Identify the prototype and describe the characteristics, action, use, adverse effects, contraindications, and nursing implications of the tetracyclines.
 Identify the prototype and describe the characteristics, action, use, adverse effects, contraindications, and nursing implications of the sulfonamides.
Identify the prototype and describe the characteristics, action, use, adverse effects, contraindications, and nursing implications of the sulfonamides.
 Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for the adjuvant urinary antiseptic agents used in the treatment of urinary tract infections.
Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for the adjuvant urinary antiseptic agents used in the treatment of urinary tract infections.
 Implement the nursing process in the care of patients being treated with tetracyclines, sulfonamides, or urinary antiseptics.
Implement the nursing process in the care of patients being treated with tetracyclines, sulfonamides, or urinary antiseptics.
Clinical Application Case Study
Sharon Dee is an 18-year-old college student. She comes to the health clinic with complaints of urinary frequency and burning on urination. Her medication history includes ongoing, long-term treatment of acne with a tetracycline. She takes 250 mg of the drug orally daily. The physician diagnoses her with a urinary tract infection and prescribes trimethoprim-sulfamethoxazole (Bactrim) 160/800 mg orally every 12 hours for 10 days.
KEY TERMS
Crystalluria: presence of crystals in the urine, indicating renal irritation
Sulfonamide: older, broad-spectrum, bacteriostatic drug (organic sulfur compounds) that is rarely used for systemic infection because of microbial resistance and the development of more effective or less toxic drugs; also known as sulfa drug
Tetracycline: antibiotic derived from chlortetracycline; used to treat a broad variety of infections
Urinary antiseptic: drug that exerts antimicrobial activity in the urine but has little or no systemic antibacterial effect; usefulness is limited to therapy and prevention of urinary tract infections
Introduction
This chapter introduces the pharmacological care of the patient experiencing an infection that is treated with tetracyclines or sulfonamides. Tetracyclines and sulfonamides are older, broad-spectrum, bacteriostatic drugs that are rarely used for systemic infections because of microbial resistance and the development of more effective or less toxic drugs. This discussion also introduces the urinary antiseptic agents administered for urinary tract infections (UTIs). The Drugs at a Glance tables present information about routes of administration and dosage ranges for both prototypes and other related drugs.
Tetracyclines
The tetracyclines are antibiotics, derived from chlortetracycline, that may be used to treat a broad variety of infections. The drugs in this class have similar pharmacologic properties and antimicrobial activity. Although tetracyclines are effective against both gram-negative and gram-positive microorganisms, they are usually not drugs of choice. Many gram-negative microorganisms have developed resistance to tetracyclines. However, prescribers still order them for bacterial infections caused by Brucella and Vibrio cholerae. The drugs also remain effective against rickettsiae, chlamydia, some protozoa, spirochetes, and others (see “Use” of tetracyclines).  Tetracycline hydrochloride is the prototype of this class.
Tetracycline hydrochloride is the prototype of this class.
Pharmacokinetics
Administration of tetracycline is oral, and the stomach absorbs 75% of the medication. Its peak of action is 2 to 4 hours. Tetracycline is widely distributed to the tissues, with 65% of the drug protein bound. It has the ability to cross the placenta and enter the breast milk. Elimination of 50% to 60% of the drug occurs in the urine within 72 hours. Its half-life in patients with normal renal function is 8 to 11 hours.
Action
Tetracycline penetrates microbial cells by passive diffusion and an active transport system. Intracellularly, it binds to the 30S ribosomes and possibly the 50S ribosomes and inhibits microbial protein synthesis. In patients with acne, it suppresses the growth of Propionibacterium acnes with sebaceous follicles, reducing the free fatty acid content in the sebum.
Use
Tetracycline is effective for treating Mycoplasma, Chlamydia, and Rickettsia. Health care providers administer it for the treatment of acne, chronic bronchitis, gonorrhea, and syphilis in patients with a known allergy to penicillin. Combined with other drugs, it may be effective in the eradication of Helicobacter pylori, thus reducing the risk of duodenal ulcers. Tetracycline is also useful in treating small animal bites and Lyme disease. In addition, it may be useful as adjunctive therapy for acute intestinal amebiasis and acne vulgaris. Finally, prescribers order tetracycline when penicillin is contraindicated to treat infections caused by Klebsiella, Neisseria gonorrhoeae, Treponema pallidum, Listeria monocytogenes, Clostridium, Bacillus anthracis, Fusobacterium fusiform, and Actinomyces.
