Identify effects produced by stimulation of alpha- and beta-adrenergic receptors.
 Discuss use of epinephrine to treat anaphylactic shock, cardiac arrest, and acute bronchospasm.
Discuss use of epinephrine to treat anaphylactic shock, cardiac arrest, and acute bronchospasm.
 Identify patients at risk for the adverse effects associated with adrenergic drugs.
Identify patients at risk for the adverse effects associated with adrenergic drugs.
 List commonly used over-the-counter preparations and herbal preparations that contain adrenergic drugs.
List commonly used over-the-counter preparations and herbal preparations that contain adrenergic drugs.
 List characteristics of adrenergic drugs in terms of etiology, pathophysiology, and clinical manifestations, along with pharmacokinetics, action, use, adverse effects, contraindications, and nursing implications in use of adrenergic agents.
List characteristics of adrenergic drugs in terms of etiology, pathophysiology, and clinical manifestations, along with pharmacokinetics, action, use, adverse effects, contraindications, and nursing implications in use of adrenergic agents.
 Discuss using adrenergic drugs in special patient populations.
Discuss using adrenergic drugs in special patient populations.
 Teach patients about safe, effective use of adrenergic drugs.
Teach patients about safe, effective use of adrenergic drugs.
 Describe signs and symptoms of toxicity due to noncatecholamine adrenergic drugs and how to treat this condition.
Describe signs and symptoms of toxicity due to noncatecholamine adrenergic drugs and how to treat this condition.
 Understand the nursing process for using adrenergic drugs.
Understand the nursing process for using adrenergic drugs.
Clinical Application Case Study
Abe Sobechenko, a 71-year-old man, has chronic obstructive pulmonary disease (COPD). He has had asthma for all of his adult life and is admitted to the hospital with acute respiratory distress secondary to pneumonia. Although he has never been a smoker, he worked as a welder for 45 years. He has a very modest pension and has Medicare for health insurance, which sometimes makes it difficult for him to pay for all his medical supplies and medications.
KEY TERMS
Adrenergic drug: agent that produces effects similar to those produced by stimulation of the sympathetic nervous system and therefore has widespread effects on body tissues
Adrenergic receptor: structure that is activated by adrenaline-like compound
 Alpha1: found on surface membranes of target tissues and organs; mainly postsynaptic
Alpha1: found on surface membranes of target tissues and organs; mainly postsynaptic
 Alpha2: found on surface membranes of target tissues and organs; mainly presynaptic
Alpha2: found on surface membranes of target tissues and organs; mainly presynaptic
 Beta: found in heart muscle, which cause increased heart rate and contractility, and in the kidney, which promote the release of renin from the kidney
Beta: found in heart muscle, which cause increased heart rate and contractility, and in the kidney, which promote the release of renin from the kidney
Anaphylaxis: type I immunoglobulin E-mediated allergic reaction to a foreign substance (antigen) that has entered the body; occurs on second or subsequent exposure to an antigen. Symptoms develop rapidly; typical symptom onset ranges from 30 minutes to 2 hours after exposure to the antigen
Antigen: foreign substance
Decongestant: agent that reduces nasal congestion by decreasing the blood flow to the upper respiratory tract and decreasing the overproduction of secretions
Neurotransmitter: chemical substance that carries messages from one neuron to another, or from a neuron to other body tissues, such as cardiac or skeletal muscle
Postsynaptic: situated behind or occurring after a synapse
Pressor: effect that increases the blood pressure
Presynaptic: situated in front of or occurring before a synapse
Vasopressor: substance that increases the blood pressure
Introduction
Adrenergic drugs produce effects similar to those produced by stimulation of the sympathetic nervous system and therefore have widespread effects on body tissues. Major therapeutic uses and adverse effects of adrenergic medications derive from drug action on the heart, blood vessels, and lungs. Some adrenergic drugs are exogenous formulations of naturally occurring neurotransmitters and hormones, such as norepinephrine, epinephrine, and dopamine. Other adrenergic medications, such as phenylephrine, pseudoephedrine, and isoproterenol, are synthetic chemical relatives of naturally occurring neurotransmitters and hormones.
