Describe factors that regulate blood pressure.
 Describe how hypertension is classified.
Describe how hypertension is classified.
 Discuss nonpharmacologic measures to control hypertension.
Discuss nonpharmacologic measures to control hypertension.
 Identify the prototype and describe the action, use, contraindications, adverse effects, and nursing implications of the angiotensin-converting enzyme inhibitors.
Identify the prototype and describe the action, use, contraindications, adverse effects, and nursing implications of the angiotensin-converting enzyme inhibitors.
 Identify the prototype and describe the action, use, contraindications, adverse effects, and nursing implications of the angiotensin II receptor blockers.
Identify the prototype and describe the action, use, contraindications, adverse effects, and nursing implications of the angiotensin II receptor blockers.
 Describe the rationale for using combination drugs in the management of hypertension.
Describe the rationale for using combination drugs in the management of hypertension.
 Review the effects of alpha-adrenergic blockers, beta-adrenergic blockers, calcium channel blockers, and diuretics in the management of hypertension.
Review the effects of alpha-adrenergic blockers, beta-adrenergic blockers, calcium channel blockers, and diuretics in the management of hypertension.
 Apply the nursing process in the care of patients with hypertension.
Apply the nursing process in the care of patients with hypertension.
Clinical Application Case Study
Harold Caudill, a 55-year-old African American man, is married, has four children, and works as an automobile salesman. He has a history of primary hypertension. His medical history includes type 1 diabetes mellitus, with early signs of nephropathy. After having a myocardial infarction (MI) 2 years ago, he has been treated with metoprolol, a beta blocker. In addition, he has been taking hydrochlorothiazide to treat the hypertension. His blood pressure today is 138/92 mm Hg, which is consistent with the readings on his last three visits. His physician has added captopril to his treatment regimen.
KEY TERMS
Angioedema: sudden swelling of the lips, tongue, throat, hands, or feet
Angiotensin-converting enzyme (ACE) inhibitor: drug that decreases activation of the renin–angiotensin–aldosterone system; specifically, the drug prevents inactive angiotensin I from being converted to angiotensin II
Angiotensin II receptor blocker: similar to ACE inhibitor, although the mechanism of action is blockade of the angiotensin II receptor site
Antiadrenergics: decrease or block the effects of sympathetic nerve stimulation
Autoregulation: ability of body tissues to regulate their own blood flow
Bradykinin: peptide that causes vasodilation and lowers blood pressure
Essential hypertension: high blood pressure for which no cause can be found
First-dose phenomenon: orthostatic hypotension with palpitations, dizziness, and perhaps syncope 1 to 3 hours after the first dose of a drug or an increased dose
Introduction
Antihypertensive drugs are used to treat hypertension, a common, chronic disorder affecting an estimated 50 to 60 million adults and an unknown number of children and adolescents in the United States. Hypertension increases risks of MI, heart failure, cerebral infarction and hemorrhage, and renal disease. To understand hypertension and antihypertensive drug therapy, it is necessary first to understand the physiologic mechanisms that normally control blood pressure, the characteristics of hypertension, and the characteristics of antihypertensive drugs.
Overview of Hypertension
Regulation of Blood Pressure
Arterial blood pressure reflects the force exerted on arterial walls by blood flow. Blood pressure normally remains constant because of homeostatic mechanisms that adjust blood flow to meet tissue needs. The two major determinants of arterial blood pressure are cardiac output (systolic pressure) and peripheral vascular resistance (diastolic pressure).
Cardiac output equals the product of the heart rate and stroke volume (CO = HR × SV). Stroke volume is the amount of blood ejected with each heartbeat (approximately 60–90 mL). Thus, cardiac output depends on the force of myocardial contraction, blood volume, and other factors. Peripheral vascular resistance is determined by local blood flow and the degree of constriction or dilation in arterioles and arteries (vascular tone).
Autoregulation of Blood Flow
Autoregulation is the ability of body tissues to regulate their own blood flow. This is a critical mechanism of major organs (e.g., heart, brain, kidneys) to preserve oxygenation and function. Local blood flow is regulated primarily by nutritional needs of the tissue, such as lack of oxygen or accumulation of products of cellular metabolism (e.g., carbon dioxide, lactic acid). Local tissues produce vasodilating and vasoconstricting substances to regulate local blood flow. Important tissue factors include histamine, bradykinin, serotonin, and prostaglandins.
Histamine is found mainly in mast cells surrounding blood vessels and is released when these tissues are injured. In some tissues, such as skeletal muscle, mast cell activity is mediated by the sympathetic nervous system (SNS), and histamine is released when SNS stimulation is blocked or withdrawn. In this case, vasodilation results from increased histamine release and the withdrawal of SNS vasoconstrictor activity. Bradykinin is released from a protein in body fluids. Kinins dilate arterioles, increase capillary permeability, and constrict venules. Serotonin is released from aggregating platelets during the blood clotting process. It causes vasoconstriction and plays a major role in control of bleeding. Prostaglandins are formed in response to tissue injury and include vasodilators (e.g., prostacyclin) and vasoconstrictors (e.g., thromboxane A2).
An important component of regulating local blood flow is the production of several vasoactive substances by the endothelial cells that line blood vessels. Vasoconstricting substances, which increase vascular tone and blood pressure, include angiotensin II, endothelin-1, and thromboxane A2. Vasodilating substances, which decrease vascular tone and blood pressure, include nitric oxide and prostacyclin. Excessive vasoconstrictors or deficient vasodilators may contribute to the development of atherosclerosis, hypertension, and other diseases. Injury to the endothelial lining of blood vessels by the sheer force of blood flow with hypertension or by rupture of atherosclerotic plaque leads to vasoconstriction, vasospasm, thrombus formation, and thickening of the blood vessel wall. All of these factors narrow the blood vessel lumen and increase peripheral vascular resistance.
