Describe the etiology, pathophysiology, and clinical manifestations of substance abuse.
 Identify the central nervous system (CNS) depressants of abuse.
Identify the central nervous system (CNS) depressants of abuse.
 Identify the prototypes and describe the action, use, adverse effects, contraindications, and nursing implications for the treatment of alcohol withdrawal and for the maintenance of sobriety.
Identify the prototypes and describe the action, use, adverse effects, contraindications, and nursing implications for the treatment of alcohol withdrawal and for the maintenance of sobriety.
 Identify commonly abused CNS stimulants.
Identify commonly abused CNS stimulants.
 Identify commonly abused psychoactive medications.
Identify commonly abused psychoactive medications.
 Implement the nursing process for patients who may be abusing CNS depressants, CNS stimulants, or other psychoactive substances.
Implement the nursing process for patients who may be abusing CNS depressants, CNS stimulants, or other psychoactive substances.
Clinical Application Case Study
Bryan Wilson is a 24-year-old man who regularly uses marijuana, alcohol, and tobacco. He was involved in a physical altercation at a local nightclub, and the owner called the police. The police brought Mr. Wilson to the emergency department, where he received a diagnosis of acute alcohol intoxication. He is admitted for treatment of alcohol withdrawal.
KEY TERMS
Intoxication: development of a reversible substance-specific syndrome caused by the recent ingestion of or exposure to a substance
Physical dependence: cluster of cognitive, behavioral, and physiological symptoms, indicating a person continues to use a substance of abuse despite significant substance-related problems
Psychological dependence: overwhelming desire to repeat the use of a particular drug to produce pleasure or avoid discomfort
Substance abuse: maladaptive pattern of substance use manifested by recurrent and significant adverse consequences related to repeated use of the substance
Tolerance: need for increasingly larger or more frequent doses of a substance to obtain the desired effects originally produced by a lower dose
Withdrawal: development of a substance-specific maladaptive behavioral change, with physiological and cognitive concomitants due to the cessation of or reduction in heavy and prolonged substance use
Introduction
This chapter introduces the pharmacological care of the patient who is experiencing substance abuse and substance dependence. It describes commonly abused substances, characteristics of substance-related disorders, and drugs used to treat substance-related disorders. Substance abuse is a maladaptive pattern of substance use, leading to clinically significant impairment or distress. This abuse involves self-administration of a drug for prolonged periods or in excessive amounts. It produces physical or psychological dependence, impairs functions of body organs, reduces the ability to function in usual activities of daily living, and decreases the ability and motivation to function as a productive member of society.
Substance abuse is a significant health, social, economic, and legal problem. It is often associated with substantial damage to the abuser and society (e.g., crime, child and spouse abuse, traumatic injury, chronic health problems, death).
Overview of Substance Abuse I and Dependence
Most drugs of abuse are those that affect the central nervous system (CNS) and alter the state of consciousness. Commonly abused drugs include CNS depressants (e.g., alcohol, antianxiety and sedative-hypnotic agents, opioid analgesics), CNS stimulants (e.g., cocaine, methamphetamine, methylphenidate, nicotine), and other mind-altering drugs (e.g., marijuana, ‘ecstasy”). The overwhelming desire to repeat the use of a particular drug to produce pleasure or avoid discomfort is known as substance dependence. Many of these commonly abused drugs have clinical usefulness and are discussed elsewhere: anxiolytics and sedative-hypnotics (see Chap. 53), opioids (see Chap. 48), and CNS stimulants (see Chap. 56). Although they produce different effects, they are associated with feelings of pleasure, positive reinforcement, and compulsive self-administration.
Psychological dependence involves feelings of satisfaction and pleasure from taking a drug. These feelings, perceived as extremely desirable by the drug-dependent person, contribute to acute intoxication (symptoms caused by recent ingestion of a substance), development and maintenance of drug-abuse patterns, and return to drug-taking behavior after periods of abstinence.
Physical dependence involves physiologic adaptation to chronic use of a drug so that withdrawal, or unpleasant symptoms, occur when the drug is stopped, when its action is antagonized by another drug, or when its dosage is decreased. Withdrawal or abstinence produces specific manifestations according to the type of drug and does not occur as long as adequate dosage is maintained. Attempts to avoid withdrawal symptoms reinforce psychological dependence and promote continuing drug use.
