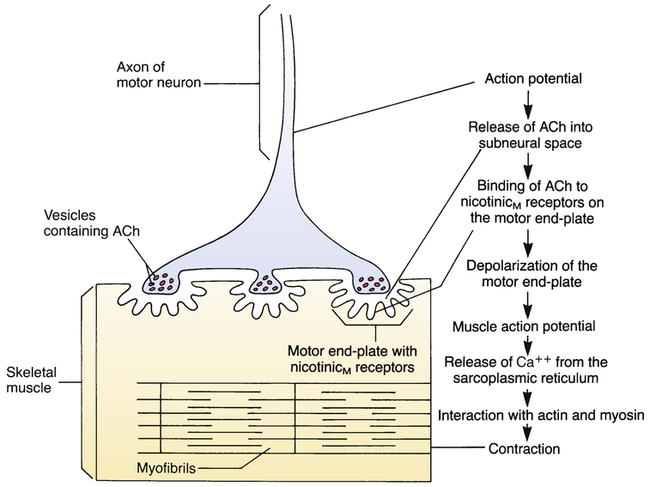
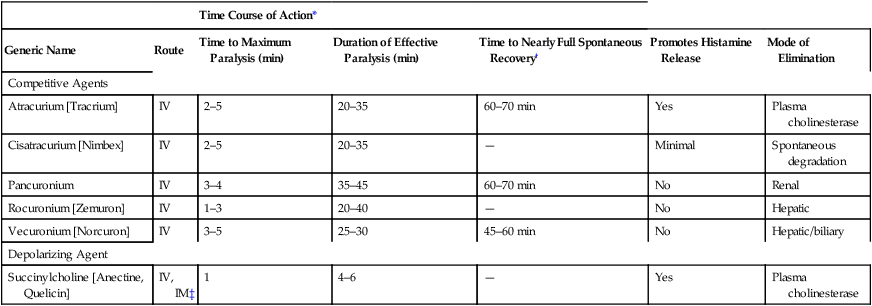
CHAPTER 16 The concepts of polarization, depolarization, and repolarization are important to understanding both muscle contraction and the neuromuscular blocking drugs. In resting muscle there is uneven distribution of electrical charge across the inner and outer surfaces of the cell membrane. As shown in Figure 16–1, positive charges cover the outer surface of the membrane and negative charges cover the inner surface. Because of this uneven charge distribution, the resting membrane is said to be polarized. When the membrane depolarizes, positive charges move from outside to inside. So many positive charges move inward that the inside of the membrane becomes more positive than the outside (see Fig. 16–1). The steps leading to muscle contraction are summarized in Figure 16–2. The process begins with the arrival of an action potential at the terminal of a motor neuron, causing release of acetylcholine (ACh) into the subneural space. Acetylcholine then binds reversibly to nicotinicM receptors on the motor end-plate (a specialized region of the muscle membrane that contains the receptors for ACh) and causes the end-plate to depolarize. This depolarization initiates a muscle action potential (ie, a wave of depolarization that spreads rapidly over the entire muscle membrane), which in turn triggers the release of calcium from the sarcoplasmic reticulum (SR) of the muscle. This calcium permits the interaction of actin and myosin, thereby causing contraction. Very rapidly, ACh dissociates from the motor end-plate, the motor end-plate repolarizes, the muscle membrane repolarizes, and calcium is taken back up into the SR. Because there is no longer any calcium available to support the interaction of actin and myosin, the muscle relaxes. All of the neuromuscular blocking agents contain at least one quaternary nitrogen atom (Fig. 16–3). As a result, these drugs always carry a positive charge, and therefore cannot readily cross membranes. As their name implies, the competitive neuromuscular blockers compete with ACh for binding to nicotinicM receptors on the motor end-plate (Fig. 16–4). However, unlike ACh, these drugs do not cause receptor activation. When they bind to nicotinicM receptors, they block receptor activation by acetylcholine, causing the muscle to relax. Muscle relaxation persists as long as the amount of competitive neuromuscular blocker at the neuromuscular junction (NMJ) is sufficient to prevent receptor occupation by ACh. Muscle function can be restored by eliminating the drug from the body or by increasing the amount of ACh at the NMJ. With the competitive neuromuscular blockers in use today, paralysis develops within minutes of IV injection. Peak effects persist 20 to 45 minutes and then decline. Complete recovery takes about 1 hour. As shown in Table 16–1, the mode of elimination—spontaneous degradation, degradation by plasma cholinesterase, renal excretion, or hepatic metabolism—depends on the agent involved. TABLE 16–1 Properties of Competitive and Depolarizing Neuromuscular Blockers *Time course of action can vary widely with dosage and route of administration. The values presented are for an average adult dose administered as a single IV injection. †Because spontaneous recovery can take a long time, recovery from the competitive agents (all of the drugs listed except succinylcholine, which is a depolarizing agent) is often accelerated by giving a cholinesterase inhibitor. Neuromuscular blocking agents must be used with special care in patients with myasthenia gravis, a condition characterized by skeletal muscle weakness. The cause of weakness is a reduction in the number of nicotinicM receptors on the motor end-plate. Because receptor number is reduced, neuromuscular blockade occurs readily. Also, doses that would have a minimal effect on others can produce complete paralysis in patients with myasthenia. Accordingly, dosing must be done with great care. Myasthenia gravis and its treatment are discussed in Chapter 15.