Specific effects of adrenergic medications depend mainly on the type of adrenergic receptor activated by the drug. Adrenergic receptors are those responses that are activated by adrenaline-like compounds. The drugs discussed in this chapter (e.g., epinephrine, pseudoephedrine, isoproterenol, phenylephrine) affect multiple adrenergic receptors and have many clinical uses. Other adrenergic drugs are more selective for specific adrenergic receptors or are given topically to produce more localized therapeutic effects and thus have fewer systemic adverse effects. These drugs have relatively restricted clinical indications and are discussed more extensively elsewhere (Chap. 29, Drug Therapy for Nasal Congestion; Chap. 31, Drugs for Asthma and Bronchoconstriction; and Chap. 57, Drug Therapy for Disorders of the Eye).
Overview of the Adrenergic Response
Physiology: Adrenergic Receptors
For the most part, adrenergic drugs interact directly with postsynaptic alpha1– or beta-adrenergic receptors on the surface membrane of target organs and tissues (Fig. 27.1). Alpha1-adrenergic receptors are receptors on surface membranes of target tissues and organs, which are mainly postsynaptic. The beta-adrenergic receptors reside in heart muscle, which causes increased heart rate and contractility, and in the kidneys, which promotes the release of renin from the kidney. The drug–receptor complex then alters the permeability of the cell membrane to ions or extracellular enzymes. The influx of these molecules stimulates intracellular metabolism and production of other enzymes, structural proteins, energy, and other products required for cell function and reproduction. Epinephrine, isoproterenol, norepinephrine, and phenylephrine are examples of direct-acting adrenergic drugs.
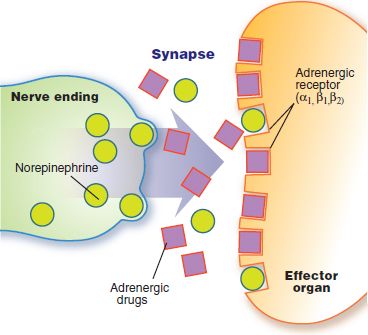
Figure 27.1 Mechanism of direct adrenergic drug action. Adrenergic drugs interact directly with postsynaptic alpha1 and beta receptors on target effector organs, activating the organ in a similar fashion as the neurotransmitter norepinephrine.
Some adrenergic drugs exert indirect effects on postsynaptic adrenergic receptors. Postsynaptic means situated behind or occurring after a synapse. Indirect adrenergic effects may be produced by drugs such as amphetamines, which increase the amount of norepinephrine released into the synapse from storage sites in nerve endings (Fig. 27.2A). Norepinephrine then stimulates the alpha and beta receptors, producing sympathetic effects in the body. Inhibition of norepinephrine reuptake from the synapse is another mechanism that produces indirect adrenergic effects. Remember that norepinephrine reuptake is the major way that sympathetic nerve transmission is terminated. Drugs such as tricyclic antidepressants and cocaine block norepinephrine reuptake, resulting in stimulation of alpha- and beta-adrenergic receptors (Fig. 27.2B).
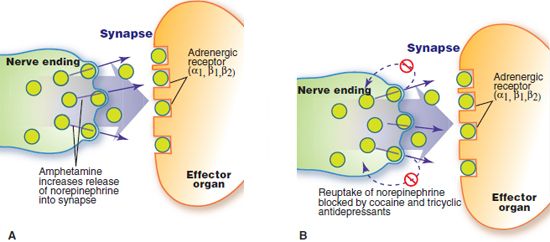
Figure 27.2 Mechanisms of indirect adrenergic drug action. Stimulation of postsynaptic alpha1, beta1, and beta2 receptors results from adrenergic medications that act indirectly, increasing the release of norepinephrine into the synapse (A) or inhibiting the reuptake of norepinephrine from the synapse (B).
Other adrenergic drugs are called mixed-acting drugs. They directly stimulate adrenergic receptors by binding to them and indirectly stimulate adrenergic receptors by increasing the release of norepinephrine into synapses. Ephedrine and pseudoephedrine are examples of mixed-acting adrenergic drugs.
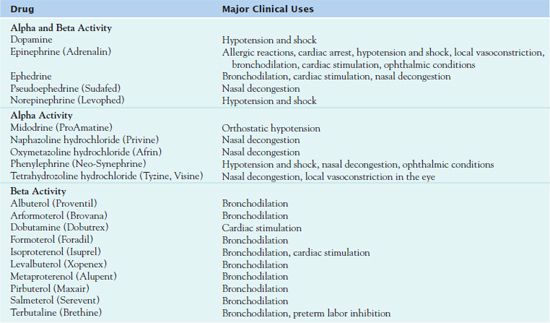
Because many body tissues have both alpha and beta receptors, the effect produced by an adrenergic drug depends on the type of receptor activated and the number of affected receptors in a particular body tissue. Some adrenergic drugs are nonselective, acting on both alpha and beta receptors. Other medications are more selective, acting only on certain subtypes of receptors. Table 27.1 groups commonly used adrenergic drugs by adrenergic receptor activity and gives their clinical use.
Pathophysiology of the Adrenergic Response
The effect produced by an adrenergic drug depends on the type of receptor activated and the number of affected receptors in a particular part of the body. The predominant effect in response to activation of alpha1 receptors is vasoconstriction of blood vessels, which increases the blood pressure. This is sometimes referred to as a pressor (or vasopressor) effect. Alpha1-activated vasoconstriction of blood vessels in nasal mucous membranes decreases nasal congestion, leading to a decongestant effect. Other adrenergic effects resulting from alpha1 activation include mydriasis, contraction of gastrointestinal (GI) and genitourinary sphincters, and elevated blood glucose.
The predominant effect in response to activation of beta1 receptors in the heart is cardiac stimulations. Beta1 activation causes increased force of myocardial contraction, or a positive inotropic effect; increased heart rate, or a positive chronotropic effect; and increased speed of electrical conduction in the heart, or a positive dromotropic effect. Another adrenergic effect resulting from beta1 activation is increased renin secretion from the kidneys.
The predominant clinical effect in response to activation of beta2 receptors is bronchodilation. Activation of beta2 receptors in blood vessels causes vasodilation and increased blood flow to the heart, brain, and skeletal muscles, tissues needed for the “fight-or-flight” sympathetic response. Beta2 activation also results in hepatic glycogenolysis and gluconeogenesis and decreased pancreatic insulin secretion, leading to hyperglycemia. Other adrenergic effects resulting from beta2 activation include relaxation of smooth muscle in the uterus, urinary bladder, and GI tract.
Activation of beta3-adrenergic receptors produces lipolysis and increased release of free fatty acids into the blood.
Drugs that activate alpha2 receptors on presynaptic nerve fibers do not produce a sympathetic effect. Alpha2 receptors are located on surface membranes of target tissues and organs and are mainly presynaptic. Presynaptic is defined as situated in front of or occurring before a synapse. These drugs inhibit the release of the neurotransmitter norepinephrine into synapses of the sympathetic nervous system, thus exerting an antiadrenergic response in the body. Neurotransmitters are chemical substances that carry messages from one neuron to another or from a neuron to other body tissues, such as cardiac or skeletal muscle.
Although activation of presynaptic alpha2 receptors in the periphery are not of clinical significance, activation of these receptors in the central nervous system (CNS) by medications is useful in treating hypertension (see Chap. 28).
Drug Therapy
The usefulness of adrenergic drugs stems mainly from the drugs’ effects on the heart, blood vessels, and bronchi. They are often used as emergency drugs in the treatment of acute cardiovascular and respiratory collapse. In addition, adrenergic drugs are useful in the treatment of allergic reactions. Patients who benefit from these drugs include those in need of restoration of blood pressure in reversing types of hypotensive states.
Some of the pathophysiological states where adrenergic drugs are used include cardiac arrest, Stokes-Adams syndrome (sudden attacks of unconsciousness caused by heart block), and profound bradycardia. These drugs may be used as cardiac stimulants. In hypotension and shock, they may be used to increase blood pressure. In hemorrhagic or hypovolemic shock, the drugs are second-line agents that may be used if adequate fluid volume replacement does not restore sufficient blood pressure and circulation to maintain organ perfusion.
In bronchial asthma and other obstructive pulmonary diseases, adrenergic drugs are used as bronchodilators to relieve bronchoconstriction and bronchospasm. In upper respiratory infections, including the common cold and sinusitis, they may be given orally or applied topically to the nasal mucosa to reduce nasal congestion (decongestant effect).
Adrenergic drugs are useful in treating a variety of symptoms of allergic disorders. Severe allergic reactions are characterized by hypotension, bronchoconstriction, and laryngoedema. As vasoconstrictors, the drugs are useful in correcting the hypotension that often accompanies severe allergic reactions. The drug-induced vasoconstriction of blood vessels in mucous membranes produces a decongestant effect to relieve edema in the respiratory tract, skin, and other tissues. As bronchodilators, the drugs also help relieve the bronchospasm of severe allergic reactions. Adrenergic drugs may be used to treat allergic rhinitis, acute hypersensitivity (anaphylactic reactions to drugs, animal serums, insect stings, and other allergens), serum sickness, urticaria, and angioneurotic edema.
Other clinical uses of adrenergic drugs include relaxation of uterine musculature and inhibition of uterine contractions in preterm labor. They also may be added to local anesthetics for their vasoconstrictive effect, thus preventing unwanted systemic absorption of the anesthetic; prolonging anesthesia; and reducing bleeding. Topical uses include application to skin and mucous membranes for vasoconstriction and hemostatic effects and to the eyes for vasoconstriction and mydriasis.
Adrenergic Drugs
The adrenergic drugs have different predominant properties: alpha activity, beta activity, and alpha and beta activity. Those drugs with alpha and beta activity include dopamine, epinephrine, ephedrine, pseudoephedrine, and norepinephrine. The condition the patient has determines which adrenergic drug, with its specific effect, is necessary for treatment. Table 27.2 presents dosing recommendations for these drugs.
 TABLE 27.2
TABLE 27.2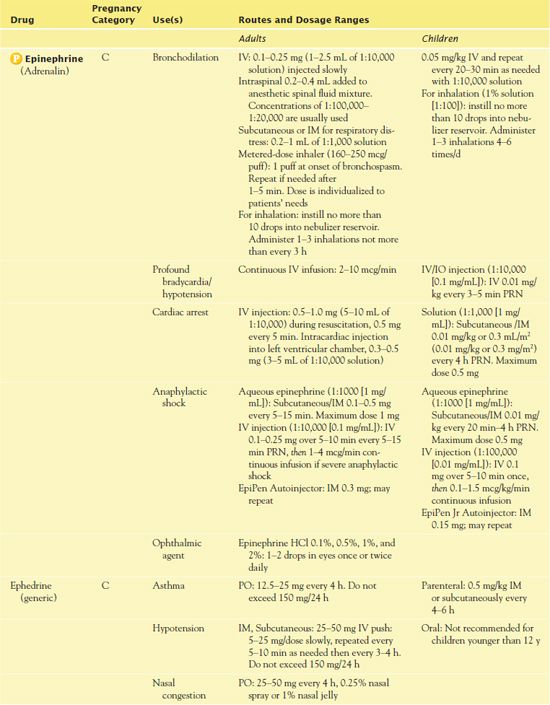
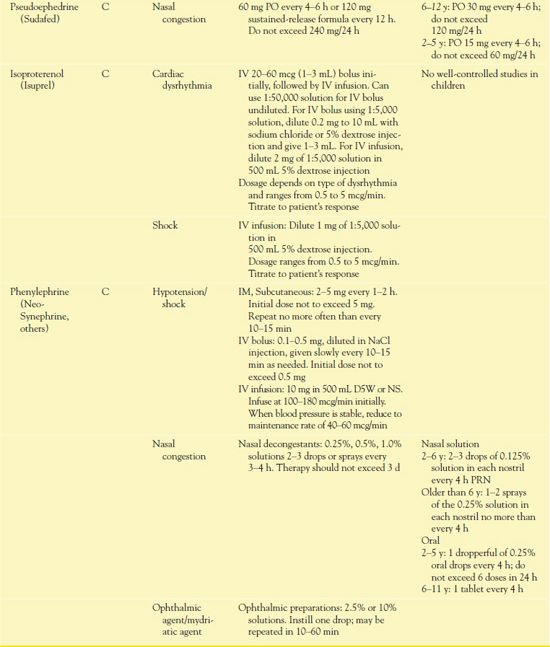
D5W, dextrose 5% in water; NS, 0.9% sodium chloride.