Characteristics of drug dependence include craving a drug, often with unsuccessful attempts to decrease its use; compulsive drug-seeking behavior; physical dependence; and continuing to take a drug despite adverse consequences (e.g., drug-related illnesses, mental or legal problems, job loss or decreased ability to function in an occupation, impaired family relationships). Box 57.1 describes other characteristics of substance abuse.
BOX 57.1 Characteristics of Substance Abuse and Dependence
Characteristics of Substance Abuse and Dependence
 Substance abuse involves all socioeconomic levels and affects all age groups. It is especially prevalent among adolescents and young adults. Patterns of abuse may vary by age group. For example, adolescents and young adults are more likely to use illicit drugs and older adults are more likely to abuse alcohol and prescription drugs. Health care professionals (e.g., physicians, pharmacists, nurses) are also considered at high risk for development of substance abuse disorders, at least partly because of easy access.
Substance abuse involves all socioeconomic levels and affects all age groups. It is especially prevalent among adolescents and young adults. Patterns of abuse may vary by age group. For example, adolescents and young adults are more likely to use illicit drugs and older adults are more likely to abuse alcohol and prescription drugs. Health care professionals (e.g., physicians, pharmacists, nurses) are also considered at high risk for development of substance abuse disorders, at least partly because of easy access.
 A person who abuses one drug is likely to abuse others.
A person who abuses one drug is likely to abuse others.
 Multiple drugs are often abused concurrently. Alcohol, for example, is often used with other drugs of abuse, probably because it is legal and readily available. In addition, alcohol, marijuana, opioids, and sedatives are often used to combat the anxiety and nervousness induced by cocaine, methamphetamine, and other CNS stimulants.
Multiple drugs are often abused concurrently. Alcohol, for example, is often used with other drugs of abuse, probably because it is legal and readily available. In addition, alcohol, marijuana, opioids, and sedatives are often used to combat the anxiety and nervousness induced by cocaine, methamphetamine, and other CNS stimulants.
 Abusers of alcohol and other drugs are not reliable sources of information about the types or amounts of drugs used. Most abusers understate the amount and frequency of substance use; heroin addicts may overstate the amount used in attempts to obtain higher doses of methadone. In addition, those who use illegal street drugs may not know what they have taken because of varying purity, potency, additives, contaminants, names, and substitutions of one drug for another.
Abusers of alcohol and other drugs are not reliable sources of information about the types or amounts of drugs used. Most abusers understate the amount and frequency of substance use; heroin addicts may overstate the amount used in attempts to obtain higher doses of methadone. In addition, those who use illegal street drugs may not know what they have taken because of varying purity, potency, additives, contaminants, names, and substitutions of one drug for another.
 Substance abusers rarely seek health care unless circumstances force the issue. Thus, most substance abuse comes to the attention of health care professionals when the abuser experiences a complication such as acute intoxication, withdrawal, or serious medical problems resulting from chronic drug overuse, misuse, or abuse.
Substance abusers rarely seek health care unless circumstances force the issue. Thus, most substance abuse comes to the attention of health care professionals when the abuser experiences a complication such as acute intoxication, withdrawal, or serious medical problems resulting from chronic drug overuse, misuse, or abuse.
 Smoking or inhaling drug vapors is a preferred route of administration for cocaine, marijuana, and nicotine because the drugs are rapidly absorbed from the large surface area of the lungs. Then, they rapidly circulate to the heart and brain without dilution by the systemic circulation or metabolism by enzymes.
Smoking or inhaling drug vapors is a preferred route of administration for cocaine, marijuana, and nicotine because the drugs are rapidly absorbed from the large surface area of the lungs. Then, they rapidly circulate to the heart and brain without dilution by the systemic circulation or metabolism by enzymes.
 Substance abusers who inject drugs intravenously are prey to serious problems because they use impure drugs of unknown potency, contaminated needles, poor hygiene, and other dangerous practices. Specific problems include overdoses, death, and numerous infections (e.g., hepatitis, human immunodeficiency virus [HIV] infection, endocarditis, phlebitis, cellulitis at injection sites).
Substance abusers who inject drugs intravenously are prey to serious problems because they use impure drugs of unknown potency, contaminated needles, poor hygiene, and other dangerous practices. Specific problems include overdoses, death, and numerous infections (e.g., hepatitis, human immunodeficiency virus [HIV] infection, endocarditis, phlebitis, cellulitis at injection sites).
