Define local anesthesia.
 Describe three types of local anesthesia.
Describe three types of local anesthesia.
 Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for the amide local anesthetics.
Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for the amide local anesthetics.
 Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for the ester local anesthetics.
Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for the ester local anesthetics.
 Implement the nursing process in the care of patients receiving local anesthesia.
Implement the nursing process in the care of patients receiving local anesthesia.
Clinical Application Case Study
Lexi Scruggs, a 7-year-old girl, was swinging from the monkey bars on the school playground. She lost her grip and fell, cutting her left knee on a piece of glass. At the emergency department, she requires 10 sutures to close the jagged cut. She receives lidocaine (Xylocaine) prior to cleaning and suturing the wound.
KEY TERMS
Bier block anesthesia: regional limb anesthesia provided by local anesthesia and an extremity tourniquet
Epidural anesthesia: injection of an anesthetic into the epidural space
Local anesthetics: agents that produce loss of sensation and motor activity
Local anesthetic systemic toxicity (LAST): systemic absorption of a local anesthetic agent that results in excitation of the CNS
Spinal anesthesia: injection of anesthetic into the cerebrospinal fluid, usually in the lumbar spine
Topical anesthesia: application of a local anesthetic on the skin or mucous membranes
Introduction
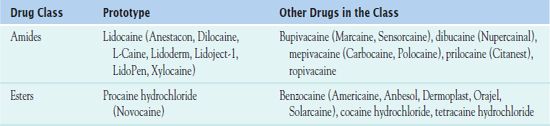
This chapter introduces the fundamentals of local anesthesia and the implementation of nursing care during the administration of local anesthesia. The local anesthetic agents are classified as amides and esters. The molecular structure of the amides possess an amide linkage and the esters contains an ester linkage.
Overview of Local Anesthesia
Local anesthetics, given to produce loss of sensation and motor activity, are injected into localized areas of the body. These agents decrease the permeability of the nerve cell membrane to ions, especially sodium. This action reduces the excitability of cell membranes. When the excitability falls, the nerve impulses can no longer be initiated or conducted by the anesthetized nerves. These drugs prevent the cells from responding to pain impulses and sensory stimulation.
Local anesthetic effects diminish as the drug molecules diffuse out of the neurons into the bloodstream. The drugs are then transported to the liver for metabolism to inactive metabolites and eventual excretion in the urine.
There are three common types of local anesthesia.
• Spinal anesthesia involves injecting the anesthetic agent into the cerebrospinal fluid, usually in the lumbar spine. The anesthetic blocks sensory impulses at the root of peripheral nerves as they enter the spinal cord. Spinal anesthesia is especially useful for surgery involving the lower abdomen and legs.
• Epidural anesthesia involves injecting the anesthetic into the epidural space. It is used most often in obstetrics during labor and delivery. The epidural route is also used to provide analgesia (often with a combination of a local anesthetic and an opioid) for patients with postoperative or other pain. When the combination is used, it is essential to reduce the dosage of the anesthetic and the opioid to avoid respiratory depression and other adverse effects.
• Topical anesthesia involves application of a local anesthetic to skin and mucous membranes. The anesthetic is usually an ingredient in ointments, solutions, or lotions designed for use at particular sites. For example, preparations are available for use on eyes, ears, nose, oral mucosa, perineum, hemorrhoids, and skin. These preparations are used to relieve pain and itching of dermatoses, sunburn, minor skin wounds, hemorrhoids, sore throat, and other conditions. The main adverse effect is allergic reactions.
Table 49.1 lists the drugs administered for local anesthesia. The use of topical anesthetics is especially important in children, who are administered local anesthesia before suturing, insertion of an intravenous (IV) line, or vaccination administration. Box 49.1 summarizes the use of topical anesthesia in children.
BOX 49.1 Topical Anesthesia Used in Children
 Eutectic mixture of local anesthetics (EMLA): This cream-based mixture of lidocaine and prilocaine is applied to intact skin. The cream penetrates intact skin to provide local anesthesia and decrease pain of vaccinations and venipuncture. The cream is applied at the injection site with an occlusive dressing at least 60 minutes before the vaccination or venipuncture. EMLA should never be applied to abraded skin or mucous membranes.
Eutectic mixture of local anesthetics (EMLA): This cream-based mixture of lidocaine and prilocaine is applied to intact skin. The cream penetrates intact skin to provide local anesthesia and decrease pain of vaccinations and venipuncture. The cream is applied at the injection site with an occlusive dressing at least 60 minutes before the vaccination or venipuncture. EMLA should never be applied to abraded skin or mucous membranes.
 Lidocaine, epinephrine, and tetracaine (LET): This combination of lidocaine (4%), epinephrine (0.1%), and tetracaine (0.5%) is an aqueous solution or gel that blocks the sensory and motor nerves. It inhibits axonal sodium channels, thus blocking conduction of action potential. Epinephrine causes local vasoconstriction, whereas lidocaine and tetracaine produce numbness and weakness. It is used for laceration repair.
Lidocaine, epinephrine, and tetracaine (LET): This combination of lidocaine (4%), epinephrine (0.1%), and tetracaine (0.5%) is an aqueous solution or gel that blocks the sensory and motor nerves. It inhibits axonal sodium channels, thus blocking conduction of action potential. Epinephrine causes local vasoconstriction, whereas lidocaine and tetracaine produce numbness and weakness. It is used for laceration repair.
 Needle-free lidocaine delivery: Lidocaine is administered by compressed gas. It reduces pain at the site of venipunctures or intravenous line insertion.
