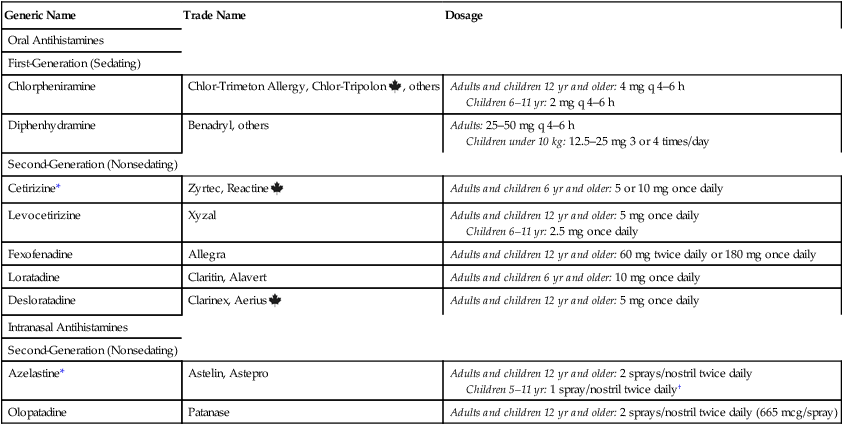
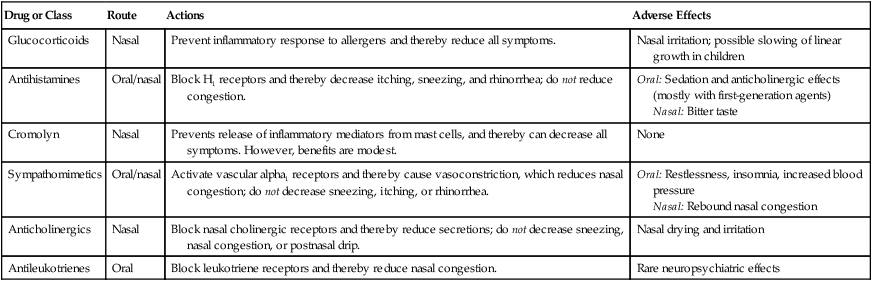
CHAPTER 77 Several classes of drugs are used for allergic rhinitis (Table 77–1). Principal among these are (1) glucocorticoids (intranasal), (2) antihistamines (oral and intranasal), and (3) sympathomimetics (oral and intranasal). Glucocorticoids and antihistamines are considered first-line therapies. Of the two, glucocorticoids are much more effective. Sympathomimetics are used in conjunction with other agents to help relieve nasal congestion. TABLE 77–1 Overview of Drugs for Allergic Rhinitis The basic pharmacology of the glucocorticoids is discussed in Chapter 72. Consideration here is limited to their use in allergic rhinitis. Intranasal glucocorticoids are the most effective drugs for prevention and treatment of seasonal and perennial rhinitis. For patients with mild to moderate rhinitis, glucocorticoids are the initial treatment of choice. With proper use, over 90% of patients respond. Because of their anti-inflammatory actions, these drugs can prevent or suppress all of the major symptoms of allergic rhinitis: congestion, rhinorrhea, sneezing, nasal itching, and erythema. In the past, intranasal steroids were reserved for patients whose symptoms could not be controlled with more traditional drugs (antihistamines, sympathomimetics, intranasal cromolyn). However, because of their proven safety and superior efficacy, glucocorticoids have now replaced the histamine1 (H1) antagonists as the treatment of first choice. Seven glucocorticoids are available (Table 77–2). All appear equally effective. TABLE 77–2 Some Glucocorticoid Nasal Sprays for Allergic Rhinitis Systemic effects are possible, but are rare at recommended doses. Of greatest concern are adrenal suppression and slowing of linear growth in children (whether final adult height is reduced is unknown). Systemic effects are least likely with fluticasone and mometasone, which have very low bioavailability (see Table 77–2). Intranasal glucocorticoids are administered using a metered-dose spray device. Benefits are greatest when dosing is done daily, rather than PRN. Full doses are given initially (see Table 77–2). After symptoms are under control, the dosage should be reduced to the lowest effective amount. For patients with seasonal allergic rhinitis, maximal effects may require a week or more to develop. However, an initial response can be seen within hours. For patients with perennial rhinitis, maximal responses may take 2 to 3 weeks to develop. If nasal passages are blocked, they should be cleared with a topical decongestant prior to glucocorticoid administration. The antihistamines are discussed at length in Chapter 70. Consideration here is limited to their use in allergic rhinitis. Dosages for some popular H1 antagonists are presented in Table 77–3. A more complete list appears in Table 70–2 (Chapter 70). TABLE 77–3 Some Antihistamines for Allergic Rhinitis *May cause some sedation at recommended doses. †Astelin only. Astepro is not approved for children under 12 years.
Drugs for allergic rhinitis, cough, and colds
Drugs for allergic rhinitis

