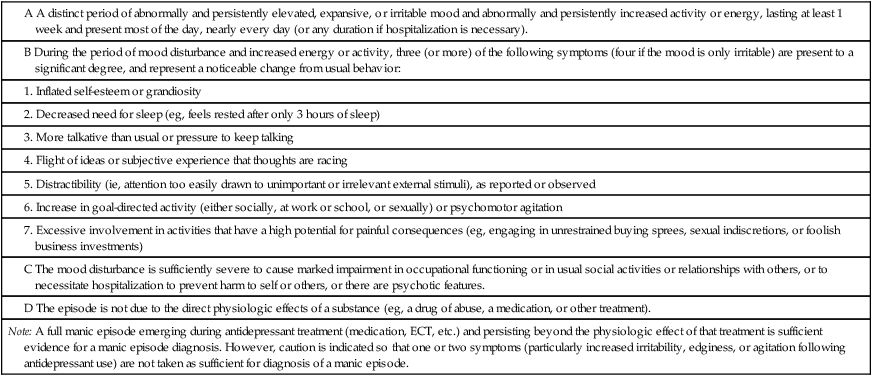
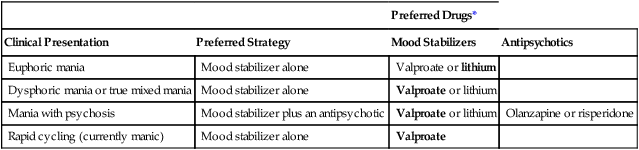
CHAPTER 33 Patients with BPD may experience four types of mood episodes. These are described below. Detailed criteria for a manic episode are set forth in the Diagnostic and Statistical Manual of Mental Disorders (DSM). The criteria now in use, published in the fourth edition of the DSM (DSM-IV), were released in 1994. Revised criteria will appear in fifth edition of the DSM (DSM-5), scheduled for release in 2013. The proposed DSM-5 criteria, which are nearly identical to those in DSM-IV, are summarized in Table 33–1. TABLE 33–1 Proposed DSM-5 Criteria for a Manic Episode Modified from the proposed criteria for a manic episode, to be published in Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Washington, DC: American Psychiatric Association. Expected publication date: May 2013. Copyright © American Psychiatric Association. The proposed criteria are from the DSM-5 web site—www.DSM5.org—accessed on November 20, 2010. A major depressive episode is characterized by depressed mood and loss of pleasure or interest in all or nearly all of one’s usual activities and pastimes. Associated symptoms include disruption of sleeping and eating patterns; difficulty concentrating; feelings of guilt, worthlessness, and helplessness; and thoughts of death and suicide. The characteristics of major depression are discussed further in Chapter 32. Although antidepressants have been studied extensively in patients with major depression, very little research has been done in patients with BPD. As a result, we lack reliable information on which to base drug selection. Even so, experts do have their preferences. Among clinicians with extensive experience in BPD, the following are considered antidepressants of choice: bupropion [Wellbutrin], venlafaxine [Effexor XR], and the selective serotonin reuptake inhibitors (SSRIs), such as fluoxetine [Prozac] and sertraline [Zoloft]. The pharmacology of these drugs is discussed in Chapter 32. Two mood stabilizers—lithium and valproate—are preferred drugs for acute management of manic episodes. The choice between them is based on clinical presentation (eg, euphoric mania, mania with psychosis, rapid-cycling BPD). As shown in Table 33–2, valproate is preferred to lithium in most cases. In fact, the only exception is euphoric mania, for which lithium is the drug of choice. If the patient does not respond adequately to lithium or valproate alone, the drugs may be used together. Responses to mood stabilizers develop slowly, taking 2 or more weeks to become maximal. TABLE 33–2 Initial Treatment of First Manic Episode Valproate = divalproex sodium. *Drugs of choice, if established, are presented in bold type.
Drugs for bipolar disorder
Characteristics of bipolar disorder
Types of mood episodes seen in BPD
Pure manic episode (euphoric mania).

Note: A full manic episode emerging during antidepressant treatment (medication, ECT, etc.) and persisting beyond the physiologic effect of that treatment is sufficient evidence for a manic episode diagnosis. However, caution is indicated so that one or two symptoms (particularly increased irritability, edginess, or agitation following antidepressant use) are not taken as sufficient for diagnosis of a manic episode.
Major depressive episode (depression).
Treatment of bipolar disorder
Drug therapy
Types of drugs employed
Antidepressants.
Drug selection
Acute therapy: manic episodes.

Preferred Drugs*
Clinical Presentation
Preferred Strategy
Mood Stabilizers
Antipsychotics
Euphoric mania
Mood stabilizer alone
Valproate or lithium
Dysphoric mania or true mixed mania
Mood stabilizer alone
Valproate or lithium
Mania with psychosis
Mood stabilizer plus an antipsychotic
Valproate or lithium
Olanzapine or risperidone
Rapid cycling (currently manic)
Mood stabilizer alone
Valproate
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Drugs for bipolar disorder
Only gold members can continue reading. Log In or Register to continue
