Identify patients at risk for developing nausea and vomiting.
 Discuss the phenothiazines in terms of indications and contraindications for use, routes of administration, and major adverse effects.
Discuss the phenothiazines in terms of indications and contraindications for use, routes of administration, and major adverse effects.
 Describe selected antihistamines used to control nausea and vomiting in terms of indications and contraindications for use, routes of administration, and major adverse effects.
Describe selected antihistamines used to control nausea and vomiting in terms of indications and contraindications for use, routes of administration, and major adverse effects.
 Discuss the 5-hydroxytryptamine3 receptor antagonists in terms of indications and contraindications for use, routes of administration, and major adverse effects.
Discuss the 5-hydroxytryptamine3 receptor antagonists in terms of indications and contraindications for use, routes of administration, and major adverse effects.
 Describe the substance P/neurokinin 1 antagonist aprepitant in terms of indications and contraindications for use, routes of administration, and major adverse effects.
Describe the substance P/neurokinin 1 antagonist aprepitant in terms of indications and contraindications for use, routes of administration, and major adverse effects.
 Identify the prototype drug for each drug class.
Identify the prototype drug for each drug class.
 Identify nonpharmacologic measures to reduce nausea and vomiting.
Identify nonpharmacologic measures to reduce nausea and vomiting.
 Understand how to use the nursing process in the care of patients receiving drugs for the management of nausea and vomiting.
Understand how to use the nursing process in the care of patients receiving drugs for the management of nausea and vomiting.
Clinical Application Case Study
Nellie Snyder is a 38-year-old woman with breast cancer who is receiving radiation and chemotherapy. She is experiencing significant nausea and vomiting.
KEY TERMS
Anticipatory nausea: conditioned response to chemotherapy or nausea in pregnancy that is triggered by fears of nausea and vomiting
Antiemetic: drug that is used to prevent or treat nausea and vomiting
Cannabinoid: derivative of marijuana
Chemoreceptor trigger zone: one of the central sites that relay stimuli to the vomiting center
Emesis: stomach contents produced with vomiting
Emetogenic: having the ability to cause vomiting
Motion sickness: action in which rapid changes in body motion stimulate receptors in the inner ear (vestibular branch of the auditory nerve, which is concerned with equilibrium), and nerve impulses are transmitted to the vomiting center.
Nausea: an unpleasant sensation of abdominal discomfort accompanied by a desire to vomit
Rescue antiemetic: antiemetic use after a prophylactic antiemetic drug regimen was unsuccessful in preventing emesis
Vomiting: expulsion of stomach contents through the mouth
Vomiting center: nucleus of cells in the medulla oblongata
Introduction
Nausea and vomiting are common symptoms experienced by virtually everyone at some time. Nausea, an unpleasant sensation of abdominal discomfort accompanied by a desire to vomit, may occur without vomiting, and vomiting, the expulsion of stomach contents through the mouth and occasionally nose, may occur without prior nausea, but the two symptoms often occur together. Antiemetic drugs are used to prevent or treat nausea and vomiting. They are usually contraindicated if their use may prevent or delay diagnosis or may mask signs and symptoms of drug toxicity.
Overview of Nausea and Vomiting
Etiology
Symptoms of nausea and vomiting may accompany almost any illness or stress situation. Causes of nausea and vomiting include the following:
• Gastrointestinal (GI) disorders, including infection or inflammation in the GI tract, liver, gallbladder, or pancreas; impaired GI motility and muscle tone (e.g., gastroparesis); and overeating or ingestion of foods or fluids that irritate the GI mucosa
• Cardiovascular, infectious, neurologic, or metabolic disorders
• Adverse effects of drug therapy; nausea and vomiting are the most common. Although the symptoms may occur with most drugs, they are especially associated with alcohol, aspirin, digoxin, anticancer drugs, antimicrobials, estrogen preparations, and opioid analgesics.
