Describe the characteristics and specific uses of macrolide and ketolides anti-infective agents.
 Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications of macrolides.
Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications of macrolides.
 Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications of ketolides.
Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications of ketolides.
 Describe the action, use, adverse effects, contraindications, and nursing implications of miscellaneous anti-infective agents.
Describe the action, use, adverse effects, contraindications, and nursing implications of miscellaneous anti-infective agents.
 Implement the nursing process in the care of patients being treated with macrolides, ketolides, and other miscellaneous anti-infective agents.
Implement the nursing process in the care of patients being treated with macrolides, ketolides, and other miscellaneous anti-infective agents.
Clinical Application Case Study
Juro Nikki, a 65-year-old man, has had chronic obstructive pulmonary disease for a number of years. He presents to the physician’s office with a respiratory tract infection. He begins taking azithromycin, 500 mg for one dose, then 250 mg orally daily for 4 days.
KEY TERMS
Glycylcyclines: class of anti-infective agents that are structurally related to the tetracyclines and share many of the same properties; used for the treatment of complicated skin and skin structure infections caused by methicillin-resistant Staphylococcus aureus and vancomycin-sensitive Enterococcus faecalis, as well as treatment of complicated intra-abdominal infections
Gray syndrome: dangerous condition that occurs in newborns who are given chloramphenicol; may lead to fatalities
Ketolides: newer class of antibiotics that belong to the macrolide group; have a more broad-spectrum effect compared to macrolides, especially Streptococcus pneumoniae infections
Lincosamides: similar to macrolides in their mechanism of action and antimicrobial spectrum
Lipopeptides: a new class of antibiotics that kills gram-positive bacteria by inhibiting synthesis of bacterial proteins, DNA, and RNA
Macrolides: may be bacteriostatic or bactericidal, depending on drug concentrations in infected tissues; widely used for treatment of respiratory tract and skin/soft tissue infections caused by streptococci and staphylococci
Methicillin-resistant Staphylococcus aureus: microorganisms resistant to broad-spectrum antibiotics such as penicillin and erythromycin; frequently colonizes nasal passages of health care workers and is increasing as a cause of infection in health care facilities
Methicillin-resistant Staphylococcus species non-aureus: other strains of antibiotic-resistant staphylococci
Methicillin-susceptible Staphylococcus aureus: methicillin-susceptible strains of Staphylococcus aureus
Mycobacterium avium complex: caused by atypical mycobacteria; opportunistic infection that occurs mainly in people with advanced human immunodeficiency virus infection
Oxazolidinones: newer class of antibiotics; active against aerobic gram-positive bacteria by inhibiting protein synthesis
Red man syndrome: adverse reaction when vancomycin is administered too quickly; characterized by hypotension, flushing, and skin rash
Streptogramins: class of antibacterial drugs; produced by Streptomyces graminofaciens bacteria
Vancomycin-resistant enterococci: pathogenic bacteria that are resistant to vancomycin
Vancomycin-resistant Enterococcus faecium : Enterococcus faecium that is resistant to vancomycin
Introduction
The drugs described in this chapter are heterogeneous in their antimicrobial spectra, characteristics, and clinical uses. Some are used often, and some are used only in specific circumstances. The drugs to be described in the following sections include the macrolides, ketolides, and miscellaneous anti-infective agents. The Drugs at a Glance tables present information about individual drugs and the prototype drugs, with routes of administration and dosage ranges.
Macrolides
The macrolides, which include erythromycin, azithromycin, and clarithromycin, have similar antibacterial spectra and mechanisms of action. Macrolides are widely distributed into body tissues and fluids and may be bacteriostatic or bactericidal, depending on drug concentration in infected tissues. They are effective against gram-positive cocci, including group A streptococci, pneumococci, and most staphylococci. They are also effective against species of Corynebacterium, Treponema, Legionella, Chlamydia, Neisseria, and Mycoplasma and against some anaerobic species of genera such as Bacteroides and Clostridia. The prototype macrolide is  erythromycin. This drug is now used less often because of microbial resistance, numerous drug interactions, and the development of newer macrolides. Compared with erythromycin, the newer drugs, such as azithromycin and clarithromycin, have enhanced antibacterial activity, require less frequent administration, and cause less nausea, vomiting, and diarrhea (see Other Drugs in the Class). Erythromycin is available in several preparations. Ophthalmic and topical preparations are discussed in Chapters 58 and 60, respectively.
erythromycin. This drug is now used less often because of microbial resistance, numerous drug interactions, and the development of newer macrolides. Compared with erythromycin, the newer drugs, such as azithromycin and clarithromycin, have enhanced antibacterial activity, require less frequent administration, and cause less nausea, vomiting, and diarrhea (see Other Drugs in the Class). Erythromycin is available in several preparations. Ophthalmic and topical preparations are discussed in Chapters 58 and 60, respectively.