Table 18.1 provides useful information about tetracycline and related drugs.
 TABLE 18.1
TABLE 18.1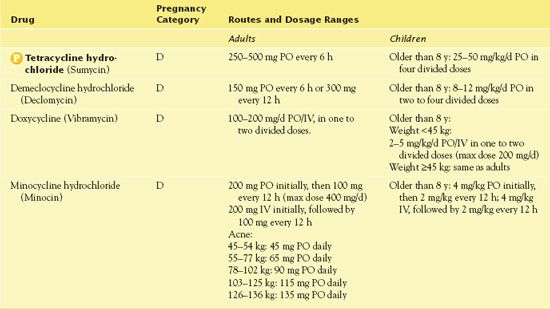
Use in Children
Children younger than 8 years of age should not take tetracyclines because of their effects on teeth and bones. In teeth, the drugs interfere with enamel development and may cause a permanent yellow, gray, or brown discoloration. In bone, the drugs form a stable compound in bone-forming tissue and may interfere with bone growth.
Use in Older Adults
A major concern with the use of tetracyclines is renal impairment, which commonly occurs in older adults. It is also necessary to monitor hepatic function in elderly patients during the administration of these drugs.
Use in Patients With Renal Impairment
Patients with renal impairment should not take tetracyclines. High concentrations of these drugs inhibit protein synthesis in human cells. This antianabolic effect increases tissue breakdown (catabolism) and the amount of waste products to be excreted by the kidneys. Normally functioning kidneys can handle the increased workload, but when renal function is impaired, the body retains these waste products. This leads to azotemia, increased blood urea nitrogen (BUN), hyperphosphatemia, hyperkalemia, and acidosis. If a tetracycline is necessary because of an organism’s sensitivity or a patient’s inability to take other antimicrobial drugs, administration of doxycycline or minocycline is necessary.
Use in Patients With Hepatic Impairment
The development of hepatotoxicity is rare, but caution is warranted when the medication is administered to patients with known hepatotoxicity. Tetracycline is generally contraindicated in pregnancy because it may cause fatal hepatic necrosis in the mother (as well as interfere with bone and tooth development in the fetus). However, there are some disorders where the benefit to the mother may outweigh the risk of hepatic dysfunction; these include rickettsial infections, ehrlichiosis, inhalational anthrax, and malaria.
Adverse Effects
Several adverse effects may occur following the administration of tetracycline. These include the following:
• Hypersensitivity such as rash, urticaria, serum sickness, or anaphylaxis. Maculopapular and erythematous rashes may also occur.
• Central nervous system (CNS) conditions such as intracranial hypertension (most severe CNS effect)
• Gastrointestinal (GI) conditions such as flatulence, diarrhea, nausea, vomiting, and epigastric distress (commonly reported). Esophagitis, pancreatitis, and staphylococcal enterocolitis may also occur.
Increase in Resistance Rates of H. pylori Isolates to Metronidazole and Tetracycline-Comparison of Three 3-Year Studies
by FARIDAEH SIAVOSHI, PhD, PARASTOO SANIEE, MSc, SAEID LATIFI-NAVID, PhD, SADEGH MASSARRATE, MD, ARGHAVAN SHEYKHOLESLAMI, MD
Archives of Iranian Medicine.
2010, 13(3): 177—187.
The aim of this 3-year study was to determine the usefulness of the treatment of Helicobacter pylori in dyspeptic diseases. The current trend of anti-infective agent use has contributed to the problem of resistant strains of H. pylori. The study included 110 H. pylori strains that were isolated in dyspeptic patients. The patients were tested for their susceptibility to anti-infective agents. It was found that 38.1% of the patients were resistant to tetracycline in the treatment of H. pylori.
IMPLICATIONS FOR NURSING PRACTICE: The resistance of anti-infective agents used in the treatment of infectious diseases is increasing. This requires that nurses carefully assess for the decrease of symptoms of the infectious disease when administering tetracycline.
• Superinfection:
• Candidal: sore throat, white patches on the oral mucosa, or a black, furry tongue
• GI: pseudomembranous colitis
• Other conditions such as increased pigmentation, photosensitivity reactions, azotemia, renal and hepatic toxicity, as well as retardation of bone growth. Discoloration of the teeth and enamel hypoplasia may occur in children younger than 8 years of age.
