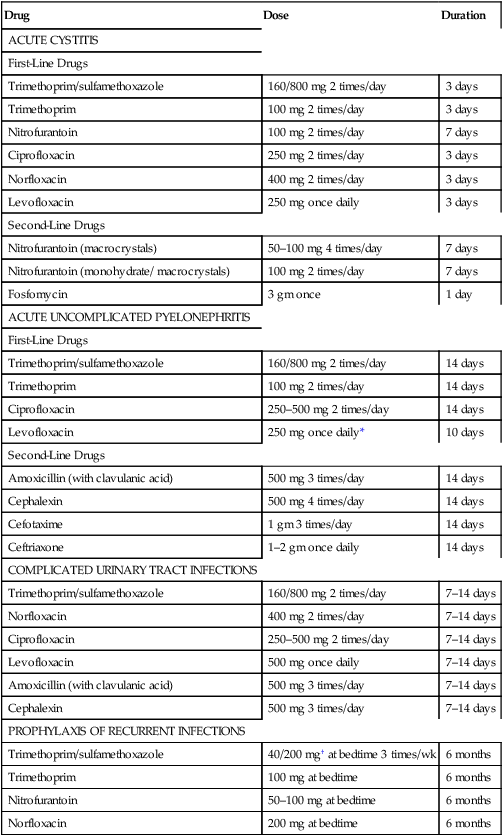
CHAPTER 89 In this section, we consider the characteristics and treatment of the major UTIs: acute cystitis, acute urethral syndrome, acute pyelonephritis, acute bacterial prostatitis, and recurrent UTIs. Most of these can be treated with oral therapy at home. The principal exception is severe pyelonephritis, which requires IV therapy in a hospital. Drugs and dosages for outpatient therapy in nonpregnant women are summarized in Table 89–1. TABLE 89–1 Regimens for Oral Therapy of Urinary Tract Infections in Nonpregnant Women *For infection due to E. coli without concurrent bacteremia. As indicated in Table 89–1, several drugs can be used for treatment. For uncomplicated cystitis, trimethoprim/sulfamethoxazole and nitrofurantoin are drugs of first choice. In communities where resistance to these drugs exceeds 20%, the fluoroquinolones (eg, ciprofloxacin, norfloxacin) are good alternatives. When adherence is a concern, fosfomycin, which requires just one dose, is an attractive choice. As a rule, beta-lactam antibiotics (eg, amoxicillin; cephalexin and other cephalosporins) should be avoided. Why? Because they are less effective than the alternatives, and less well tolerated.
Drug therapy of urinary tract infections
Specific urinary tract infections and their treatment

Drug
Dose
Duration
ACUTE CYSTITIS
First-Line Drugs
Trimethoprim/sulfamethoxazole
160/800 mg 2 times/day
3 days
Trimethoprim
100 mg 2 times/day
3 days
Nitrofurantoin
100 mg 2 times/day
7 days
Ciprofloxacin
250 mg 2 times/day
3 days
Norfloxacin
400 mg 2 times/day
3 days
Levofloxacin
250 mg once daily
3 days
Second-Line Drugs
Nitrofurantoin (macrocrystals)
50–100 mg 4 times/day
7 days
Nitrofurantoin (monohydrate/ macrocrystals)
100 mg 2 times/day
7 days
Fosfomycin
3 gm once
1 day
ACUTE UNCOMPLICATED PYELONEPHRITIS
First-Line Drugs
Trimethoprim/sulfamethoxazole
160/800 mg 2 times/day
14 days
Trimethoprim
100 mg 2 times/day
14 days
Ciprofloxacin
250–500 mg 2 times/day
14 days
Levofloxacin
250 mg once daily*
10 days
Second-Line Drugs
Amoxicillin (with clavulanic acid)
500 mg 3 times/day
14 days
Cephalexin
500 mg 4 times/day
14 days
Cefotaxime
1 gm 3 times/day
14 days
Ceftriaxone
1–2 gm once daily
14 days
COMPLICATED URINARY TRACT INFECTIONS
Trimethoprim/sulfamethoxazole
160/800 mg 2 times/day
7–14 days
Norfloxacin
400 mg 2 times/day
7–14 days
Ciprofloxacin
250–500 mg 2 times/day
7–14 days
Levofloxacin
500 mg once daily
7–14 days
Amoxicillin (with clavulanic acid)
500 mg 3 times/day
7–14 days
Cephalexin
500 mg 3 times/day
7–14 days
PROPHYLAXIS OF RECURRENT INFECTIONS
Trimethoprim/sulfamethoxazole
40/200 mg† at bedtime 3 times/wk
6 months
Trimethoprim
100 mg at bedtime
6 months
Nitrofurantoin
50–100 mg at bedtime
6 months
Norfloxacin
200 mg at bedtime
6 months
Acute cystitis
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Drug therapy of urinary tract infections
Only gold members can continue reading. Log In or Register to continue