Pharmacokinetics
The oral preparation of erythromycin is absorbed in the small intestine and has an onset of action in 1 to 2 hours. The medication reaches its peak in 1 to 4 hours. The intravenous (IV) preparation has a rapid onset of action, reaching a peak of action in less than 1 hour. Both the oral and parenteral forms cross the placenta and enter the breast milk. Erythromycin is metabolized in the liver by the cytochrome P450 3A4 (CYP3A4) isoenzymes and excreted mainly in bile; approximately 20% is excreted in urine. Depending on the specific salt formulation used, food can have a variable effect on the absorption of oral erythromycin.
Action
Erythromycin enters the microbial cells and reversibly binds to the 50S subunits of ribosomes, thereby inhibiting microbial protein synthesis and leading to cell death. The medication has bacteriostatic or bactericidal activity against susceptible bacteria.
Use
Erythromycin is useful as a penicillin substitute in patients who are allergic to penicillin; for prevention of rheumatic fever, gonorrhea, syphilis, pertussis, and chlamydial conjunctivitis in newborns (ophthalmic ointment); and to treat other infections (e.g., Legionnaire’s disease, genitourinary infections caused by Chlamydia trachomatis, intestinal amebiasis caused by Entamoeba histolytica). The drug is administered for upper respiratory infections caused by group A beta-hemolytic streptococci. It is used for with sulfonamides for upper respiratory infections caused by Haemophilus influenzae. Prophylactically, erythromycin is administered to prevent alpha-hemolytic streptococcal endocarditis before dental or other procedures in patients who have valvular heart disease and are allergic to penicillin. Table 19.1 provides route and dosage information for erythromycin and other macrolides.
 TABLE 19.1
TABLE 19.1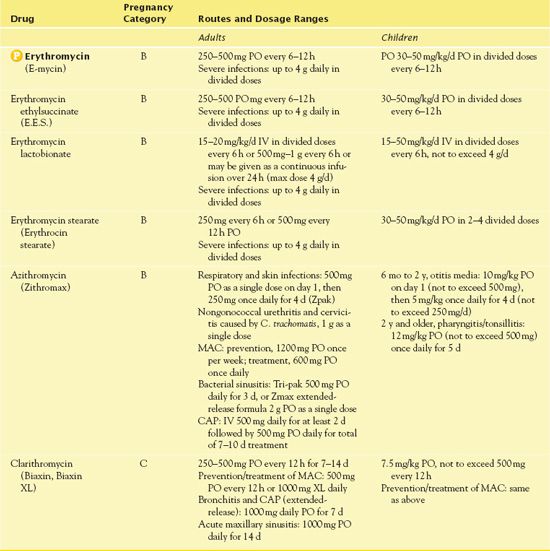
IV, intravenous; CAP, community-acquired pneumonia; MAC, Mycobacterium avium complex.
Use in Patients With Hepatic Impairment
Using erythromycin warrants caution, if the drug is given at all, to patients with hepatic impairment, because it is metabolized in the liver to an active metabolite that is excreted in the bile. Avoiding the drug or dosage reduction may be necessary in hepatic failure. It has also been associated with cholestatic hepatitis.
Use in Patients With Critical Illness
Erythromycin is seldom used in critical care settings, partly because broader spectrum bactericidal drugs are usually needed in critically ill patients and partly because it inhibits liver metabolism and slows elimination of several other drugs. For a critically ill patient who needs a macrolide antibiotic, one of the newer macrolides is preferred because the newer drugs have activity against several groups of microorganisms and fewer effects on the metabolism of other drugs.
Adverse Effects
Erythromycin may result in several adverse effects. Gastrointestinal (GI) effects include nausea, vomiting, diarrhea, cramping, anorexia, hepatotoxicity, and pseudomembranous colitis. If fever and jaundice occur after 1 to 2 weeks of drug administration, they subside after the drug is discontinued. Central nervous system (CNS) effects are reversible hearing loss, confusion, lability of emotions, and alterations in thought processes. Cardiac effects, with the IV form of the drug, include possible ventricular dysrhythmias. Allergic reactions include redness of the skin, rash, bronchospasm, or anaphylaxis.