Drug or Class
Route
Actions
Adverse Effects
Glucocorticoids
Nasal
Prevent inflammatory response to allergens and thereby reduce all symptoms.
Nasal irritation; possible slowing of linear growth in children
Antihistamines
Oral/nasal
Block H1 receptors and thereby decrease itching, sneezing, and rhinorrhea; do not reduce congestion.
Oral: Sedation and anticholinergic effects (mostly with first-generation agents)
Nasal: Bitter taste
Cromolyn
Nasal
Prevents release of inflammatory mediators from mast cells, and thereby can decrease all symptoms. However, benefits are modest.
None
Sympathomimetics
Oral/nasal
Activate vascular alpha1 receptors and thereby cause vasoconstriction, which reduces nasal congestion; do not decrease sneezing, itching, or rhinorrhea.
Oral: Restlessness, insomnia, increased blood pressure
Nasal: Rebound nasal congestion
Anticholinergics
Nasal
Block nasal cholinergic receptors and thereby reduce secretions; do not decrease sneezing, nasal congestion, or postnasal drip.
Nasal drying and irritation
Antileukotrienes
Oral
Block leukotriene receptors and thereby reduce nasal congestion.
Rare neuropsychiatric effects
Intranasal glucocorticoids
Actions and uses.

Drug
Trade Name
Intranasal Bioavailability (%)
Dose/Spray (mcg)
Patient Age (yr)
Initial Dosage (Sprays/Nostril)
Beclomethasone
Beconase AQ
44
42
6–11
12 and older
1 twice daily
1 or 2 twice daily
Budesonide
Rhinocort Aqua
34
32
6–11
12 and older
1 or 2 once daily
1–4 once daily
Ciclesonide
Omnaris
—
50
6 and older
2 once daily
Flunisolide
generic only
49
25
6–13
14 and older
2 twice daily or 1 thrice daily
2 twice or thrice daily
Fluticasone propionate
Flonase
0.5–2
50
4–11
12 and older
1 once daily
2 once daily
Fluticasone furoate
Veramyst
—
27.5
2–11
12 and older
1 once daily
2 once daily
Mometasone
Nasonex
0.1
50
2–11
12 and older
1 once daily
2 once daily
Triamcinolone
Nasacort AQ
46
55
6 and older
1 or 2 once daily
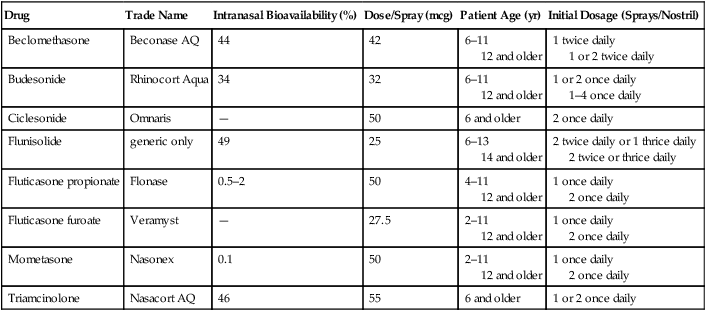
Adverse effects.
Preparations, dosage, and administration.
Antihistamines
Oral antihistamines

Generic Name
Trade Name
Dosage
Oral Antihistamines
First-Generation (Sedating)
Chlorpheniramine
Chlor-Trimeton Allergy, Chlor-Tripolon ![]() , others
, others
Adults and children 12 yr and older: 4 mg q 4–6 h
Children 6–11 yr: 2 mg q 4–6 h
Diphenhydramine
Benadryl, others
Adults: 25–50 mg q 4–6 h
Children under 10 kg: 12.5–25 mg 3 or 4 times/day
Second-Generation (Nonsedating)
Cetirizine*
Zyrtec, Reactine ![]()
Adults and children 6 yr and older: 5 or 10 mg once daily
Levocetirizine
Xyzal
Adults and children 12 yr and older: 5 mg once daily
Children 6–11 yr: 2.5 mg once daily
Fexofenadine
Allegra
Adults and children 12 yr and older: 60 mg twice daily or 180 mg once daily
Loratadine
Claritin, Alavert
Adults and children 6 yr and older: 10 mg once daily
Desloratadine
Clarinex, Aerius ![]()
Adults and children 12 yr and older: 5 mg once daily
Intranasal Antihistamines
Second-Generation (Nonsedating)
Azelastine*
Astelin, Astepro
Adults and children 12 yr and older: 2 sprays/nostril twice daily
Children 5–11 yr: 1 spray/nostril twice daily†
Olopatadine
Patanase
Adults and children 12 yr and older: 2 sprays/nostril twice daily (665 mcg/spray)