, environmental investigations, and medical monitoring. Previously, the recommended treatment level was > 9 μg/dL. Website Resource 9B ![]() provides additional information about symptoms and recommended interventions for the secondary prevention of lead poisoning starting at blood levels greater than 9 μg/dL.
provides additional information about symptoms and recommended interventions for the secondary prevention of lead poisoning starting at blood levels greater than 9 μg/dL.
Some local health departments, particularly in urban settings, have lead poisoning prevention programs. Some states, such as Maryland, have created statewide blood lead registries in order to track childhood and adult lead poisonings and intervene appropriately. Lead poisoning programs are often the domain of public health nurses, either alone or in collaboration with environmental health specialists. Developing targeted lead surveillance and intervention programs in areas with poor children who live in older housing stock has proven to be a successful form of secondary prevention. Because surveillance finds active cases of lead poisoning, instead of preventing the exposures, it is a secondary prevention approach. Nurses working with families must identify those at risk for lead toxicity while educating children, teachers, parents, and other health care providers about how to prevent lead toxicity (Arvidson & Colledge, 1996; Davis, 2007).
Other sources of lead exposure include contaminated soil, airborne particles from industrial and municipal incinerator sources, water from lead pipes, food cooked in ceramic ware with lead glaze, and hobbies such as target shooting, stained glass, and pottery making.
In recent years, lead has been recognized as a hazard when renovating older homes. Unfortunately, families renovating older homes are often unaware that lead poisoning might be a risk (Agency for Toxic Substances and Disease Registry [ATSDR], 1995; Sanborn et al., 2002). Early signs of lead poisoning include disturbances in cognition, behavior, learning, attention span, and growth and development. Colic, constipation, and upper extremity weakness are signs of chronic exposure. Continued high-level exposure can lead to central nervous system symptoms (e.g., encephalopathy) and renal and hematological effects. Such exposures and symptoms can occur in children and also in adults, particularly those who have significant occupational exposures to lead. In such worker exposure situations it is important to make sure that “take home lead” (as would be true with other workplace toxins) is not brought into the home on workers’ clothing and shoes.
Formaldehyde
Formaldehyde is a colorless, flammable gas that has a distinct, pungent odor. Formaldehyde is a common building block for the synthesis of more complex compounds and materials. Worldwide, over 50 million tons of formaldehyde are used annually in a wide range of products, including household products such as carpets, draperies, paper, shampoos, and cosmetics. It is also used in glues for plywood and fiberboard; thus many homes have formaldehyde in their cabinetry and furniture. In 2011 the National Toxicology Program pronounced that formaldehyde is “known to be a human carcinogen” (National Toxicology Program, 2011). The most common acute symptoms associated with exposure to formaldehyde are eye and nose irritation, respiratory symptoms, nausea, headache, and fatigue. Young children can have abdominal complaints. Less toxic products are available and should be recommended when new purchases are being made. If formaldehyde is present, it can be helpful to increase ventilation in a room by increasing air exchange or by opening windows.
Formaldehyde falls into a large category of chemicals called volatile organic compounds (VOCs). These are chemicals that are gases at room temperature. If they are in solution with other chemicals they may escape into the air as a gas. This process is known as outgassing. For people who are highly sensitive to chemicals, VOCs present a particular problem because they can readily outgas from everyday products and become part of the indoor air. There is a subset of the population that is particularly susceptible to chemical exposures even at very low levels. Formaldehyde is but one of the chemicals that some people react to at low doses.
Carbon Monoxide
Carbon monoxide (CO) is a colorless and odorless gas that is a by-product of combustion and can be an insidious, fatal poison. Possible sources are improperly vented furnaces, blocked flues or chimneys, generators, and automobile exhausts, particularly when a garage is attached to a house. Low-level exposure to carbon monoxide can cause dizziness, headache, drowsiness, nausea, or flu-like symptoms. Higher levels can result in unconsciousness and death. Persons who have cardiovascular or respiratory diseases are particularly vulnerable to the effects of carbon monoxide. The activities of smoking tobacco and cooking also produce carbon monoxide. When possible, range hoods with exhaust fans should be used during cooking. As with formaldehyde, there is an increased risk in well-insulated houses. Nurses can recommend that combustion appliances (fueled by gas or oil) be checked annually (dryers, ovens/stoves, as well as furnaces) and that carbon monoxide detectors be installed if combustion appliances are used (Davis, 2007).
Environmental Tobacco Smoke
The health risks associated with tobacco smoke for both the smoker and those in the presence of environmental tobacco smoke (ETS) are well documented. Secondhand tobacco smoke has carcinogenic and toxic agents that are similar to those in mainstream smoke; the EPA classifies tobacco smoke as a carcinogen. Increasingly, state laws are being passed to create smoke-free spaces in health facilities, restaurants, government buildings, and even in bars.
Reducing children’s exposure to ETS continues to be an objective in Healthy People 2020. It is a major contributor to earaches and respiratory tract infections, such as pneumonia, bronchitis, and asthma. ETS is both a cause of asthma and a trigger for asthmatic events among those with a diagnosis of asthma (Goldman, 2000)
.
Implications for Nurses
Community/public health nurses can address environmental health from an educational, practice, research, and/or policy/advocacy approach. For example, from an educational perspective, nurses can provide guidance to their pregnant patients about preparing an environmentally healthy and safe nursery by addressing potential lead-based paint risks, pesticide use, and carbon monoxide exposures, as well as safety issues such as covering electrical outlets. They can also coach patients on product selection such as choosing infant toys that do not contain phthalates or bisphenol A. Such approaches constitute primary prevention measures.
Environmental exposures can be subtle and may require investigative work by the nurse. For example, water contaminants might not produce a visible change in the water, and some chemicals (e.g., carbon monoxide in air) are not easily detectable.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree