Describe the allergic and immune disorders as well as organ transplantation in terms of etiology, pathophysiology, and clinical manifestations.
 Discuss characteristics and uses of major immunosuppressant drugs in autoimmune disorders and organ transplantation.
Discuss characteristics and uses of major immunosuppressant drugs in autoimmune disorders and organ transplantation.
 Describe the cytotoxic immunosuppressant agents in terms of prototype, action, use, adverse effects, contraindications, and nursing implications.
Describe the cytotoxic immunosuppressant agents in terms of prototype, action, use, adverse effects, contraindications, and nursing implications.
 Discuss the conventional antirejection agents in terms of prototype, action, use, adverse effects, contraindications, and nursing implications.
Discuss the conventional antirejection agents in terms of prototype, action, use, adverse effects, contraindications, and nursing implications.
 Describe the adjuvant drugs in terms of prototypes, indications and contraindications for use, major adverse effects, and administration.
Describe the adjuvant drugs in terms of prototypes, indications and contraindications for use, major adverse effects, and administration.
 Understand how to use the nursing process in the care of patients receiving immunosuppressant drugs.
Understand how to use the nursing process in the care of patients receiving immunosuppressant drugs.
Clinical Application Case Study
Sam Jones, a 35-year-old mechanic with type 1 diabetes mellitus and end-stage renal disease, received a renal transplant from a living donor 2 years ago. To prevent organ rejection, he is currently taking cyclosporine, mycophenolate mofetil, and prednisone daily. He has monthly appointments at the nephrology clinic and has serum trough levels for cyclosporine measured before each visit. A month ago, Mr. Jones was hospitalized and received four infusions of muromonab-CD3 for an acute organ rejection reaction.
KEY TERMS
Autoantigens: protein complexes on a person’s own tissue that stimulate an abnormal immune reaction
Autoimmune disorders: conditions associated with an abnormal immune response to self-antigens (autoantigens) on body tissue, resulting in ongoing inflammation and damage to body tissues
Cytotoxic: causing cell death
Graft rejection reaction: activated immunological response by the recipient to graft donor organ cells resulting in graft tissue damage and loss of graft organ function
Graft-versus-host disease: complication of bone marrow or stem cell transplantation where activated T cells in donor bone marrow attack host tissues producing inflammatory changes in the skin, liver, and gastrointestinal tract; also can occur infrequently with a blood transfusion
Immunosuppression: suppression of the immune system
Monoclonal antibody: immunoglobulin therapeutically replicated in laboratory cells to react with a specific cell antigen altering the immune response to that antigen
Murine antibodies: immunoglobulins created in mouse cells for use as therapeutic treatment for human diseases
Polyclonal antibody: mixtures of antibodies (IgA, IgD, IgE, IgG, and IgM) produced by several clones of B lymphocytes
Introduction
The immune response, normally a protective process, recognizes and destroys potentially harmful outside substances, helping the body defend itself against disease. However, disease processes can also develop when the immune system perceives a harmless substance, such as an antigen or the person’s own body tissues, as foreign and tries to eliminate them. This inappropriate activation of the immune response is a major factor in allergic conditions (e.g., allergic asthma) and autoimmune disorders (e.g., rheumatoid arthritis, Crohn’s disease, psoriasis). Autoimmune disorders occur when a person’s immune system loses its ability to differentiate self from nonself. As a result, an immune response against host tissues occurs.
An appropriate, but undesirable, immune response also occurs when foreign tissue from another organism is transplanted into the body. With transplant therapy, if the immune response is not suppressed, a graft rejection reaction occurs, where the body reacts to the implanted cells as with other antigens and attempts to destroy the foreign tissue. Although numerous advances have been made in transplantation technology, the ability to modulate the immune response remains a major factor in determining the success or failure of transplant therapy.