Contraindications
Contraindications to erythromycin include a known hypersensitivity reaction to the drug or any macrolide. As previously stated, hepatic insufficiency requires careful use. The U.S. Food and Drug Administration (FDA) has issued a BLACK BOX WARNING ♦ regarding erythromycin estolate, a Canadian preparation of erythromycin; administration to patients with known liver disease warrants caution. Women who are breastfeeding should not take erythromycin because the drug is concentrated in the breast milk. This can alter the bowel flora of the infant and interfere with fever assessments. Also, people should not take erythromycin if they are concurrently using drugs highly dependent on CYP3A4 liver enzymes for metabolism.
Nursing Implications
Preventing Interactions
Many medication and herbs interact with erythromycin, increasing or decreasing its effects (Boxes 19.1 and 19.2).
BOX 19.1  Drug Interactions: Erythromycin
Drug Interactions: Erythromycin
Drugs That Increase the Effects of Erythromycin
 Chloramphenicol
Chloramphenicol
Increases effectiveness against strains of resistant S. aureus
 Streptomycin
Streptomycin
Increases effectiveness against Enterococcus in bacteremia, brain abscess, endocarditis, meningitis, and urinary tract infection
Drugs That Decrease the Effects of Erythromycin
 Antacids, calcium, magnesium, aluminum, and zinc
Antacids, calcium, magnesium, aluminum, and zinc
Decrease antibiotic absorption
 Etravirine and lincosamide antibiotics
Etravirine and lincosamide antibiotics
Decrease serum concentration of erythromycin
 Ethanol
Ethanol
Decreases the absorption of erythromycin
BOX 19.2  Herb and Dietary Interactions: Erythromycin
Herb and Dietary Interactions: Erythromycin
Herbs and Foods That Decrease the Effects of Erythromycin
 Grapefruit juice
Grapefruit juice
Decreases antibiotic absorption
 St. John’s Wort
St. John’s Wort
Decreases antibiotic absorption
In addition, as stated previously, the CYP3A4 isoenzymes in the liver metabolize erythromycin. The drug interacts with other drugs metabolized by the same isoenzyme and interferes with the elimination of several drugs. As a result, the affected drugs are eliminated more slowly, their serum levels are increased, and they are more likely to cause adverse effects and toxicity unless the erythromycin dosage is reduced. In combination with potent inhibitors of CYP3A4 (e.g., fluconazole, diltiazem), erythromycin increases the risk of sudden cardiac death. A partial list of other interacting drugs includes carbamazepine (Tegretol), cyclosporine (Sandimmune), digoxin (Lanoxin), disopyramide (Norpace), lopinavir/ritonavir (Kaletra), lovastatin (Mevacor), nevirapine (Viramune), pimozide (Orap), quinidine, rifampin (Rifadin), ritonavir (Norvir), simvastatin (Zocor), theophylline (Theo-Dur), triazolam (Halcion), and warfarin (Coumadin). These drugs represent a variety of drug classes.
Administering the Medication
It is necessary to take oral erythromycin according to manufacturer’s instructions. Drinking 6 to 8 ounces of water with the medication is important; adequate water aids absorption of the medication. It is necessary to take the drug on an empty stomach at evenly spaced intervals around the clock. Regular intervals help maintain therapeutic blood levels. People should not take erythromycin after taking antacids. Antacids decrease the absorption of both the tablet and suspension form of erythromycin.
The nurse may administer the IV administration preparation of erythromycin without regard to meals. It is important to consult the manufacturer’s instructions for dissolving, diluting, and administering the parenteral form of erythromycin to achieve therapeutic effects. The IV formulation has limited stability in the solution. Also, instructions differ for intermittent and continuous infusions. The nurse infuses the medication in a peripheral or central IV site every 6 hours over 30 to 60 minutes.
Assessing Therapeutic Effects
The nurse assesses for decreased pain, fever, and malaise. Both the local and systemic signs of the infection are decreased, and the patient has decreased signs and symptoms of the specific infection for which erythromycin is being administered.