 Epinephrine is the prototype adrenergic drug. When it is given systemically, the effects may be therapeutic or adverse, depending on the reason for use; dosage; and route of administration. Epinephrine stimulates alpha1 and all beta receptors. At usual doses, beta-adrenergic effects on the heart and vascular and other smooth muscles predominate. However, at high doses, alpha1-adrenergic effects (e.g., vasoconstriction) predominate.
Epinephrine is the prototype adrenergic drug. When it is given systemically, the effects may be therapeutic or adverse, depending on the reason for use; dosage; and route of administration. Epinephrine stimulates alpha1 and all beta receptors. At usual doses, beta-adrenergic effects on the heart and vascular and other smooth muscles predominate. However, at high doses, alpha1-adrenergic effects (e.g., vasoconstriction) predominate.
Pharmacokinetics
Epinephrine is administered through various routes: subcutaneously, intramuscularly, intravenously, via inhalation, and even as eye drops. The subcutaneous route has an onset of 5 to 10 minutes, with a peak of 20 minutes and a duration of 20 to 30 minutes. The intramuscular route has an onset of 5 to 10 minutes, a peak in 20 minutes, and a duration of 20 to 30 minutes, the same as the subcutaneous route. The intravenous (IV) route has an instant onset, a peak of 20 minutes, and a duration of 20 to 30 minutes. The inhalation route has an onset is 3 to 5 minutes, a peak of 20 minutes, and a duration of 1 to 3 hours. Finally, administration via eye drops has an onset of less than 1 hour, a peak in 4 to 8 hours, and a duration of 24 hours. Most epinephrine is rapidly metabolized in the liver to inactive metabolites, which are then excreted in the urine. The remaining epinephrine is deactivated by reuptake at synaptic receptor sites.
The nurse should note that when given by injection, epinephrine acts rapidly but has a short duration of action. The IV form acts almost immediately to produce an increase in blood pressure; a positive inotropic and positive chronotropic effect on the myocardium; hyperglycemia; bronchodilation; and vasoconstriction of arterioles in the skin, mucosa, and most viscera. For acute asthma attacks, subcutaneous administration of epinephrine usually produces bronchodilation within 5 to 10 minutes; maximal effects may occur within 20 minutes.
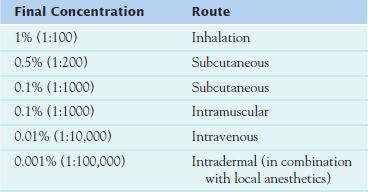
Table 27.3 lists the numerous epinephrine solutions available. Solutions vary widely in the amount of drug they contain. They must be used correctly to avoid potentially serious hazards.
Action
Epinephrine is a naturally occurring neurotransmitter, the effects of which are mediated by alpha or beta receptors in specific organs. Effect on alpha receptors includes vasoconstriction, including contraction of dilator muscles of the iris. The effects on the beta receptors include positive chronotropic and inotropic effects on the heart at the beta1 receptors; bronchodilation, vasodilation, and uterine relaxation of the beta2 receptors; and decreased production of aqueous humor.