Immunosuppressant drugs are used to decrease an undesirable immune response by interfering with the production or function of immune cells and cytokines that contribute to tissue inflammation and damage. Drugs used therapeutically as immunosuppressants constitute a diverse group, some of which also are used for other purposes. Drug groups that are used to reduce the immune response include corticosteroids (see Chap. 15) and some cytotoxic (causing cell death) antineoplastic drugs (see Chap. 12). Health care providers use these drugs, discussed here in relation to their effects in modulating the body’s response to autoimmune disorders or organ transplantation, to treat inflammatory autoimmune disorders or to prevent or treat transplant rejection reactions. These drugs are the main focus of this chapter. To aid in the understanding of immunosuppressant drugs, descriptions of selected inflammatory autoimmune disorders, tissue transplantation, and rejection reactions appear below.
Overview of Altered Immune Function
Etiology
In healthy people, the immune system’s ability to inherently differentiate between cell surface proteins on its own cells (called self-antigens or autoantigens) and antigens on foreign cells provides protection against disease. However, in people who have received an organ transplant, this protective mechanism must be altered to avoid damage to the transplant and organ rejection. Drug therapy to suppress the body’s ability to recognize self from nonself is a major part of transplantation protocols.
Tissue and organ transplantation involves replacing diseased host tissue with healthy donor tissue. The goal of such treatment is to save and enhance the quality of the recipient’s life. Skin grafts and kidney transplants are commonly performed, and heart, lung, liver, pancreas, and bone marrow/stem cell transplants are increasing. The use of biological agents, which stimulate the production of hematopoietic stem cells from bone marrow and mobilize them into circulating blood, has helped improve the availability of stem cells for transplant, reducing the need for bone marrow transplants.
Although many factors affect graft survival, including the degree of matching between donor tissues and recipient tissues, drug-induced immunosuppression is a major part of transplantation protocols. The goal is to provide adequate immunosuppression while minimizing adverse effects on normal body tissue. If immunosuppression is inadequate, a graft rejection reaction will occur with solid organ transplantation, and graft-versus-host disease (GVHD) will develop with bone marrow/stem cell transplantation. If immunosuppressive drug therapy is excessive, serious infection may occur, some malignancies such as lymphomas and skin cancers may develop, and organ damage related to the proliferation of activated lymphocytes in normal body cells may result.
Pathophysiology
After self-antigens develop, the tissue containing them is perceived as foreign and antigenic, triggering an inappropriate immune response that may involve T lymphocytes in direct destruction of tissue, as well as the production of proinflammatory cytokines, chemical messengers that attract and activate phagocytes contributing to the inflammatory immune process. Stimulation of B lymphocytes to produce antibodies leads to further inflammation and tissue damage.
Knowledge about the role of inflammatory cells and cytokines in the immune response to tissue injury continues to expand. This has led to the development of biological agents that can modulate inflammatory cytokine production by activated lymphocytes. Cytokines act as messengers between different types of lymphocytes to increase or decrease the immune response, modifying the production and activity of different white blood cells. Attachment of an antigen to an antigen-presenting cell activates macrophages to produce interleukin-1 (IL-1) and T cells to produce IL-2. Lymphocyte activation by IL-1 causes the activated lymphocytes and other immune cells to produce more IL-2 receptors, amplifying the immune response. IL-2 activates production and promotes the activity of cytotoxic T cells, macrophages, natural killer (NK) cells, and B lymphocytes. Hence, decreasing IL-2 production induces lymphocyte apoptosis, reducing the numbers of T lymphocytes available to participate in an immune response.
Another inflammatory mediator mediating the inflammatory process of autoimmune disease is tumor necrosis factor (TNF)-alpha, a cytokine that plays a major role in the response to infection. Functions of TNF include activation of monocytes, macrophages, and cytotoxic T cells; enhancement of NK cell functions; increased leukocyte movement into areas of tissue injury; increased phagocytosis by neutrophils; and stimulation of B and T lymphocytes. Although TNF can be beneficial in helping to fight infection, an excessive TNF response has been associated with the pathogenesis of autoimmune disorders. Overproduction of cytokines, such as IL-2 and TNF, contributes to prolonged tissue inflammation and damage in autoimmune disease.