• Pain and other noxious stimuli, such as unpleasant sights and odors
• Emotional disturbances; physical or mental stress
• Radiation therapy
• Motion sickness
• Postoperative status, which may include pain, impaired GI motility, and receiving various medications
• Pregnancy
• Migraines
Pathophysiology
Vomiting occurs when the vomiting center (a nucleus of cells in the medulla oblongata) is stimulated (Fig. 36.1). Stimuli are relayed to the vomiting center by afferent signals from the chemoreceptor trigger zone (CTZ), as well as the cerebral cortex, the sensory organs, and the vestibular apparatus. The CTZ, composed of neurons in the fourth ventricle, can be activated by a variety of stimuli, including the presence of emetic substances (e.g., chemo-therapy, opioids, ipecac) in the blood and cerebrospinal fluid and stimuli from the pharynx and GI tract. In cancer chemotherapy, emetogenic drugs are thought to stimulate the release of serotonin from the enterochromaffin cells of the small intestine; this released serotonin then activates 5-HT3 receptors located on vagal afferent nerves in the CTZ to initiate the vomiting reflex. Activation of the CTZ is also thought to play a role in the nausea and vomiting associated with pregnancy. Anticipatory nausea triggered by memories and fear of nausea and vomiting is mediated by afferent signals from the higher centers of the cerebral cortex to the vomiting center. Noxious stimuli such as unpleasant odors or sights as well as pain are transmitted by afferent pathways from the sensory organs to the vomiting center. In motion sickness, rapid changes in body motion stimulate receptors in the inner ear (vestibular branch of the auditory nerve, which is concerned with equilibrium), and nerve impulses are transmitted to the vomiting center.
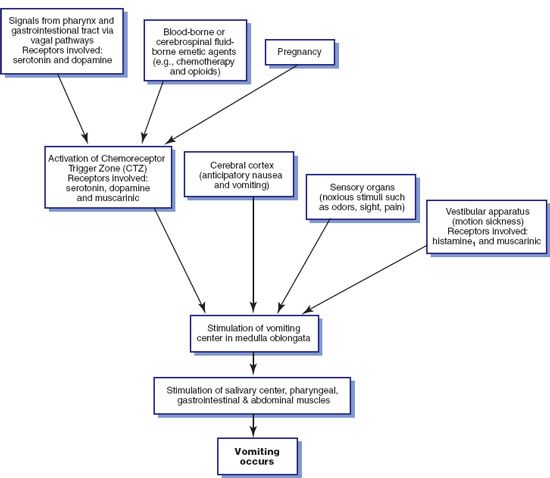
Figure 36.1 Pathophysiology of nausea and vomiting.
The vomiting center, CTZ, and GI tract contain benzodiazepine, cholinergic, dopamine, histamine, opiate, substance P/neurokinin, and serotonin receptors, which are stimulated by emetogenic drugs and toxins. When stimulated, the vomiting center initiates efferent impulses that stimulate the salivary center; cause closure of the glottis, contraction of abdominal muscles and the diaphragm, and relaxation of the gastroesophageal sphincter; and reverse peristalsis, which moves stomach contents toward the mouth for ejection.
Clinical Manifestations
As previously stated, nausea is an unpleasant abdominal sensation that is often, but not always, accompanied by vomiting. Emesis is the stomach contents produced with vomiting.
Drug Therapy
Antiemetic drugs are indicated to prevent and treat nausea and vomiting associated with surgery, pain, motion sickness, cancer chemotherapy, radiation therapy, pregnancy, and other causes. Drugs used to prevent or treat nausea and vomiting belong to several different therapeutic classifications and most have anticholinergic, antidopaminergic, antihistaminic, or antiserotonergic effects. In general, the drugs are more effective in prophylaxis than treatment. Most antiemetic agents are available in oral, parenteral, and rectal dosage forms. As a general rule, oral forms are preferred for prophylactic use, and rectal or parenteral forms are preferred for therapeutic use. When the nausea and vomiting associated with pregnancy are not controlled with lifestyle measures, some pharmacologic interventions may be appropriate. Most antiemetics prevent or relieve nausea and vomiting by acting on the vomiting center, CTZ, cerebral cortex, vestibular apparatus, or a combination of these. Table 36.1 describes major antiemetic drugs.