Contraindications
Contraindications to tetracycline include renal failure and known hypersensitivity to the drug. Other contraindications are young age (less than 8 years) and pregnancy; as previously stated, the drug causes permanent discoloration of teeth, defects in tooth enamel, and retardation of bone growth. Women who are breastfeeding should not take the drug because they secrete it into their breast milk. Possible hepatotoxicity may also be a problem.
Nursing Implications
Preventing Interactions
Many medications interact with tetracycline hydrochloride, increasing or decreasing its effects (Box 18.1). Tetracycline also affects the action of several drugs. Administering oral anticoagulants with tetracycline enhances the effect of vitamin K. Digoxin combined with tetracycline leads to increased digoxin absorption, resulting in digoxin toxicity. Giving penicillins with tetracycline interferes with the bactericidal effects of the penicillins. The combination of oral contraceptives and tetracycline results in diminished contraceptive effects. Some women need to use an additional form of birth control.
BOX 18.1  Drug Interactions: Tetracycline
Drug Interactions: Tetracycline
Drugs That Increase the Effects of Tetracycline
 Methoxyflurane
Methoxyflurane
Increases the risk of nephrotoxicity
Drugs That Decrease the Effects of Tetracycline
 Aluminum, antacids, bismuth subsalicylate, didanosine, ferrous sulfate, calcium, kaolin, laxatives, magnesium, pectin, zinc
Aluminum, antacids, bismuth subsalicylate, didanosine, ferrous sulfate, calcium, kaolin, laxatives, magnesium, pectin, zinc
Decrease antibiotic absorption
Foods that affect the action of tetracycline include dairy products, which decrease the absorption of the antibiotic.
Administering the Medication
It is important to obtain a culture and sensitivity prior to beginning therapy with tetracycline. Administration of the drug is oral. The medication is most effective when taken on an empty stomach. Patients should take the medication 1 hour before meals or 2 hours after meals. It is important not to take it with dairy products, antacids, or iron supplements. The combination of tetracycline with metallic ions such as aluminum, calcium, iron, or magnesium inhibits tetracycline absorption. If the patient has consumed dairy products or antacids, it is necessary to withhold tetracycline for 2 hours. Also, it is essential that tetracycline never be used after the expiration date. The administration of outdated tetracycline causes severe kidney damage.
Assessing for Therapeutic Effects
The nurse assesses for decreased signs and symptoms of the infection for which the medication is being administered. He or she checks for decreased pain and fever.
Assessing for Adverse Effects
The nurse assesses for GI irritation, nausea, epigastric distress, diarrhea, and vomiting. He or she also assesses for rash, anaphylaxis, and serum sickness. If a patient is exposed to sunlight, it is necessary to assess for sunburn or photosensitivity reactions. In addition, the nurse checks the patient’s complete blood count for anemia and signs and symptoms of superinfection.
Patient Teaching
Box 18.2 identifies patient teaching guidelines for tetracycline.
BOX 18.2  Patient Teaching Guidelines for Tetracycline
Patient Teaching Guidelines for Tetracycline
 Take tetracycline around the clock because it inhibits bacteria rather than kill the bacteria.
Take tetracycline around the clock because it inhibits bacteria rather than kill the bacteria.
 Avoid sunlamps, tanning beds, and intense or prolonged exposure to sunlight.
Avoid sunlamps, tanning beds, and intense or prolonged exposure to sunlight.
 Wear sunscreen and protective clothing when in the sun.
Wear sunscreen and protective clothing when in the sun.
 Report severe nausea, vomiting, diarrhea, skin rash, or perineal itching to your health care provider. These symptoms may indicate a need to change or stop the drug.
Report severe nausea, vomiting, diarrhea, skin rash, or perineal itching to your health care provider. These symptoms may indicate a need to change or stop the drug.
 Take the drug on an empty stomach, at least 1 hour before or 2 hours after meals.
Take the drug on an empty stomach, at least 1 hour before or 2 hours after meals.
 Do not take the drug with or within 2 hours of taking dairy products, antacids, or iron supplements.
Do not take the drug with or within 2 hours of taking dairy products, antacids, or iron supplements.
 If you must take an antacid, take it at least 2 hours before or 4 hours after tetracycline.