Use
Epinephrine is the adrenergic drug of choice for relief of anaphylactic shock, the most serious allergic reaction, as well as treatment of cardiac arrest. In addition, epinephrine is used as an additive to local anesthetics for vasoconstrictive effects, which include prolonging the action of the local anesthetic drug, preventing systemic absorption, and minimizing bleeding. Adrenergic drugs are given intravenously only for emergencies, such as anaphylactic shock, cardiac arrest, severe arterial hypotension, and circulatory shock. Because adrenergic drugs are often used in medical crises, they must be readily available in all health care settings (e.g., hospitals, long-term care facilities, physicians’ offices). All health care personnel should know where emergency drugs are stored.
Use in Specific Disorders
Anaphylaxis
Anaphylactic shock or anaphylaxis is a type I immunoglobulin E-mediated allergic reaction to an antigen, a foreign substance that has entered the body. Some typical antigens include foods (e.g., shellfish, peanuts, eggs), medications (e.g., penicillin, vaccinations, enzymes, iodine-contrast media), and insect bites or stings (e.g., bees, ants). During an anaphylactic reaction, mast cells release chemical mediators such as histamine, serotonin, platelet-activating factor, prostaglandins, and leukotrienes. The resulting increased capillary permeability and smooth muscle contraction lead to edema, bronchospasm, and airway obstruction. Vasodilation results in hypotension and shock. Anaphylactic reactions occur on second or subsequent exposure to an antigen. Symptoms develop rapidly; typical symptom onset ranges from 30 minutes to 2 hours after exposure to the antigen.
IV or subcutaneous epinephrine is the drug of choice for the treatment of anaphylaxis. The drug relieves bronchospasm, laryngeal edema, and hypotension. In conjunction with its alpha (vasoconstriction) and beta (cardiac stimulation, bronchodilation) effects, it acts as a physiologic antagonist of histamine and other bronchoconstricting and vasodilating substances released during anaphylactic reactions. People susceptible to severe allergic responses should carry a syringe of epinephrine at all times. EpiPen and EpiPen Jr are prefilled, autoinjection syringes for intramuscular self-administration of epinephrine in emergency situations (Fig. 27.3). The thigh is the preferred site for autoinjection, providing more rapid absorption and higher blood levels of epinephrine than the arm in children and adults for either intramuscular or subcutaneous administration. Victims of anaphylaxis who have been taking beta-adrenergic blocking drugs (e.g., propranolol [Inderal]) do not respond as readily to epinephrine as those not taking beta blockers. Larger doses of epinephrine and large amounts of IV fluids may be required.
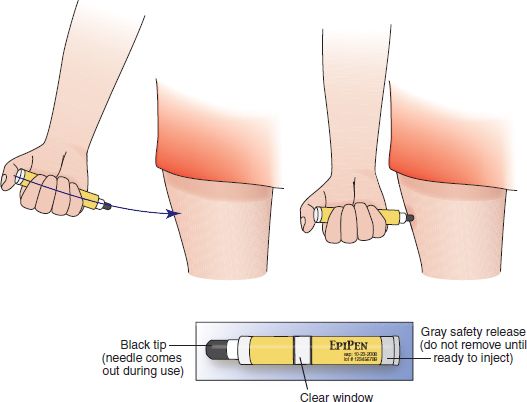
Figure 27.3 To use the EpiPen Autoinjector, grasp the unit in your first with the black tip pointing down. When ready to inject, activate the unit by removing the gray activation cap with your other hand. Firmly thrust the device into the outer thigh at a 90-degree angle and hold in place for several seconds. After removing the autoinjector, massage the injection site to enhance absorption. (Note: The injection can be made through clothing.)
Adjunct medications that may be useful in treating severe cases of anaphylaxis include corticosteroids, norepinephrine, and aminophylline. Antihistamines are considered secondline treatment; their usefulness is limited because histamine plays a minor role in causing anaphylaxis compared with leukotrienes and other inflammatory mediators. Antihistamines should never be used alone in the treatment of anaphylaxis. Diphenhydramine is often used as a second-line adjunctive treatment; however, studies show that a combination of ranitidine and diphenhydramine is more efficacious than diphenhydramine alone.