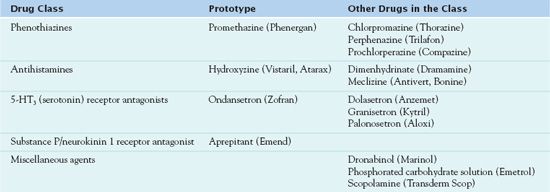
Phenothiazines
Phenothiazines are central nervous system (CNS) depressants that are used for a variety of reasons, including the prevention and treatment of nausea and vomiting. Dosage and route of administration depend primarily on the reason for use. Doses of phenothiazines are much smaller for antiemetic effects than for antipsychotic effects; not all phenothiazines are effective antiemetics. In this discussion,  promethazine (Phenergan), with its antiemetic action, serves as the prototype.
promethazine (Phenergan), with its antiemetic action, serves as the prototype.
Pharmacokinetics
Promethazine is rapidly absorbed following oral administration and undergoes extensive first-pass metabolism in the liver. Clinical effects are apparent within 20 minutes after oral, intramuscular, or rectal administration; the effects last 4 to 6 hours. Metabolism occurs in the liver, with excretion in the urine.
Action
Promethazine and other phenothiazines have widespread effects on the body. The therapeutic effects in nausea and vomiting are attributed to their ability to block dopamine from receptor sites in the brain and CTZ.
Use
Promethazine is used for the prevention and treatment of nausea and vomiting associated with surgery, anesthesia, migraines, chemotherapy, and motion sickness. Table 36.2 presents specific information about the use of promethazine and other phenothiazines, including dosages for adults and children.
 TABLE 36.2
TABLE 36.2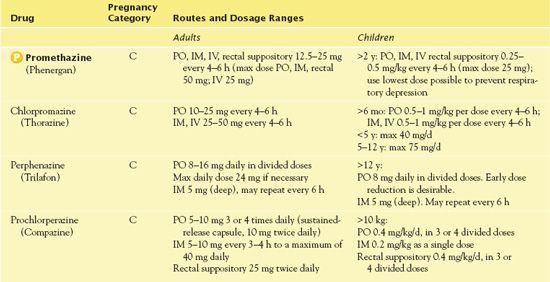
Clinical management guidelines for obstetrician-gynecologists: Nausea and vomiting of pregnancy
by AMERICAN COLLEGE OF OBSTETRICIANS AND GYNECOLOGISTS.
2004, ACOG Practice Bulletin. Obstetrics and Gynecology, 103, 803-811
Although the cause of morning sickness remains largely unknown, effective treatments to prevent and manage the condition are available. Severe morning sickness (hyperemesis gravidarum) is the most common cause of hospitalization during early pregnancy and is the second most common reason for hospitalization during pregnancy (second only to preterm labor). Practice guidelines from the American College of Obstetricians and Gynecologists include the following evidence-based pharmacologic recommendations for treating nausea and vomiting during pregnancy:
• Taking a multivitamin at the time of conception may be effective in decreasing the severity of morning sickness.
• Taking pyridoxine (vitamin B6) 30 to 75 mg daily in three divided doses with or without the antihistamine doxylamine 12.5 mg every 8 hours as needed is considered a first-line treatment option that is safe and effective.
IMPLICATIONS FOR NURSING PRACTICE: Nurses should be aware that pregnant women should not take any medication without the guidance of their health care provider. Some antiemetics are dangerous during pregnancy and can cause damage to the fetus. Lifestyle and dietary changes should be considered for treatment of mild cases. Prompt treatment of vomiting is more effective than managing long-term vomiting. See Chapter 6 for additional information on antiemetics used during pregnancy.
Use in Children
A BLACK BOX WARNING ♦ alerts nurses that promethazine is contraindicated in children younger than 2 years of age because of the risk of potentially fatal respiratory depression. Additionally, promethazine should not be used in children with hepatic disease, Reye’s syndrome, a history of sleep apnea, or a family history of sudden infant death syndrome.
Use in Older Adults
Older adults may have increased concerns with the adverse anticholinergic effects (e.g., dizziness, acute confusion, delirium, dry mouth, tachycardia, blurred vision, urinary retention, constipation).
Use in Patients With Renal Impairment
A dose reduction may be necessary in patients with renal impairment to avoid the possibility of adverse effects, toxicity, or increased sensitivity to phenothiazines.
Use in Patients With Hepatic Impairment
Phenothiazines are metabolized in the liver. Therefore, the presence of liver disease (e.g., cirrhosis, hepatitis) may slow metabolism and prolong drug elimination half-life, with resultant accumulation and increased risk of adverse effects. Thus, the drugs should be used cautiously in patients with hepatic impairment. Cholestatic jaundice may occur with promethazine.
