State the rationale for the increasing use of single daily doses of aminoglycosides.
 Discuss the importance of measuring serum drug levels during aminoglycoside therapy.
Discuss the importance of measuring serum drug levels during aminoglycoside therapy.
 Describe measures to decrease nephrotoxicity and ototoxicity with aminoglycosides.
Describe measures to decrease nephrotoxicity and ototoxicity with aminoglycosides.
 Identify characteristics of aminoglycosides and fluoroquinolones in relation to effectiveness, safety, spectrum of antimicrobial activity, indications for use, administration, and observation of patient responses.
Identify characteristics of aminoglycosides and fluoroquinolones in relation to effectiveness, safety, spectrum of antimicrobial activity, indications for use, administration, and observation of patient responses.
 Recognize factors influencing selection and dosage of aminoglycosides and fluoroquinolones.
Recognize factors influencing selection and dosage of aminoglycosides and fluoroquinolones.
 Describe characteristics, uses, adverse effects, and nursing process implications of fluoroquinolones.
Describe characteristics, uses, adverse effects, and nursing process implications of fluoroquinolones.
 Discuss principles of using aminoglycosides and fluoroquinolones in renal impairment and critical illness.
Discuss principles of using aminoglycosides and fluoroquinolones in renal impairment and critical illness.
Clinical Application Case Study
Edward Louis, an 84-year-old man, is taking ciprofloxacin (Cipro) 500 mg PO every 12 hours for an infected leg wound. He has experienced arterial insufficiency to his lower extremities for many years, secondary to atherosclerosis. The medical plan is to clear the infection so that he can have surgery to restore circulation to his lower extremities.
KEY TERMS
Concentration-dependent bactericidal effect: relation of bactericidal ability of a drug to its concentration; the greater the concentration of the drug, the faster and the more extensive the killing of the bacteria. The goal is to maximize concentration of the drug. Once-daily dosing—single daily aminoglycoside dosing, typically using a dose of 7 mg per kg every 24 hours, or longer in patients with renal impairment.
Ototoxicity: adverse effects on the structures of the ear, especially the cochlea and auditory nerve
Postantibiotic effect: persistent effect of an antimicrobial on bacterial growth after brief exposure of the organisms to a drug
Introduction
Health care practitioners have used the aminoglycosides to treat serious aerobic gram-negative infections extensively for many years. Select aminoglycosides have shown stability in the face of the emergence of resistance. The quinolones are also older drugs originally used only for the treatment of urinary tract infections (see Chap. 18). Synthesis of the quinolones involves adding a fluorine molecule to the quinolone structure. This addition increases drug activity against gram-negative microorganisms, broadens the antimicrobial spectrum to include several other microorganisms, and allows the use of the drugs in treating systemic infections. General characteristics, mechanisms of action, indications for and contraindications to use, nursing process implications, and principles of therapy for these drugs are described in this chapter. Individual drugs and the prototype drugs, with routes of administration and dosage ranges, are presented in the Drugs at a Glance tables.
Aminoglycosides
Aminoglycosides are bactericidal agents with similar pharmacologic, antimicrobial, and toxicologic characteristics. They are used to treat infections caused by gram-negative microorganisms such as Pseudomonas and Proteus species, Escherichia coli, and Klebsiella, Enterobacter, and Serratia species.  Gentamicin (Garamycin), the most widely used aminoglycoside, is the prototype. Patients often receive gentamicin for systemic infections in the clinical setting. If it is a concern, patients may receive amikacin or tobramycin because these drugs are usually less susceptible to drug-destroying enzymes.
Gentamicin (Garamycin), the most widely used aminoglycoside, is the prototype. Patients often receive gentamicin for systemic infections in the clinical setting. If it is a concern, patients may receive amikacin or tobramycin because these drugs are usually less susceptible to drug-destroying enzymes.