In addition to the factors that activate an immune response, there are also factors that prevent the immune system from “turning off” an abnormal immune or inflammatory process. One of these factors may be a decrease in the number of suppressor T cells, which help modulate the immune response. Another factor may be inadequate amounts of anti-inflammatory cytokines (e.g., IL-10) to modulate the immune reaction.
A transplant rejection reaction occurs when the host’s immune system is stimulated to destroy the transplanted organ. The immune cells of the transplant recipient attach to the donor cells of the transplanted organ and react against the antigens in the donor organ. The rejection process involves T and B lymphocytes, antibodies, multiple cytokines, and inflammatory mediators. In most cases, T-cell activation and proliferation are more important initially in the rejection reaction than B-cell activation and the presence of active antibodies. Typically, during an organ rejection reaction, helper T cells become activated by donor antigen attachment to an antigen-presenting cell; the activated helper T cells then stimulate B cells to produce antibodies, leading to a delayed hypersensitivity reaction weeks or months later. The antibodies injure the transplanted organ by activating complement, producing antigen-antibody complexes or causing antibody-mediated tissue destruction. This reaction can destroy the solid organ graft within 2 weeks if the recipient’s immune system is not adequately suppressed by immunosuppressant drugs. Immunosuppressive drug therapy begins either immediately before or at the time of the transplant procedure to prevent antibody formation, and it must continue for life to prevent organ rejection.
Clinical Manifestations
Allergic Disorders
Allergic asthma is characterized by increased production of IgE in response to inhaled allergens. The IgE-allergen complexes trigger inflammation, producing airway edema and increasing mucus production. People use immunosuppressants to reduce the airway edema and excessive vascular permeability that accompany this type of asthma.
Barriers to Immunosuppressive Medication Adherence in High-Risk Adult Renal Transplant Recipients
by M. CONSTATINER, D. CUKOR
Dialysis and Transplantation
2011, 2, 60–65
Investigators identified two sets of barriers to adherence in a convenience sample of 94 postrenal transplant patients: (1) intentional omissions (too many pills or doses daily; perceived adverse effects related to the drugs) and (2) unintentional omission (forgetting doses, getting out of daily administration routine, lack of money to buy medications). Nurses can intervene to help patients improve adherence to posttransplant immunosuppressant medication by:
• Helping patients organize and set up a scheduled medication routine that is integrated with activities of daily living (e.g., meals, activities, bedtime)
• Using individualized cues and reminders to help the patient maintain their routine; a special medication container, prefilled by a pharmacist with a week of medications (e.g., Medisets); pill bottle alarm caps; environmental cues
• Making use of support by family and significant others to encourage ongoing compliance
• Helping the patient develop a plan to cope with and address common adverse effects
• Helping the patient to complete application forms for drug company assistance programs, as needed, to pay for medications
IMPLICATIONS FOR NURSING PRACTICE: Lack of adherence to immunosuppressant medication is a major factor in rejection reactions after transplant therapy. Nursing measures to assist patients with medication adherence can prevent organ loss and reduce patient morbidity and mortality after transplant therapy.
Immune Disorders
Crohn’s disease is a chronic, recurrent, inflammatory bowel disorder that can affect any area of the gastrointestinal (GI) tract. The chronic inflammation is attributed to a mixture of inflammatory mediators (e.g., IL-1 and –6, TNF-alpha) produced by overactivated macrophages in the lining of the bowel, which contribute to GI ulceration, bleeding, and diarrhea. The goal of treatment is to decrease inflammation and promote healing of bowel lesions.