Drugs that block nicotinic cholinergic transmission: neuromuscular blocking agents and ganglionic blocking agents
Neuromuscular blocking agents
Control of muscle contraction
Basic concepts: polarization, depolarization, and repolarization
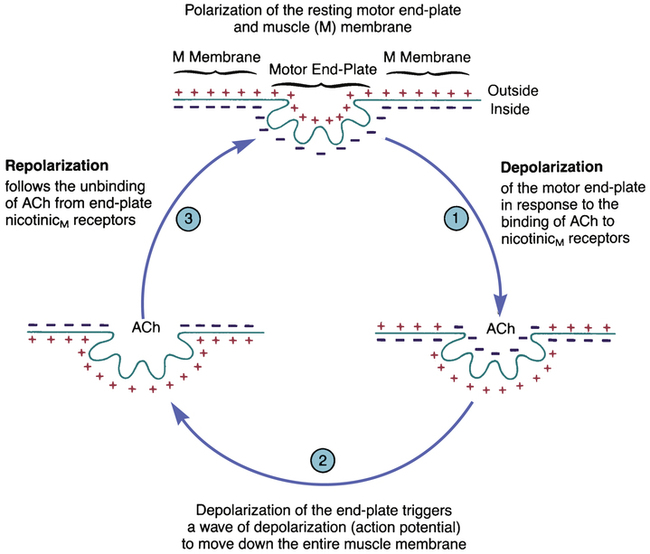
 The depolarization-repolarization cycle of the motor end-plate and muscle membrane.
The depolarization-repolarization cycle of the motor end-plate and muscle membrane.
(ACh = acetylcholine.)
Steps in muscle contraction
Competitive (nondepolarizing) neuromuscular blockers
Group properties
Chemistry
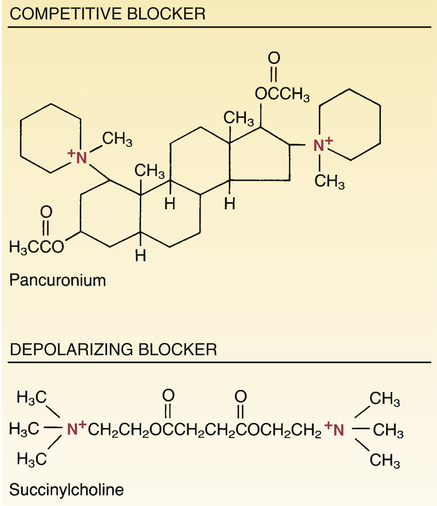
 Structural formulas of representative neuromuscular blocking agents.
Structural formulas of representative neuromuscular blocking agents.
Note that both agents contain a quaternary nitrogen atom and therefore cross membranes poorly. Consequently, they must be administered parenterally and have little effect on the central nervous system or the developing fetus.
Mechanism of action
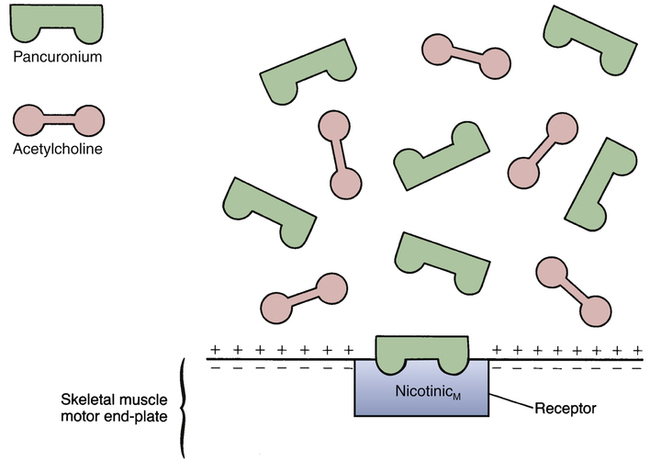
 Mechanism of competitive neuromuscular blockade.
Mechanism of competitive neuromuscular blockade.
Pancuronium, a competitive blocker, competes with acetylcholine (ACh) for binding to nicotinicM receptors on the motor end-plate. Binding of pancuronium does not depolarize the end-plate, and therefore does not cause contraction. At the same time, the presence of pancuronium prevents ACh from binding to the receptor, and hence contraction is prevented.
Pharmacokinetics

Time Course of Action*
Generic Name
Route
Time to Maximum Paralysis (min)
Duration of Effective Paralysis (min)
Time to Nearly Full Spontaneous Recovery†
Promotes Histamine Release
Mode of Elimination
Competitive Agents
Atracurium [Tracrium]
IV
2–5
20–35
60–70 min
Yes
Plasma cholinesterase
Cisatracurium [Nimbex]
IV
2–5
20–35
—
Minimal
Spontaneous degradation
Pancuronium
IV
3–4
35–45
60–70 min
No
Renal
Rocuronium [Zemuron]
IV
1–3
20–40
—
No
Hepatic
Vecuronium [Norcuron]
IV
3–5
25–30
45–60 min
No
Hepatic/biliary
Depolarizing Agent
Succinylcholine [Anectine, Quelicin]
IV, IM‡
1
4–6
—
Yes
Plasma cholinesterase
Precautions and contraindications
Myasthenia gravis.
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Drugs that block nicotinic cholinergic transmission: neuromuscular blocking agents and ganglionic blocking agents
Only gold members can continue reading. Log In or Register to continue
Get Clinical Tree app for offline access