Clinical Application 27-1
Mr. Sobechenko receives piperacillin/tazobactam, a beta-lactam antibiotic, for treatment of his pneumonia. Within 15 minutes of the start of the antibiotic infusion, he has an anaphylactic reaction. He is agitated and flushed and complains of palpitations. He is having severe difficulty breathing due to bronchospasm. His physician then orders epinephrine.
 What are the nursing implications for this patient’s reaction to the antibiotic?
What are the nursing implications for this patient’s reaction to the antibiotic?
 What assessment is needed relative to the adverse effects of epinephrine?
What assessment is needed relative to the adverse effects of epinephrine?
Cardiopulmonary Resuscitation
Epinephrine is often administered during cardiopulmonary resuscitation (CPR). The most important action of epinephrine during cardiac arrest is constriction of peripheral blood vessels, which shunts blood to the central circulation and increases blood flow to the heart and brain. This beneficial effect comes at the expense of increased oxygen consumption by the myocardium, ventricular dysrhythmias, and myocardial dysfunction after resuscitation. Epinephrine is considered the drug of choice for the treatment of cardiac arrest in cases of nonventricular tachycardia/fibrillation such as asystole or pulseless electrical activity. Epinephrine is beneficial in these situations because it stimulates electrical and mechanical activity and produces myocardial contraction.
The specific effects of epinephrine depend largely on the dose and route of administration. The optimal dose in CPR has not been established. Advanced Cardiovascular Life Support (ACLS) guidelines recommend administering epinephrine 1 mg intravenously every 5 minutes.
Hypotension and Shock
In hypotension and shock, initial efforts involve identifying and treating the cause when possible. Such treatments include placing the patient in the recumbent position, blood transfusions, fluid and electrolyte replacement, treatment of infection, and use of positive inotropic drugs and other medications to treat heart failure. If these measures are ineffective in raising the blood pressure enough to maintain perfusion to vital organs such as the brain, kidneys, and heart, vasopressor drugs may be used. The usual goal of vasopressor drug therapy is to maintain tissue perfusion and a mean arterial pressure of at least 80 to 100 mm Hg.
Nasal Congestion
In nasal congestion, adrenergic drugs given topically or systemically constrict blood vessels in nasal mucosa and decrease the nasal congestion associated with the common cold, allergic rhinitis, hay fever, sinusitis, or other upper respiratory allergy. The topical nasal solutions of epinephrine are for the temporary relief from nasal and nasopharyngeal mucosal congestion due to these conditions. Topical agents are effective, undergo little systemic absorption, are available over the counter (OTC), and are widely used. However, overuse leads to decreased effectiveness (tolerance), irritation and ischemic changes in the nasal mucosa, and rebound congestion. These effects can be minimized by using small doses only when necessary and for no longer than 3 to 5 days.
Oral drugs have a slower onset of action than topical ones but may last longer. They also may cause more adverse effects, which may occur with usual therapeutic doses and are especially likely with high doses. The most problematic adverse effects are cardiac and CNS stimulation; the risks of hypertension and cerebral hemorrhage are greater in people with hypertension. Commonly used oral agents are pseudoephedrine and ephedrine.
Use in Children
Clinicians use adrenergic agents to treat asthma, hypotension, shock, cardiac arrest, and anaphylaxis in children. However, guidelines for safe and effective use of adrenergic drugs in children are not well established. Children are very sensitive to drug effects, including cardiac and CNS stimulation, and recommended doses usually should not be exceeded.
Prescribers mainly order epinephrine in children for treatment of bronchospasm due to asthma or allergic reactions. Parenteral epinephrine may cause syncope when given to asthmatic children. Isoproterenol is rarely given parenterally to children. There is little reason to use the inhalation route, because in children, as in adults, selective beta2 agonists such as albuterol are preferred for bronchodilation in asthma.