Assessing for Adverse Effects
With erythromycin, it is important to assess the patient’s hearing. The loss of hearing is reversible with the discontinuation of the medication. The nurse also assesses for nausea, vomiting, and diarrhea. These symptoms may be severe and result in an alteration in acid–base balance. In addition, the nurse assesses for superinfection, as noted, with the development of pseudomembranous colitis. It is important to assess the patient’s psychosocial responses that are adverse effects of erythromycin, such as crying, laughing, and altered thought processes. Finally, the nurse assesses for skin rash, urticaria, edema, dermatitis, and bronchospasm. These symptoms are indicative of an allergic reaction to erythromycin.
When administering the IV form of the drug, the nurse assesses the infusion site for phlebitis.
Patient Teaching
Box 19.3 identifies patient teaching guidelines for erythromycin.
BOX 19.3  Patient Teaching Guidelines for Erythromycin
Patient Teaching Guidelines for Erythromycin
 Erythromycin should be taken around the clock because it inhibits bacteria; it does not kill them.
Erythromycin should be taken around the clock because it inhibits bacteria; it does not kill them.
 Take erythromycin on an empty stomach, 1 hour before meals or 2 to 3 hours after meals.
Take erythromycin on an empty stomach, 1 hour before meals or 2 to 3 hours after meals.
 Do not drink grapefruit juice while taking erythromycin.
Do not drink grapefruit juice while taking erythromycin.
 Complete the full course of the prescription.
Complete the full course of the prescription.
 Do not take with or within 2 hours of dairy products or antacids.
Do not take with or within 2 hours of dairy products or antacids.
 Take each dose with 8 ounces of water.
Take each dose with 8 ounces of water.
 Be aware that the effectiveness of oral contraceptives is decreased when combined with erythromycin.
Be aware that the effectiveness of oral contraceptives is decreased when combined with erythromycin.
 Adverse effects that you may experience include stomach cramping, gastrointestinal discomfort, labile emotions, crying, laughing, and abnormal thinking.
Adverse effects that you may experience include stomach cramping, gastrointestinal discomfort, labile emotions, crying, laughing, and abnormal thinking.
 Report severe or watery diarrhea, nausea, vomiting, dark urine, yellowing of the eyes or skin, loss of hearing, itching, and rash to your prescriber.
Report severe or watery diarrhea, nausea, vomiting, dark urine, yellowing of the eyes or skin, loss of hearing, itching, and rash to your prescriber.
Other Drugs in the Class
The macrolides azithromycin and clarithromycin are active against the atypical mycobacteria that cause Mycobacterium avium complex (MAC) disease. MAC disease (see Chap. 20) is an opportunistic infection that occurs mainly in people with advanced human immunodeficiency virus (HIV) infection. Helicobacter pylori, a pathogen implicated in peptic ulcer disease, is also susceptible to treatment with azithromycin or clarithromycin as part of a combination regimen (see Chap. 35).
Azithromycin (Zithromax) is useful in the treatment of lower respiratory infections, pharyngitis, and tonsillitis caused by Haemophilus ducreyi, H. influenzae, Moraxella catarrhalis, and Streptococcus pneumoniae. Prescribers order the drug for children older than 6 months of age for otitis media. It is also effective for treatment of community-acquired pneumonia (CAP) caused by S. pneumoniae as well as for genital ulcer disease in men and pelvic inflammatory disease in women. As previously stated, people with advanced HIV take azithromycin for MAC.
The onset of action of azithromycin is rapid, with a peak of action in 2.5 to 3.2 hours. The duration of action is 24 hours. The medication is metabolized in the liver and is distributed extensively to the tissues, skin, lungs, sputum, tonsils, and cervix. A minimal amount enters the cerebrospinal fluid (CSF). Major elimination of the drug is in the bile, with only 6% of excretion in the urine. The mechanism of action is the inhibition of RNA-dependent protein synthesis at the chain elongation step; the drug binds to the 50S ribosomal subunit to block the involved transpeptide. The parenteral form of azithromycin is stable in 5% dextrose and water, 5% dextrose and lactated Ringer’s solution, lactated Ringer’s solution, normal saline, and all 5% dextrose and saline IV fluids.
The adverse effects of azithromycin are similar to those of erythromycin. Caution is necessary with azithromycin in patients who have gonorrhea, syphilis, pseudomembranous colitis, and hepatic and renal impairment, as well as in lactating women. Alfuzosin, amiodarone, and artemether combined with azithromycin can enhance QT elongations. Careful assessment of the cardiac status is crucial when these medications are combined. Close monitoring of the international normalized ratio (INR) and prothrombin time is necessary when azithromycin is administered with warfarin. Patients should take the oral medication on an empty stomach, 2 hours before or after the administration of aluminum-or magnesium-containing antacids.