Adverse Effects
With promethazine, common side effects include blurred vision, urinary retention, dry mouth, photosensitivity, drowsiness, and confusion.
Contraindications
Contraindications to use of promethazine include known hypersensitivity to the drug. Cautious use is necessary in people with glaucoma because the drug possesses antimuscarinic activity.
Nursing Implications
Preventing Interactions
Several medications interact with promethazine, increasing its effects (Box 36.1). Herbal interactions with promethazine have been reported with kava kava, St. John’s wort, and valerian; an increased risk of CNS depression is a possibility. No herbs or foods that decrease the effects of promethazine have been identified.
BOX 36.1  Drug Interactions: Promethazine
Drug Interactions: Promethazine
Drugs That Increase the Effects of Promethazine
 Escitalopram
Escitalopram
Has additive respiratory depressant effects
 Ethanol
Ethanol
Increases the risk of central nervous system depression and psychomotor impairment
 Duloxetine
Duloxetine
Increases the plasma concentration
 Gabapentin
Gabapentin
Has additive respiratory depressant effects
 Zolpidem
Zolpidem
Has additive respiratory depressant effects
Administering the Medication
A BLACK BOX WARNING ♦ alerts nurses that promethazine is contraindicated for subcutaneous administration. The preferred route of administration is intramuscular, which reduces risk of surrounding muscle and tissue damage. However, the drug can cause pain at the injection site. The nurse avoid intravenous (IV) administration, if possible, because the drug can cause severe tissue injury.
Assessing for Therapeutic Effects
The nurse observes for prevention or resolution of nausea and vomiting.
Assessing for Adverse Effects
The nurse assesses for associated adverse anticholinergic effects (dry mouth, blurred vision, urinary retention, constipation, acute confusion, dizziness, tachycardia). It is necessary to be aware that hallucinations, convulsions, and sudden death may occur with excessive doses. The nurse also assesses tissue integrity with injection of the drug because the drug may cause severe tissue injury; burning and pain at the IV site justify immediate discontinuation of the drug.
Patient Teaching
The nurse teaches patients taking promethazine to use the lowest effective dosage and not to take other drugs with respiratory depressant effects concurrently. Box 36.2 presents additional patient teaching guidelines.
BOX 36.2  Drug Interactions: Promethazine
Drug Interactions: Promethazine
General Considerations
 Try to identify the circumstances that cause or aggravate nausea and vomiting and avoid them when possible.
Try to identify the circumstances that cause or aggravate nausea and vomiting and avoid them when possible.
 Drugs are more effective in preventing nausea and vomiting than in stopping them. Thus, they should be taken before the causative event when possible.
Drugs are more effective in preventing nausea and vomiting than in stopping them. Thus, they should be taken before the causative event when possible.
 Do not eat, drink, or take oral medications during acute vomiting episodes, to avoid aggravating the stomach upset.
Do not eat, drink, or take oral medications during acute vomiting episodes, to avoid aggravating the stomach upset.
 Lying down may help nausea and vomiting to subside; activity tends to increase stomach upset.
Lying down may help nausea and vomiting to subside; activity tends to increase stomach upset.
 After your stomach has settled down, try to take enough fluids to prevent dehydration and potentially serious problems. Tea, broth, and gelatins are usually tolerated.
After your stomach has settled down, try to take enough fluids to prevent dehydration and potentially serious problems. Tea, broth, and gelatins are usually tolerated.
 Do not drive an automobile or operate dangerous machinery if drowsy from antiemetic drugs, to avoid injury.
Do not drive an automobile or operate dangerous machinery if drowsy from antiemetic drugs, to avoid injury.
 If you take antiemetic drugs regularly, do not drink alcohol or take other drugs without consulting a health care provider. Several drugs interact with antiemetic agents, to increase adverse effects.
If you take antiemetic drugs regularly, do not drink alcohol or take other drugs without consulting a health care provider. Several drugs interact with antiemetic agents, to increase adverse effects.