Psoriasis, a hyperproliferative skin disorder, is characterized by an abnormal overproduction of skin cells, forming plaque lesions. Activated T lymphocytes producing cytokines are believed to stimulate the abnormal growth of the affected skin cells with accompanying inflammation from tissue infiltration of neutrophils and monocytes. Some medications (e.g., beta-blockers, lithium) may precipitate or aggravate psoriasis.
Psoriatic arthritis is a type of arthritis associated with psoriasis that is similar to rheumatoid arthritis. It may be characterized by extensive and disabling joint damage, especially in the hand and finger joints.
Rheumatoid arthritis occurs when an abnormal immune response leads to chronic inflammation and damage of joint cartilage and bone. It is thought to involve the activation of T lymphocytes, release of inflammatory cytokines, and formation of antibodies in the joint tissue as well as other organs. Research in recent years has delineated the roles of TNF-alpha and IL-1 in the pathophysiology of rheumatoid arthritis. Symptoms may include fatigue, loss of energy, lack of appetite, low-grade fever, muscle and joint aches, and stiffness. Joints frequently become red, swollen, painful, and tender.
Rejection Reactions With Solid Organ Transplantation
Rejection reactions may be either acute or chronic. Acute reactions may occur from 10 days to a few months after transplantation and mainly involve cellular immunity and proliferation of T lymphocytes. Characteristics include signs of organ failure and inflammation of blood vessels, leading to arterial narrowing or obliteration. Treatment with immunosuppressant drugs is usually effective in ensuring short-term survival of the transplant but does not prevent chronic rejection. Chronic reactions, which occur after months or years of normal function, are caused by both cellular and humoral immunity and do not respond to increasing immunosuppressive drug therapy. Characteristics include fibrosis of blood vessels and progressive failure of the transplanted organ.
Rejection reactions produce both general manifestations of inflammation and specific organ manifestations, depending on the organ involved. With renal transplantation, for example, acute rejection reactions produce fever, flank tenderness over the graft organ site, and symptoms of renal failure (e.g., increased serum creatinine, decreased urine output, edema, weight gain, hypertension). Chronic renal rejection reactions are characterized by a gradual increase in serum creatinine levels over 4 to 6 months. Along with observing for symptoms of decline in organ function, periodic organ tissue biopsies are often required to diagnose a chronic organ rejection process.
Bone Marrow/Stem Cell Transplantation and Graft-Versus-Host Disease
With bone marrow/stem cell transplantation, the donor marrow or stem cells, which contain T lymphocytes, develop an active immune response against antigens on the host’s tissues, producing GVHD. Tissue damage is produced directly by the action of cytotoxic T cells and indirectly through the release of inflammatory mediators (e.g., complement) and cytokines (e.g., TNF-alpha and ILs).
Acute GVHD occurs in 30% to 50% of patients, usually within 6 weeks of transplant. Signs and symptoms include delayed recovery of blood cell production in the bone marrow, skin rash, liver dysfunction (indicated by increased alkaline phosphatase, aminotransferases, and bilirubin), and diarrhea. The skin reaction is usually a pruritic maculopapular rash that begins on the palms and soles and may progress to cover the entire body. Liver involvement can lead to bleeding disorders and the development of hepatic encephalopathy.
Chronic GVHD occurs when symptoms persist or occur 100 days or more after transplantation. It is characterized by abnormal humoral and cellular immunity, severe skin disorders, and liver disease. Chronic GVHD appears to be an autoimmune disorder in which activated donor T cells continue to respond to the recipient’s surface proteins as if they are foreign antigens.
Drug Therapy
Immunosuppressant drugs compose several groups of pharmacological agents, with often overlapping mechanisms and sites of action (Table 11.1.; Fig. 11.1). Older groups of immunosuppressant drugs often depress the immune system of the recipient nonspecifically. Therapeutic use of these drugs increases the risk of serious infections with bacteria, viruses, fungi, or protozoa. In addition, most cytotoxic immunosuppressant drugs that slow the proliferation of activated lymphocytes also produce damage to rapidly dividing cells in other tissues (e.g., mucosal cells, intestinal cells, hematopoietic stem cells). As a result, serious, life-threatening complications can occur with the use of immunosuppressant agents. For example, patients with autoimmune disorders or organ transplants, who are receiving long-term immunosuppressant drug therapy, are at increased risk for serious infections, cancer (especially lymphoma), hypertension, renal and hepatic disease, and metabolic bone disease.