If you must take an antacid, take it at least 2 hours before or 4 hours after tetracycline.
 Take each dose with 8 ounces of water.
Take each dose with 8 ounces of water.
 If you are taking an oral contraceptive, use another form of birth control for the duration of therapy. The effectiveness of oral contraceptives is decreased when combined with tetracycline.
If you are taking an oral contraceptive, use another form of birth control for the duration of therapy. The effectiveness of oral contraceptives is decreased when combined with tetracycline.
 Never take outdated tetracycline due to the risk of severe reactions.
Never take outdated tetracycline due to the risk of severe reactions.
Other Drugs in the Class
Demeclocycline hydrochloride (Declomycin) is useful in the treatment of bacterial infections such as acne, pertussis, and UTIs caused by gram-positive or gram-negative organisms. An unlabeled use is for the treatment of chronic syndrome of inappropriate secretion of antidiuretic hormone. When administering demeclocycline, it is important to monitor the patient’s BUN. Increases in the BUN are secondary to antianabolic effects. Demeclocycline is the tetracycline most likely to cause photosensitivity.
Doxycycline (Vibramycin) is one of the drugs of choice for B. anthracis (anthrax); it is part of a combination drug regimen for postexposure prophylaxis and treatment. Patients who are exposed to anthrax should receive doxycycline for 60 days following exposure. The drug is also useful for infections with Chlamydia trachomatis and in respiratory tract infections due to Mycoplasma pneumoniae. In addition, people take doxycycline to prevent traveler’s diarrhea due to enterotoxic strains of Escherichia coli. Finally, it is effective in treating gonorrhea in patients who are allergic to penicillin.
The oral form of doxycycline, which is well absorbed in the GI tract, reaches serum levels equivalent to those obtained with parenteral administration. It is highly lipid soluble, reaching therapeutic levels in the cerebrospinal fluid (CSF), eye, and prostate gland. It can be administered in smaller doses and less frequently than other tetracyclines because of its long serum half-life of 18 hours. Excretion occurs in the kidneys; however, authorities consider the drug safe for patients with impaired renal function.
Parenteral administration of doxycycline requires mixing with lactated Ringer’s or dextrose 5% and lactated Ringer’s. Slow infusion is necessary. The minimum infusion period is 1 hour. Complete infusion should occur in 12 hours. Doxycycline is incompatible with allopurinol, barbiturates, erythromycin lactobionate, heparin, meropenem, nafcillin, penicillin, piperacillin, sulfonamides, and riboflavin.
Minocycline hydrochloride (Minocin) is a semisynthetic tetracycline derivative. It is useful in the treatment of mucopurulent cervicitis, lower respiratory tract infections caused by M. pneumoniae, and rickettsial and chlamydial infections. Administration of the drug is oral. Absorption is good, and foods and fluids affect absorption of minocycline less than other tetracyclines. It readily penetrates the CSF, eye, and prostate gland. From 70% to 75% of the drug is protein bound, and metabolism occurs in the liver. Excretion takes place in the urine and feces.
Intravenous (IV) administration of minocycline requires slow infusion. Prolonged IV administration of minocycline may be associated with thrombophlebitis. The drug is stable in all IV solutions but is incompatible with calcium-containing solutions.
Clinical Application 18-1
A nurse at the college health center is interviewing Ms. Dee about her recent health history. The nurse inquires if Ms. Dee is sexually active. She replies that she has a new boyfriend with whom she has had sexual intercourse every day for the past 5 days. She says she is taking oral contraceptives. The nurse also gathers information regarding Ms. Dee’s sunbathing practices (the college is on the Gulf Coast). Ms. Dee reports that she has been going to the beach daily.
 Based on the information gathered in the interview regarding the fact she is sexually active, what should the nurse instruct Ms. Dee on related to the tetracycline she is taking?
Based on the information gathered in the interview regarding the fact she is sexually active, what should the nurse instruct Ms. Dee on related to the tetracycline she is taking?
 What teaching should the nurse at the health center provide related to the administration of tetracycline?
What teaching should the nurse at the health center provide related to the administration of tetracycline?
 Based on the fact that Ms. Dee has been going to the beach daily, what is she at risk for developing?
Based on the fact that Ms. Dee has been going to the beach daily, what is she at risk for developing?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