Maintenance doses are based on serum drug concentrations. Peak serum concentrations should be determined 30 to 60 minutes after drug administration (5 to 8 mcg per mL for gentamicin and tobramycin; 20 to 30 mcg per mL for amikacin). Measurement of both peak and trough levels helps maintain therapeutic serum levels without excessive toxicity. For gentamicin and tobramycin, peak levels above 10 to 12 mcg per mL and trough levels above 2 mcg per mL for prolonged periods have been associated with nephrotoxicity. For accuracy, it is necessary to draw blood samples at the correct times and to document the timing of drug administration and blood sampling accurately, based on institutional recommendations.
Pharmacokinetics
Gentamicin is poorly absorbed from the gastrointestinal (GI) tract. Thus, when given orally, the drug exerts local effects in the GI tract. It is rapidly and completely absorbed from intramuscular (IM) injection sites and reaches peak effects in 30 to 90 minutes if circulatory status is proficient. After intravenous (IV) administration, the peak effect occurs 30 minutes after a 30-minute infusion. Plasma half-life is 2 to 4 hours in patients with normal renal function. The volume of distribution is increased by edema, ascites, and fluid overload, and it is decreased with dehydration.
After parenteral administration, gentamicin is widely distributed in extracellular fluid and reaches therapeutic levels in blood, urine, bone, inflamed joints, and pleural and ascitic fluids. Gentamicin accumulates in high concentrations in the proximal renal tubules of the kidney, potentially leading to acute tubular necrosis. This damage to the kidney is termed nephrotoxicity. Gentamicin also accumulates in high concentrations in the inner ear, damaging sensory cells in the cochlea (disrupting hearing) and the vestibular apparatus (disturbing balance). This damage to the inner ear is termed ototoxicity. Gentamicin is poorly distributed in the central nervous system, intraocular fluids, and respiratory tract secretions.
Action
Aminoglycosides penetrate the cell walls of susceptible bacteria and bind irreversibly to 30S and 50S ribosomal subunits, intracellular structures that synthesize proteins. As a result, the bacteria cell membrane becomes defective and cannot synthesize the proteins necessary for their function and replication.
Use
The major clinical use of gentamicin (most commonly with other antibacterial agents) is empiric therapy for serious infections caused by susceptible aerobic gram-negative organisms. Treatment of infections such as septicemia, respiratory tract infections, urinary tract infections, intra-abdominal infections, and osteomyelitis often involves gentamicin. In pseudomonal infections, patients may receive gentamicin concurrently with an antipseudomonal penicillin (e.g., piperacillin/tazobactam) for synergistic therapeutic effects. The penicillin-induced breakdown of the bacterial cell wall makes it easier for gentamicin to reach its site of action inside the bacterial cell. Researchers have demonstrated decreased mortality from combination antibiotic therapy in treatment of infections due to Pseudomonas aeruginosa and other multidrug-resistant gram-negative bacilli.
Table 17.1 presents dosage information for gentamicin and the other aminoglycosides.
 TABLE 17.1
TABLE 17.1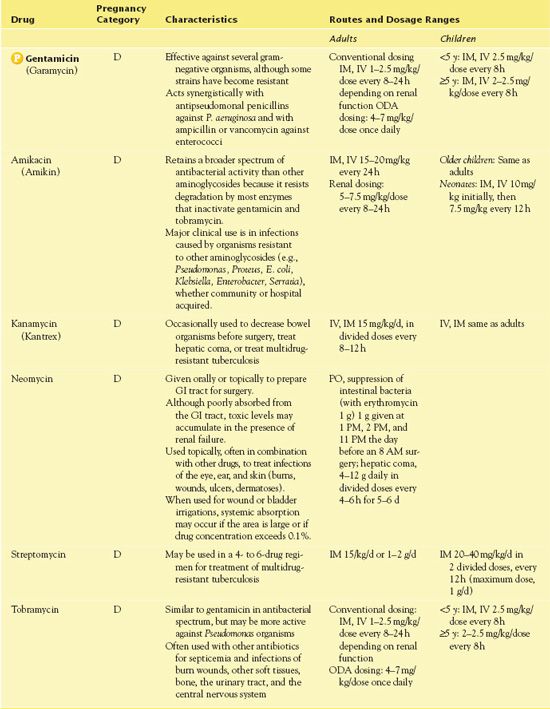
GI, gastrointestinal; IM, intramuscular; IV, intravenous; ODA, once-daily aminoglycoside
Use in Children
Caution is necessary when using gentamicin and other aminoglycosides in children. Individualization of the dose is extremely critical because of the low therapeutic index of the drug. Larger individual doses or more frequent dosing intervals may be necessary in certain clinical situations (cystic fibrosis). Initial doses of gentamicin in neonates and children are based on age. Serum levels should be obtained to assess the pharmacokinetic parameters to establish the frequency and dose of subsequent doses. It should be noted that the risk of nephrotoxicity and ototoxicity may be increased in neonates because of their immature renal function.