 TABLE 11.1
TABLE 11.1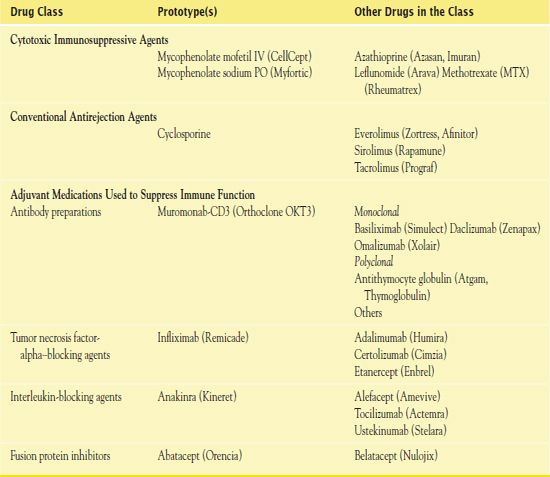
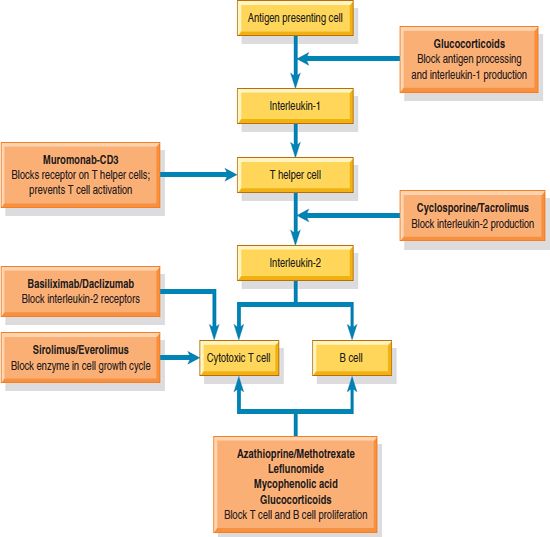
Figure 11.1 Activity of immunosuppressant drugs. Available immunosuppressants inhibit the immune response by blocking that response at various sites.
Ongoing research has helped develop drugs that modify the immune response more specifically in response to excessive levels of cytokines and T-cell activity that cause tissue damaging inflammation and autoimmune reactions. These drugs, called immunomodulators or biologic response modifiers, are part of the growing number of drugs with more specific immunosuppressive actions that have been developed through monoclonal antibody cloning technology. Most are used in combination with older immunosuppressants for synergistic effects with lower doses that minimize drug toxicities, whereas some are replacing the older, nonspecific immunosuppressants.
Immunosuppressants discussed here are cytotoxic immunosuppressant agents; conventional antirejection agents; and adjuvant medications, including antibody preparations, cytokine inhibitors, and corticosteroids.
NCLEX Success
1. After organ transplantation, immunosuppressants are given to prevent which of the following?
A. nephrotoxicity
B. hepatotoxicity
C. rejection reaction
D. bleeding disorders
2. The most common cancers that develop with long-term immunosuppression after organ transplant are
A. skin cancers and lymphomas
B. cancers of the gastrointestinal tract
C. renal and liver cancers
D. brain and spinal cord cancers
Cytotoxic Immunosuppressive Agents
Cytotoxic immunosuppressive drugs damage or kill dividing cells, such as immunologically competent lymphocytes. Health care providers use these drugs primarily in cancer chemotherapy (see Chap. 12). However, in smaller doses, some cytotoxic drugs also exhibit immunosuppressive activities and are useful in the treatment of autoimmune disorders and the prevention of rejection reactions in organ transplantation. For many years, azathioprine was the drug selected to induce immunosuppression and prevent rejection reactions to transplanted organs. Now,  mycophenolate mofetil (CellCept), the prototype in this discussion, has essentially replaced it.
mycophenolate mofetil (CellCept), the prototype in this discussion, has essentially replaced it.