Needle-free lidocaine delivery: Lidocaine is administered by compressed gas. It reduces pain at the site of venipunctures or intravenous line insertion.
 Liposomal lidocaine (LMX 4 or LMX 5): This solution contains lidocaine encapsulated in liposomes. It is applied to intact skin with the use of an occlusive dressing.
Liposomal lidocaine (LMX 4 or LMX 5): This solution contains lidocaine encapsulated in liposomes. It is applied to intact skin with the use of an occlusive dressing.
NCLEX Success
1. A 50-year-old patient is 1 day postoperative following abdominal surgery for resection of colon cancer. Which of the following pain control devices is most effective in treating his pain?
A. fentanyl citrate by the transdermal route
B. bupivacaine hydrochloride by the epidural route
C. lidocaine by the transdermal route
D. fentanyl citrate by patient-controlled analgesia
2. Local anesthetics decrease the permeability of the nerve cells to ions. What is the most significant ion that reduces the excitability of the cell membrane?
A. sodium
B. potassium
C. chloride
D. magnesium
Amides
 Lidocaine (Anestacon, Dilocaine, L-Caine, Lidoderm, Lidoject-1, LidoPen, Xylocaine) is the prototype amide local anesthetic. It has a rapid effect, and, when combined with epinephrine, this effect is prolonged.
Lidocaine (Anestacon, Dilocaine, L-Caine, Lidoderm, Lidoject-1, LidoPen, Xylocaine) is the prototype amide local anesthetic. It has a rapid effect, and, when combined with epinephrine, this effect is prolonged.
Pharmacokinetics and Action
The pharmacokinetics of lidocaine depend on the route of administration. The onset of action may be almost immediate, with a peak of 2 to 5 minutes and a duration of 30 to 120 minutes. The anesthetic has an elimination half-life of 96 minutes, and therefore, a single dose should not be repeated during this time frame. It is metabolized in the liver into two active metabolites, and most is excreted in the urine.
Lidocaine diminishes pain by blocking nerve conduction. It decreases the neuronal membrane’s permeability to sodium ions. This action then inhibits the depolarization and blocks nerve conduction.
Use
Clinicians use lidocaine in its various forms to obtain local anesthesia. Specific uses include
• Topical preparation: used to relieve pain associated with postherpetic neuralgia
• Injectable solution: used for infiltration of the skin or subcutaneous administration prior to the insertion of an IV or central venous catheter, spinal, epidural or a minor emergency procedure such as suturing or a minor surgical procedure.
• 2% solution: administered intravenously preceding administration of a painful IV medication such as propofol (Diprivan) in the surgical arena. Lidocaine 2% is also used in conjunction with other local anesthetics to achieve epidural anesthesia, appropriate for surgical procedures, treatment of postoperative pain, or management of labor pain. In addition, it can be administered as surface anesthesia for a diagnostic procedure of the upper respiratory tract, such as a medical thoracoscopy.
• 0.5% to 2% solution: administered for IV regional anesthesia. Bier block anesthesia is regional limb anesthesia produced by a local anesthetic such as lidocaine and a pneumatic extremity tourniquet. The tourniquet prevents lidocaine and blood flow from the extremity to enter the general circulation.
• 4% solution: administered through a nebulizer and inhaled into the lungs to produce anesthesia for a diagnostic procedure, such as a bronchoscopy.
Table 49.2 gives route and dosage information for lidocaine and other amide local anesthetics.
 TABLE 49.2
TABLE 49.2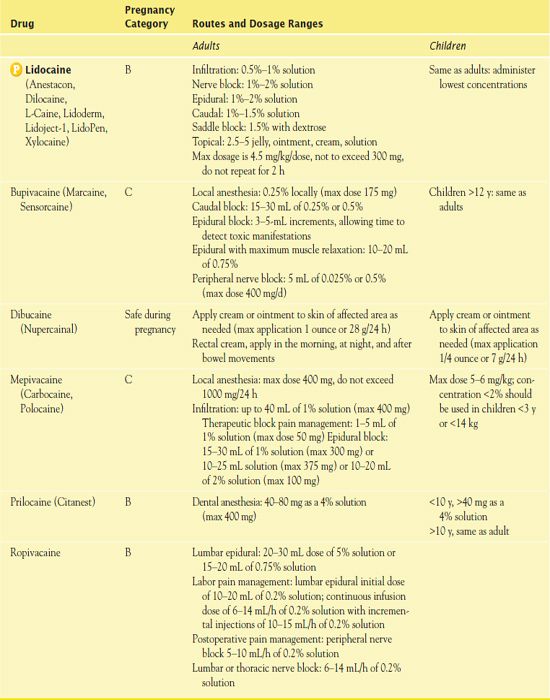
Adverse Effects
Local anesthetic systemic toxicity (LAST) is the most severe and life-threatening effect associated with the use of lidocaine or any local anesthetic. LAST occurs when the local anesthetic is absorbed systemically, resulting in extreme central nervous system (CNS) excitation followed by cardiovascular excitation and cardiovascular collapse. Initial symptoms may include analgesia, circumoral numbness, metallic taste, tinnitus or auditory changes, and agitation. These may progress to seizure activity and then lead to symptoms of CNS depression, including coma, respiratory arrest, and cardiovascular depression.
Contraindications
A known hypersensitivity or allergic reaction to an amide local anesthetic rules out the use of lidocaine in any form. Any patient may experience hypersensitivity reactions to any local anesthetic. If lidocaine is combined with sulfites, the patient may develop a laryngospasm. Other contraindications include severe trauma, sepsis, blood dyscrasias, and cardiac abnormalities, including heart block.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