Tolerance, which may be associated with many drugs if used repeatedly, is often an element of drug dependence. Increasing doses are required to obtain psychological effects or avoid physical withdrawal symptoms. The body “adjusts” to the drugs, and higher doses are needed to achieve feelings of pleasure (“reward”) or to stave off withdrawal symptoms (“punishment”). Both reward and punishment serve to reinforce continued substance abuse.
Etiology
Researchers have identified a number of factors in the predisposition to substance abuse and dependence. Biological factors include genetics. This is evident with many substances, especially with alcohol. Studies indicate that children of alcoholics are three times more likely than other children to become alcoholics themselves, even if reared away from the abusing parent. In addition, certain personality traits are thought to contribute to addictive behavior. Personality characteristics, such as low self-esteem, depression, and the inability to delay gratification, have been found in people with substance abuse and dependence.
Other factors important in developing drug dependence include the specific drug; the amount, frequency, and route of administration; and environmental or circumstantial characteristics. The environment in which a person uses a substance may contribute to the reinforcement. Moreover, the pleasurable effect of the substance itself may encourage the user to repeat it.
Cultural and ethnic influences may also play a role in substance abuse and dependence, related to patterns of consumption of substance and cultural acceptance of substance use. Lastly, peer pressure is often an important factor in initial and continuing drug ingestion. Although patterns of drug abuse vary in particular populations and in geographic areas, continuing trends seem to include increased use of methamphetamines, ‘club drugs,’ prescription drugs, and using multiple drugs at the same time. Internet web sites have become an important source of the drugs, and in some instances, instructions for manufacturing particular drugs are available.
Pathophysiology
Many drugs of abuse activate the pleasure or reward system in the brain by altering neurotransmission systems. Prolonged drug-abuse damages nerve cells in the brain and alters brain functions. The damage is long lasting.
Drug dependence is a complex phenomenon. Although the cause is unknown, one theory is that drugs stimulate or inhibit neurotransmitters in the brain to produce pleasure and euphoria or to decrease unpleasant feelings such as anxiety. For example, dopaminergic neurons in the limbic system are associated with the brain’s reward system and are thought to be sites of action of alcohol, amphetamines, cocaine, nicotine, and opiates. These major drugs of abuse increase dopaminergic transmission and the availability of dopamine. These actions are believed to stimulate the brain’s reward system and lead to compulsive drug administration and abuse.
The noradrenergic neurotransmission system, which uses norepinephrine as its neurotransmitter, is often involved as well as the dopaminergic system. Noradrenergic neurons innervate the limbic system and cerebral cortex and are important in setting mood and affect. Drugs that alter noradrenergic transmission have profound effects on mood and affect. Amphetamines and cocaine increase noradrenergic transmission, as with dopaminergic transmission, by promoting the release of norepinephrine and/or inhibiting its reuptake. Increased norepinephrine leads to mood elevation and euphoria, which promotes continued drug abuse. Increased norepinephrine also leads to major adverse effects of amphetamines and cocaine, including myocardial infarction, severe hypertension, and stroke, as well as profound mood swings from euphoria to depression.
Clinical Manifestations
Drug effects vary according to the type of substance being abused, the amount, route of administration, duration of use, and phase of substance abuse (e.g., acute intoxication, withdrawal syndromes, organ damage, medical illness). Thus, acute intoxication often produces profound behavioral changes, and chronic abuse often leads to serious organ damage and impaired ability to function in work, family, or social settings. Withdrawal symptoms are characteristic of particular types of drugs and are usually opposite to the effects originally produced. For example, withdrawal symptoms of alcohol and sedative-type drugs are mainly agitation, nervousness, and hyperactivity.
Therapy
General Approach
The major goals of treatment for substance abuse are detoxification, initiation of abstinence, and prevention of relapse. Patients who are likely to benefit from treatment are those who recognize that substance abuse is negatively influencing their problems and causing significant problems in their ability to function. Despite advances in treatment and the many adverse consequences of substance abuse, relapses to drug-taking behavior are common among people who have been detoxified or even abstinent for varying periods of time.