Pharmacokinetics
Mycophenolate mofetil is a prodrug that, after oral or intravenous (IV) administration, is rapidly broken down to mycophenolic acid, the active component. Metabolism to an active metabolite occurs in the liver, finally resulting in inactive metabolites. Excretion takes place in the urine.
Action
Mycophenolate is an antimetabolite agent that interferes with the production of cellular deoxyribonucleic acid (DNA) and ribonucleic acid (RNA) and thus blocks cellular reproduction, growth, and development. As its active component, mycophenolic acid inhibits an enzyme needed for DNA synthesis and reduces the proliferation of lymphocytes.
Use
Uses of mycophenolate mofetil include the prophylaxis of organ rejection after cardiac, hepatic, and renal transplants, as well as immunosuppression after other solid organ transplant procedures involving the lung, pancreas, and small intestine. Mycophenolate sodium (Myfortic), an oral formulation, has received U.S. Food and Drug Administration (FDA) approval for use after kidney transplant to prevent organ rejection. Table 11.2. gives route and dosage information for mycophenolate and other cytotoxic immunosuppressant agents.
 TABLE 11.2
TABLE 11.2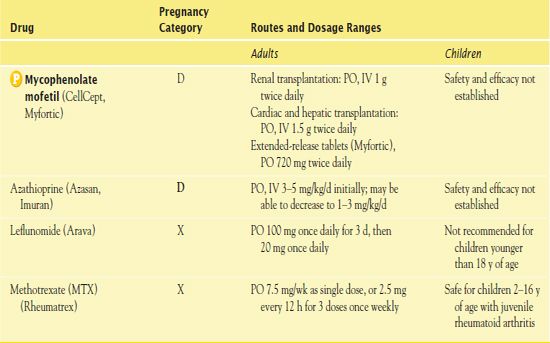
Use in Children
A few children undergoing renal transplantation have taken mycophenolate. In children with impaired renal function, recommended doses of mycophenolate may cause a high incidence of adverse effects. Thus, it is necessary to adjust the dosage for the renal function of the individual child.
Use in Older Adults
Mycophenolate has similar therapeutic and adverse effects in older adults compared with younger adults. However, because older adults often have multiple disorders and decreased organ function, it is especially important that drug choices, dosages, and monitoring tests be individualized.
Use in Patients With Renal Impairment
Mycophenolate produces higher plasma levels in renal transplant recipients with severe renal impairment than in patients with less severe renal impairment (and in healthy volunteers). It is important to avoid doses higher than 1 g twice a day in these patients.
Use in Patients With Hepatic Impairment
Liver impairment may interfere with metabolism, increasing drug half-life.
Use in Patients Receiving Home Care
With patients who are taking mycophenolate and other immunosuppressant drugs, a major role of the home care nurse is to assess the environment for potential sources of infection, assist patients and other members of the household to understand the patient’s susceptibility to infection, and teach ways to decrease risks of infection. Although infections often develop from the patient’s own body flora or reactivation of a latent infection, other potential sources include people with infections, caregivers, water or soil around live plants, and raw fruits and vegetables. Attention to environmental cleansing as well as good personal and hand hygiene is required with immunosuppressant therapy. In addition, the nurse may need to assist with setting up a medication schedule and scheduling clinic visits for monitoring and follow-up care.