 Dronabinol, which is derived from marijuana and recommended only for nausea and vomiting associated with cancer chemotherapy, can cause dizziness, drowsiness, mood changes, and other mind-altering effects. You should avoid alcohol and other drugs that cause drowsiness. Also, do not drive or perform hazardous tasks requiring alertness, coordination, or physical dexterity, to decrease risks of injury.
Dronabinol, which is derived from marijuana and recommended only for nausea and vomiting associated with cancer chemotherapy, can cause dizziness, drowsiness, mood changes, and other mind-altering effects. You should avoid alcohol and other drugs that cause drowsiness. Also, do not drive or perform hazardous tasks requiring alertness, coordination, or physical dexterity, to decrease risks of injury.
Self- or Caregiver Administration
 Take the drugs as prescribed. Do not increase dosage, take more often, or take when drowsy, dizzy, or unsteady on your feet. Several of the drugs cause sedation and other adverse effects, which are more severe if too much is taken.
Take the drugs as prescribed. Do not increase dosage, take more often, or take when drowsy, dizzy, or unsteady on your feet. Several of the drugs cause sedation and other adverse effects, which are more severe if too much is taken.
 To prevent motion sickness, take medication 30 minutes before travel and then every 4 to 6 hours, if necessary, to avoid or minimize adverse effects.
To prevent motion sickness, take medication 30 minutes before travel and then every 4 to 6 hours, if necessary, to avoid or minimize adverse effects.
 Take or give antiemetic drugs 30 to 60 minutes before a nausea-producing event, when possible. This includes cancer chemotherapy, radiation therapy, changing of painful dressings, or other treatments.
Take or give antiemetic drugs 30 to 60 minutes before a nausea-producing event, when possible. This includes cancer chemotherapy, radiation therapy, changing of painful dressings, or other treatments.
 Take dronabinol only when you can be supervised by a responsible adult because of its sedative and mind-altering effects.
Take dronabinol only when you can be supervised by a responsible adult because of its sedative and mind-altering effects.
 Aprepitant (Emend) reduces the effectiveness of oral contraceptives; therefore, use an alternative form of birth control during therapy and for 1 month after therapy.
Aprepitant (Emend) reduces the effectiveness of oral contraceptives; therefore, use an alternative form of birth control during therapy and for 1 month after therapy.
Other Drugs in the Class
Although phenothiazines are effective antiemetic agents, because of their adverse effects (e.g., sedation, cognitive impairment, extrapyramidal reactions), phenothiazines are mainly indicated if vomiting is severe and cannot be controlled by other measures or only when a few doses are needed. Prochlorperazine (Compazine), which has a side-effect profile similar to that of promethazine, is used in the treatment of severe nausea and vomiting associated with anesthesia. Chlorpromazine (Thorazine), which is more commonly used in the treatment of psychosis and psychotic symptoms in other disorders (see Chap. 55), is also used with intractable hiccups and treatment of nausea and vomiting associated with anesthesia. Perphenazine (Trilafon) is used to manage intractable hiccups and severe nausea and vomiting.
Antihistamines
Antihistamines are used primarily to prevent histamine from exerting its widespread effects on body tissues (see Chap. 30). Antihistamines used as antiemetic agents are the “classic” antihistamines or H1 receptor blocking agents (as differentiated from cimetidine and related drugs, which are H2 receptor blocking agents). Not all antihistamines are effective as antiemetic agents.  Hydroxyzine (Vistaril, Atarax) is the prototype of the class.
Hydroxyzine (Vistaril, Atarax) is the prototype of the class.
Pharmacokinetics
When administered orally, hydroxyzine is rapidly absorbed from the GI tract, with its effect noticeable within 30 minutes. The drug is metabolized in the liver, and the main metabolite is cetirizine. The half-life of hydroxyzine is, on average, 14 hours for adults, but it can be as short as 5 hours for small children and as long as 30 hours for elderly people. Hydroxyzine is excreted into the urine in the form of its metabolites.
Action
Hydroxyzine and other antihistamines are thought to relieve nausea and vomiting by blocking the action of acetylcholine in the brain.
Use
Hydroxyzine may be effective in treating nausea and vomiting and preventing and treating motion sickness. Hydroxyzine is also used as a sedative to treat anxiety. Additionally, the drug is given in combination with other medications during anesthesia. Table 36.3 presents dosage information for the antihistamines.
 TABLE 36.3
TABLE 36.3 Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