Clarithromycin (Biaxin, Biaxin XL) is a macrolide administered for bronchitis, sinusitis, otitis media, MAC, peptic ulcer disease, pertussis, pharyngitis, tonsillitis, and pneumonia. Prescribers also order the drug for prophylactic use in patients with underlying cardiac conditions who are undergoing invasive procedures that predispose them to infective endocarditis. It is also useful in skin infections caused by Staphylococcus aureus and Streptococcus pyogenes as well as in duodenal ulcers caused by H. pylori.
Absorption of clarithromycin is rapid, and the serum half-life is 3 to 7 hours. The drug is 42% to 50% protein bound, and it is widely distributed to all body tissues except the CNS. The metabolism of the medication takes place partially in the liver with CYP3A4 and is converted to the active metabolite. Metabolism occurs in the liver, and elimination takes place in the urine, with 20% to 40% of the drug unchanged. (An additional 10% to 15% remains as the metabolite.) Clarithromycin binds to the 50S ribosome to inhibit protein synthesis. One of its metabolites is two times as active as the parent compound against certain organisms.
The adverse effects of clarithromycin are headache, rash, abnormal taste, nausea, vomiting, abdominal pain, and dyspepsia. People should not take the drug with ergot derivatives, pimozide, cisapride, astemizole, colchicine, or terfenadine due to the risk of increased levels of the medications and toxicity. Generally, people may take it with or without food; however, they should take the extended-release form on an empty stomach. As with the other macrolides, use of aluminum-or magnesium-containing antacids within 2 hours of administration of clarithromycin decreases absorption of the antibiotic.
Clinical Application 19-1
The home care nurse is visiting Mr. Nikki to assess his lung status and medication regimen. Along with azithromycin, Mr. Nikki is taking omeprazole 20 mg orally daily for gastric reflux and 30 mL of Maalox at night. Since his myocardial infarction 6 months ago, he has been also taking warfarin 2 mg orally daily.
 The nurse is educating Mr. Nikki on all aspects of azithromycin. Identify all aspects of patient teaching to be provided to him.
The nurse is educating Mr. Nikki on all aspects of azithromycin. Identify all aspects of patient teaching to be provided to him.
 What instructions does the nurse provide regarding the other medications Mr. Nikki is taking?
What instructions does the nurse provide regarding the other medications Mr. Nikki is taking?
 What laboratory tests are important to monitor during the administration of azithromycin?
What laboratory tests are important to monitor during the administration of azithromycin?
NCLEX Success
1. A patient is admitted to the critical care unit with a diagnosis of Legionnaire’s disease. Based on your knowledge of pharmacology, which medication is the drug of choice to treat the infection?
A. azithromycin
B. clarithromycin
C. erythromycin
D. vancomycin
2. The nurse instructs a patient on the administration of clarithromycin. Which of the following patient teaching instructions is appropriate?
A. Take the medication on an empty stomach.
B. Take the medication with a calcium supplement.
C. Take the medication with a class of milk.
D. Take the medication with cheese.
3. A teenage boy receives a prescription for erythromycin for an upper respiratory tract infection. He complains that he cannot hear the teacher, who then sends him to the school nurse’s office. After assessing the patient’s hearing with a tuning fork, the nurse determines that his hearing is diminished. What is the most important nursing intervention?
A. The nurse should notify the parents to call the physician; this is an adverse effect of erythromycin.
B. The nurse should inform the parents of a physician who specializes in ear, nose, and throat surgery.
C. The nurse should instruct the patient to stop taking the erythromycin and his hearing will improve.
D. The nurse should call the physician and inform the patient of a change in antibiotics.
4. A parent of a high school student calls the school nurse regarding her daughter’s crying. The parent states that this behavior is unusual for her daughter. Which of the following medications contributes to changes in behavior?
A. metronidazole
B. naproxen sodium
C. vitamin C
D. erythromycin
5. A man had rheumatic fever as a child. He has an appointment for a tooth extraction. His dentist prescribes which of the following medications prior to the extraction?
A. chloramphenicol
B. vancomycin
C. clarithromycin
D. digoxin