The home care nurse also assesses the patient’s ability to safely self-administer the medications as prescribed, monitors for adverse drug effects, and observes for signs of drug toxicity. Drug interactions with drugs from multiple prescribers as well as drug–nutrient and drug–herbal interactions can all have an impact on the patient’s response to immunosuppressant drug therapy.
Adverse Effects
Common GI adverse effects of mycophenolate include nausea, vomiting, and diarrhea. The most serious risks associated with the use of this drug and some other immunosuppressant drugs are infection and increased risk of malignancy. Latent infections with the tuberculosis bacillus or hepatitis B virus may become active infections during immunosuppressant therapy.
Contraindications
Use of cytotoxic immunosuppressant drugs is not recommended during pregnancy or lactation. The FDA has issued a BLACK BOX WARNING ♦ for mycophenolate mofetil regarding the risk of fetal loss and malformations. Women of childbearing age must use contraception. A negative pregnancy test for such women is required prior to starting therapy. Contraceptive counseling for patients of both sexes is recommended prior to treatment and for several months after stopping treatment.
Nursing Implications
Preventing Interactions
Several drugs can increase and decrease the effects of mycophenolate, increasing or decreasing its effects (Box 11.1). Herbal preparations such as alfalfa, echinacea, ginseng, and bee venom, which potentially stimulate immune function, may interfere with mycophenolate and other immunosuppressant drug activity; thus, it is necessary to avoid them during therapy.
BOX 11.1  Drug Interactions: Mycophenolate Mofetil
Drug Interactions: Mycophenolate Mofetil
Drugs That Increase the Effects of Mycophenolate Mofetil
 Acyclovir, ganciclovir, probenecid, salicylates
Acyclovir, ganciclovir, probenecid, salicylates
Decrease excretion
Drugs That Decrease the Effects of Mycophenolate Mofetil
 Antacids containing magnesium, aluminum, and calcium; cholestyramine
Antacids containing magnesium, aluminum, and calcium; cholestyramine
Decrease absorption as drug binds with mycophenolate
Administering the Medication
QSEN Safety Alert 
It is necessary to handle immunosuppressant drugs such as mycophenolate with care to avoid direct contact with skin or mucous membranes. Such contacts have produced teratogenic effects in animals. Patients should swallow oral tablets or capsules whole, without crushing or altering them. They should avoid inhaling the powder from the capsules.
For best absorption, it is important to take oral mycophenolate on an empty stomach.
To ensure correct dosing, it is important to measure oral mycophenolate solution carefully using an accurate measuring device.
Assessing for Therapeutic Effects
After organ transplant, the absence of signs and symptoms of a rejection reaction is evidence of the therapeutic effects of mycophenolate immunosuppressive therapy. (Inflammatory changes in the organ tissue along with laboratory evidence of organ impairment usually accompany acute rejection reactions.) Periodic organ tissue biopsy is used to evaluate for signs of chronic rejection reaction.
Assessing for Adverse Effects
A primary focus for nursing assessment is evidence of signs of infection, including fever, chills, sore throat, headache, swollen glands, cough, and urinary burning or frequency. Following organ transplant surgery, patients often take prophylactic antimicrobials for the first 3 to 6 months to prevent opportunistic infections. Wound healing may be slower during cytotoxic drug therapy with suppression of the normal inflammatory response.
Nursing care includes assessment of GI symptoms, oral intake, elimination pattern, fluid and electrolyte balance, and weight changes. Skin assessment for signs of rash, bruising, petechiae, and color changes such as pallor or jaundice of the skin or sclera offers important clues to allergic or hematological complications and hepatotoxicity. Laboratory monitoring of the complete blood count (CBC), renal function tests, and liver function tests performed prior to therapy and periodically during treatment limits the potential for bone marrow suppression and potential hepatotoxicity.
Clinical Application 11-1
At his office visit, Mr. Jones tells the nurse he has been regularly attending his son’s Little League baseball games at a local park. What self-care measures related to his long-term need for immunosuppressive drug therapy should the nurse recommend?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