Use in Older Adults
As in children, individualized dosing of gentamicin is critical in older adults because of the low therapeutic index of the drug. Decreased renal function, other disease processes, and concurrent drug therapies increase the adverse effects in older adults, specifically aminoglycoside-induced nephrotoxicity and ototoxicity. Monitoring of renal function during treatment with gentamicin, as well as other aminoglycosides, is extremely important. Prolonged therapy (longer than 1 week) increases the risk of toxicity and should be avoided when possible.
Use in Patients With Renal Impairment
With impaired renal function, a reduction in dosage of aminoglycosides is essential. Gentamicin may accumulate in the serum and tissues of patients being treated with higher doses and for longer periods. Methods of adjusting dosage include lengthening the time between doses or reducing doses. For specific recommendations on adjusting aminoglycoside doses for renal impairment, nurses and other health care practitioners should consult references. In urinary tract infections, smaller doses can be used than in systemic infections because the aminoglycosides reach high concentrations in the urine.
Use in Patients With Hepatic Impairment
Gentamicin is appropriate for use in patients with hepatic impairment. No adjustment in dosage or frequency is indicated. However, it is necessary to continue to monitor plasma concentrations. Gentamicin should be used with caution in severe hepatic disease, such as cirrhosis, because of the possibility of precipitating hepatorenal syndrome.
Use in Patients With Critical Illness
Primary uses for gentamicin (in combination with other antibacterial agents) include serious infections caused by aerobic gram-negative bacilli that result in septicemia, nosocomial respiratory infections, complicated urinary tract infections and intra-abdominal infections, osteomyelitis, and endocarditis. The drug also demonstrates in vitro activity against methicillin-susceptible Staphylococcus aureus. Patients should not take gentamicin as monotherapy. Serious infections caused by Serratia, Pseudomonas, Citrobacter, Acinetobacter, and Enterobacter species warrant its use in combination with piperacillin/tazobactam, cefepime, meropenem, or imipenem/cilastatin. However, once susceptibilities to the identified organism are determined, prescribers usually discontinue aminoglycosides if a less toxic antibiotic may be used to complete the typical course of treatment. Because patients who are critically ill are at high risk for development of nephrotoxicity and ototoxicity with aminoglycosides, it is essential to follow guidelines for safe drug usage strictly.
Use in Patients Receiving Home Care
Administration of gentamicin does not typically occur in the home setting. However, instruction about IV care is essential for caregivers who are giving this medication at home. Potential for secondary infections is of concern.
Adverse Effects
Gentamicin and other aminoglycosides result in similar adverse reactions. A BLACK BOX WARNING ♦ alerts health care professionals that these drugs are nephrotoxic and ototoxic and must be used very cautiously in the presence of renal impairment.
A well-known adverse reaction associated with aminoglycoside therapy, nephrotoxicity, occurs more frequently in patients with a history of renal impairment. Extended duration of treatment with gentamicin may also contribute to nephrotoxicity. In most cases, nephrotoxicity is reversible on discontinuation of the drug. Ototoxicity (auditory or vestibular) may develop after extended use and may not be reversible. Dizziness, vertigo, tinnitus, and hearing loss may be signs of ototoxicity. Peripheral nephropathy, including numbness, skin tingling, and muscle twitching, also occurs. Therefore, use of gentamicin in patients with myasthenia gravis and other neuromuscular disorders warrants caution, because increased muscle weakness may occur.