The most frequent use of phenylephrine is to relieve congestion of the upper respiratory tract and may be given topically, as nose drops. The nurse must carefully measure doses. Rebound nasal congestion occurs with overuse.
Use in Older Adults
It is necessary to use epinephrine with caution in the geriatric patient population. Clinicians use adrenergic agents to treat asthma, hypotension, shock, cardiac arrest, and anaphylaxis in older adults. These drugs stimulate the heart to increase rate and force of contraction and blood pressure. Because older adults often have chronic cardiovascular conditions (e.g., angina, dysrhythmias, heart failure, coronary artery disease, hypertension, peripheral vascular disease) that are aggravated by adrenergic drugs, careful monitoring by the nurse is required.
Prescribers often order adrenergic drugs as bronchodilators and decongestants in older adults. Therapeutic doses increase the workload of the heart and may cause symptoms of impaired cardiovascular function. Overdoses may cause severe cardiovascular dysfunction, including life-threatening dysrhythmias. The drugs also cause CNS stimulation. With therapeutic doses, anxiety, restlessness, nervousness, and insomnia often occur in older adults. Overdoses may cause hallucinations, convulsions, CNS depression, and death.
Adrenergics are ingredients in OTC asthma remedies, cold remedies, nasal decongestants, and appetite suppressants. Cautious use of these preparations is required in older adults. They should not take the drugs concurrently with prescription adrenergic drugs because of the high risk of overdose and toxicity.
Ophthalmic preparations of adrenergic drugs also require cautious use in the elderly. For example, phenylephrine acts as a vasoconstrictor and mydriatic. Applying larger-than- recommended doses to the normal eye or usual doses to the traumatized, inflamed, or diseased eye may result in sufficient systemic absorption of the drug to cause increased blood pressure and other adverse effects. The rationale for the caution in older adults is because of cardiac and CNS-stimulating effects of epinephrine.
Use in Patients With Renal Impairment
Epinephrine warrants cautious use in patients with renal failure. Adrenergic drugs exert effects on the renal system that may cause problems for patients with renal impairment. For example, adrenergic drugs with alpha1 activity cause constriction of renal arteries, thereby diminishing renal blood flow and urine production. These drugs also constrict urinary sphincters, causing urinary retention and painful urination, especially in men with prostatic hyperplasia.
The renal system eliminates many adrenergic drugs and their metabolites. In the presence of renal disease, these compounds may accumulate and cause increased adverse effects.
Use in Patients With Hepatic Impairment
Epinephrine administration has no reported precautions for use in patients with hepatic impairment. The liver is rich in the enzymes monoamine oxidase (MAO) and catecholamine O-methyl transferase (COMT), which are responsible for metabolism of circulating epinephrine and other adrenergic drugs (e.g., norepinephrine, dopamine, isoproterenol). However, other tissues in the body also possess these enzymes and are capable of metabolizing natural and synthetic catecholamines. Any unchanged drug can be excreted in the urine. Many noncatecholamine adrenergic drugs are excreted largely unchanged in the urine. Therefore, liver disease is not usually considered a contraindication to administering adrenergic drugs.
Use in Patients With Critical Illness
Adrenergic drugs are important emergency drugs. They are essential for treating hypotension, shock, asystole and other dysrhythmias, acute bronchospasm, and anaphylaxis. Although they may save lives of critically ill patients, use of adrenergic drugs may result in secondary health problems that require monitoring and intervention. These health problems include
• Possible diminished renal perfusion and decreased urine output due to vasopressor action
• Possible decreased perfusion to the liver, with subsequent liver damage due to vasopressor action
• Possible irritable cardiac dysrhythmias due to beta1 activity
• Possible increase in myocardial oxygen requirement due to beta1 activity
• Hyperglycemia, hypokalemia, and hypophosphatemia due to beta1 activity
• Severe hypertension and reflex bradycardia
• Tissue necrosis after extravasation
• Limb ischemia due to profound vasoconstriction