Treatments for substance abuse are limited but increasing, and more treatment facilities are needed. For most health professionals, contact with substance abusers is more likely to occur in acute situations, such as with intoxication or overdose, withdrawal syndromes, or various medical-surgical illnesses associated with the substance abuse. In general, treatment depends on the type, extent, and duration of drug-taking behavior and the particular situation for which treatment is needed.
Psychological rehabilitation efforts should be part of any treatment program for a drug-dependent person. Several approaches may be useful, including inpatient and outpatient psychotherapy, voluntary self-help groups (e.g., Alcoholics Anonymous, Narcotics Anonymous), and other types of emotional support and counseling. Box 57.2 gives sources of information about substance abuse.
BOX 57.2 Sources of Information About Substance Abuse
 The National Institute on Drug Abuse (NIDA) of the National Institutes of Health supports most of the world’s research on the health aspects of drug abuse and addiction.
The National Institute on Drug Abuse (NIDA) of the National Institutes of Health supports most of the world’s research on the health aspects of drug abuse and addiction.
6001 Executive Blvd.
Bethesda, MD 20892-9561
(301) 443-1124
 Substance Abuse and Mental Health Services Administration (SAMHSA)
Substance Abuse and Mental Health Services Administration (SAMHSA)
PO Box 2345
Rockville, MD 20847-2345
(877) 726-4727
 SAMHSA’s National Clearinghouse for Alcohol and Drug Information (NCADI): http://ncadi.samhsa.gov
SAMHSA’s National Clearinghouse for Alcohol and Drug Information (NCADI): http://ncadi.samhsa.gov
 The National Institute on Alcohol Abuse and Alcoholism (NIAAA) conducts and supports research on the causes, consequences, prevention, and treatment of alcohol abuse and disseminates research findings to general, professional, and academic audiences. Publications and research information are available at www.niaaa.nih.gov.
The National Institute on Alcohol Abuse and Alcoholism (NIAAA) conducts and supports research on the causes, consequences, prevention, and treatment of alcohol abuse and disseminates research findings to general, professional, and academic audiences. Publications and research information are available at www.niaaa.nih.gov.
Use of Drugs
Drug therapy for treatment of drug dependence is limited for several reasons. first, specific antidotes are available only for benzodiazepines (flumazenil) and opioid narcotics (naltrexone). Second, there is a high risk of substituting one abused drug for another. Third, there are significant drawbacks to giving CNS stimulants to reverse effects of CNS depressants and vice versa. Fourth, there is often inadequate information about the types and amounts of drug taken. Two of the more successful drug therapy regimens are methadone administration for heroin dependence and nicotine replacement (or other drugs [e.g., bupropion or varenicline]) for nicotine dependence. With both treatments, however, a combination of drug therapy and counseling is more effective than either method alone.
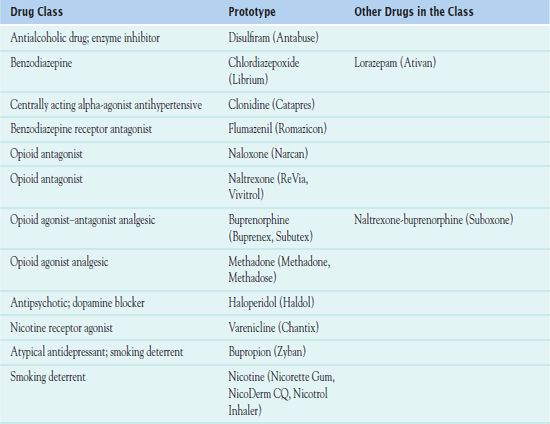
Treatment programs for substance abuse and dependence emphasize sobriety, which is complete abstinence from substance use. Combined with psychotherapy, there are pharmacological interventions that can assist the patient with sobriety. Table 57.1 lists the specific drugs that may be used treat substance-related disorders.
NCLEX Success
1. The nurse who is caring for a patient who has been abusing alcohol may expect to see what symptom as the patient enters withdrawal?
A. sleep
B. muscle relaxation
C. euphoria
D. agitation
2. The nurse is taking care of an adolescent male with a history of compulsive drug use. His parents have questioned him about the reasons behind such drug use. What factor is attributed to compulsive drug use?