Contraindications
Contraindications include a hypersensitivity to aminoglycosides. Prescribers generally reserve aminoglycosides are for infections that have not responded to less toxic drugs.
Nursing Implications
Dosage of aminoglycosides must be carefully monitored based on serum concentrations. Two major dosing schedules are used: one involving multiple daily doses (conventional dosing) and one involving a single daily dose (once-daily dosing, or once-daily aminoglycosides [ODA]). The use of ODA dosing, unless contraindicated, has replaced the common multiple daily dosing in many people. The ODA method uses higher doses (e.g., 4 to 7 mg per kg) to produce high initial drug concentrations, with no repeat dosing until the serum concentration is quite low (typically 24 hours later). The rationale for this dosing approach is a potential increase in efficacy with a reduced incidence of nephrotoxicity. Most patients can be successfully treated using ODA. However, ODA is not appropriate for certain people. In general, the following circumstances contraindicate its use: age of 18 years or less, pregnancy or postpartum status, and endocarditis.
The ODA dosing practice evolved from increased knowledge about the concentration-dependent bactericidal effects and postantibiotic effects of aminoglycosides. Concentration-dependent bactericidal effects mean that a large dose of aminoglycosides, with high peak serum concentrations, kills more microorganisms. Postantibiotic effects mean that aminoglycosides continue killing microorganisms even at low serum concentrations. Monitoring of random level (12-hour) serum evaluation in a single dosing regimen replaces traditional peak and trough serum monitoring.
With the multiple-dose regimen, a patient receives an initial loading dose, based on patient weight and the desired peak serum concentration, to achieve therapeutic serum concentrations rapidly. If the patient is obese, adjusted body weight should be used because aminoglycosides are not significantly distributed in body fat. In patients with normal renal function, recommended loading doses for selected aminoglycosides are the following:
• Gentamicin: 1 to 2.5 mg per kg
• Tobramycin: 1 to 2.5 mg per kg
• Amikacin: 5 to 7.5 mg per kg
Prescribers adjust dosages according to serum drug levels and creatinine clearance (CrCl). With conventional dosing, it is necessary to take gentamicin peak levels 30 minutes after the end of a 30 minute IV infusion or 1 hour after IM injection. The nurse ensures that trough levels are obtained immediately before the next dose is given. With ODA dosing, it is necessary to obtain a 12-hour random gentamicin level 12 hours after the start of the infusion.
Preventing Interactions
Many medications interact with gentamicin, increasing or decreasing its effects (Box 17.1). When patients who are taking agents that may lead to nephrotoxicity receive gentamicin, careful monitoring and caution are necessary. Caution is also warranted when administering diphenhydramine and chlor-pheniramine with gentamicin, because gentamicin may mask symptoms of ototoxicity. In addition, ginger may increase the effect of gentamicin by masking these effects. No herbs or foods appear to increase the effect of the drug.
BOX 17.1  Drug Interactions: Gentamicin
Drug Interactions: Gentamicin
Drugs That Increase the Effects of Gentamicin
 Acyclovir, amphotericin B, carboplatin and cisplatin, cyclosporine, ganciclovir, Pamidronate, salicylates, vancomycin
Acyclovir, amphotericin B, carboplatin and cisplatin, cyclosporine, ganciclovir, Pamidronate, salicylates, vancomycin
Increase the risk of nephrotoxicity
 Loop diuretics
Loop diuretics
Increase the risk of nephrotoxicity and ototoxicity
Drugs That Decrease the Effects of Gentamicin
 Penicillins
Penicillins
Decrease serum concentrations
The nurse should not mix penicillins and aminoglycosides in a syringe or IV solution, or administer them via a Y-site, because the penicillin inactivates the aminoglycoside. If feasible, dose separation is ideal.
Administering the Medication
The nurse uses only the IV route of administration if possible, because IM injections may be erratic. If gentamicin is used concomitantly with a penicillin-class agent, it is necessary to administer the penicillin 1 hour before or after the gentamicin infusion. Gentamicin is available in an ophthalmic preparation, and other ophthalmics should be administered 10 minutes before or after the gentamicin preparation.
QSEN Safety Alert 