A. drug stimulation of the “reward” center in the brain
B. a belief that the drugs are not harmful
C. parental pressure to do well in school
D. a permissive attitude toward taking drugs by parents and society
Central Nervous System Depressant I Abuse and Dependence: Drug Therapy
CNS depressants are drugs that slow down or “depress” brain activity. These drugs are capable of inducing varying degrees of CNS depression ranging from tranquilizing relief of anxiety to anesthesia, coma, and even death. Effects produced by these substances depend on the size of dose and potency of the drug administered. They include alcohol, benzodiazepines (antianxiety drugs), and opioids. Box 57.3 summarizes information about these drugs.
BOX 57.3 Central Nervous System Depressants of Abuse
Alcohol (Ethanol)
Alcohol is commonly abused around the world. It is legal and readily available, and its use is accepted in most societies. Excessive amounts and long-term abuse damages essentially all organ systems of the body. Alcohol is thought to exert its effects on the central nervous system (CNS) mainly by enhancing the activity of gamma-aminobutyric acid, an inhibitory neurotransmitter, or by inhibiting the activity of glutamate, an excitatory neurotransmitter.
The clinical manifestations of acute alcohol intoxication include impaired thinking, judgment, and psychomotor coordination, which may lead to poor work performance and accidents. There is a loss of conscious control of behavior, and exhibitionism and aggressiveness often result. Chronic ingestion may cause severe organ damage and mental problems.
Psychological dependence, physical dependence, tolerance, and cross-tolerance with other CNS depressants may occur with chronic alcohol consumption. People who are alcohol dependent are unlikely to seek treatment for alcohol abuse unless an acute illness or other situation forces the issue. However, they are likely to seek treatment for other disorders, such as agitation and anxiety. Delirium tremens, the most serious form of alcohol withdrawal, is characterized by confusion, disorientation, delusions, visual hallucinations, and other signs of acute psychosis. Treatment with psychological counseling, referral to a self-help group such as Alcoholics Anonymous, and drug therapy with disulfiram or naltrexone may be useful.
Benzodiazepines
Benzodiazepines, commonly used for their anxiolytic and sedative-hypnotic effects (see Chap. 53), are also widely abused, mainly by people who also abuse alcohol and/or other drugs. Benzodiazepines rarely cause respiratory depression or death, even in overdose, unless taken with alcohol or other drugs. However, they may cause over sedation, memory impairment, poor motor coordination, and confusion. Withdrawal reactions can be extremely uncomfortable. Unfortunately, abusers often combine drugs in their quest for a greater “high” or to relieve the unpleasant effects of CNS stimulants and other street drugs.
With mild benzodiazepine overdose, the patient usually sleeps off the effects of the drug. More severe overdoses cause respiratory depression and coma.
Flumazenil (Romazicon) is a specific antidote that can reverse benzodiazepine-induced sedation, coma, and respiratory depression. The drug competes with benzodiazepines for benzodiazepine receptors. It has a short duration of action, and repeated intravenous injections are usually necessary. Close observation is required, because symptoms of overdose may recur when the effects of a dose of flumazenil subside and because the drug may precipitate acute withdrawal symptoms (e.g., agitation, confusion, seizures).
Opioids
Opioids are potent analgesics extensively used in pain management (see Chap. 48). They are also commonly abused. Legal opioid analgesics are increasingly being diverted from their appropriate use and bought and sold as street drugs. The focus here is on heroin, a common drug of abuse. A Schedule I drug in the United States, it is not used therapeutically. Heroin produces the same effects as naturally occurring endorphins and other opioid drugs. The drug rapidly enters the brain, where it is converted to morphine. Morphine stimulates opioid receptors in the reward system of the brain, which causes greater amounts of dopamine to be released.
Opioids produce tolerance and high degrees of psychological and physical dependence. Most other drugs that produce dependence do so with prolonged usage of large doses, but morphine-like drugs produce dependence with repeated administration of small doses. Medical usage of these drugs produces physical dependence and tolerance but rarely leads to use or abuse for mind-altering effects. Thus, “addiction” should not be an issue when the drugs are needed for pain management in patients with cancer or other severe illnesses.
Treatment may be needed for overdose or withdrawal syndromes. Overdose may produce severe respiratory depression and coma. Insertion of an endotracheal tube and mechanical ventilation may be necessary. Drug therapy consists of an opioid antagonist, such as naloxone, to reverse opioid effects. In addition to profound respiratory depression, pulmonary edema, hypoglycemia, pneumonia, cellulitis, and other infections often accompany opioid overdose and require specific treatment measures.