Overall, regulation of blood pressure involves a complex, interacting, overlapping network of hormonal, neural, and vascular mechanisms, and any condition that affects heart rate, stroke volume, or peripheral vascular resistance affects arterial blood pressure. Many of these mechanisms are compensatory effects that attempt to restore balance when hypotension or hypertension occurs. Box 28.1 further describes these mechanisms.
BOX 28.1 Mechanisms That Regulate Blood Pressure
Neural
Neural regulation of blood pressure mainly involves the sympathetic nervous system (SNS). In the heart, SNS neurons control heart rate and force of contraction. In blood vessels, SNS neurons control muscle tone by maintaining a state of partial contraction, with additional constriction or dilation accomplished by altering this basal state. When hypotension and inadequate tissue perfusion occur, the SNS is activated and produces secretion of epinephrine and norepinephrine by the adrenal medulla; constriction of blood vessels in the skin, gastrointestinal tract, and kidneys; and stimulation of beta-adrenergic receptors in the heart, which increases heart rate and force of myocardial contraction. All of these mechanisms act to increase blood pressure and tissue perfusion, especially of the brain and heart.
The SNS is activated by the vasomotor center in the brain, which constantly receives messages from baroreceptors and chemoreceptors located in the circulatory system. Adequate function of these receptors is essential for rapid and short-term regulation of blood pressure. The vasomotor center interprets the messages from these receptors and modifies cardiovascular functions to maintain adequate blood flow.
More specifically, baroreceptors detect changes in pressure or stretch. For example, when a person moves from a lying to a standing position, blood pressure falls and decreases stretch in the aorta and arteries. This elicits increased heart rate and vasoconstriction to restore adequate circulation. The increased heart rate occurs rapidly and blood pressure is adjusted within 1 to 2 minutes. This quick response prevents orthostatic hypotension with dizziness and possible syncope. (Antihypertensive medications may blunt this response and cause orthostatic hypotension.)
Chemoreceptors, which are located in the aorta and carotid arteries, are in close contact with arterial blood and respond to changes in the oxygen, carbon dioxide, and hydrogen ion content of blood. Although their main function is to regulate ventilation, they also communicate with the vasomotor center and can induce vasoconstriction.
Chemoreceptors are stimulated when blood pressure drops to a certain point because oxygen is decreased and carbon dioxide and hydrogen ions are increased in arterial blood.
The central nervous system (CNS) also regulates vasomotor tone and blood pressure. Inadequate blood flow to the brain results in ischemia of the vasomotor center. When this occurs, neurons in the vasomotor center stimulate widespread vasoconstriction in an attempt to raise blood pressure and restore blood flow. This reaction, the CNS ischemic response, is an emergency measure to preserve blood flow to vital brain centers. If blood flow is not restored within 3 to 10 minutes, the neurons of the vasomotor center are unable to function, the impulses that maintain vascular muscle tone stop, and blood pressure drops to a fatal level.
Hormonal
The renin-angiotensin-aldosterone (RAA) system and vasopressin are important hormonal mechanisms in blood pressure regulation.
The RAA system is activated in response to hypotension and acts as a compensatory mechanism to restore adequate blood flow to body tissues. Renin is an enzyme that is synthesized, stored, and released from the kidneys in response to decreased blood pressure, SNS stimulation, or decreased sodium concentration in extracellular fluid. When released into the bloodstream, where its action lasts 30 to 60 minutes, renin converts angiotensinogen (a plasma protein) to angiotensin I. Angiotensin-converting enzyme (ACE) in the endothelium of pulmonary blood vessels then acts on angiotensin I to produce angiotensin II. Angiotensin II strongly constricts arterioles (and weakly constricts veins), increases peripheral resistance, and increases blood pressure by direct vasoconstriction, stimulation of the SNS, and stimulation of catecholamine release from the adrenal medulla. It also stimulates secretion of aldosterone from the adrenal cortex, which then causes the kidneys to retain sodium and water. Retention of sodium and water increases blood volume, cardiac output, and blood pressure.
Vasopressin, also called antidiuretic hormone or ADH, is a hormone secreted by the posterior pituitary gland that regulates reabsorption of water by the kidneys. It is released in response to decreased blood volume and decreased blood pressure. It causes retention of body fluids and vasoconstriction, both of which act to raise blood pressure.
Vascular
The endothelial cells that line blood vessels synthesize and secrete several substances that play important roles in regulating cardiovascular functions, including blood pressure. These substances normally maintain a balance between vasoconstriction and vasodilation. When the endothelium is damaged (e.g., by trauma, hypertension, hypercholesterolemia, or atherosclerosis), the resulting imbalance promotes production of vasoconstricting substances and also causes blood vessels to lose their ability to relax in response to dilator substances. In addition, changes in structure of endothelial and vascular smooth muscle cells (vascular remodeling) further impair vascular functions.
Vasoconstrictors increase vascular tone (i.e., constrict or narrow blood vessels so that higher blood pressure is required to pump blood to body tissues). Vasoconstricting substances produced by the endothelium include angiotensin II, endothelin-1, platelet-derived growth factor (PDGF), and thromboxane A2. Endothelin-1 is the strongest endogenous vasoconstrictor known. Angiotensin II and thromboxane A2 can also be produced by other types of cells, but endothelial cells can produce both. Thromboxane A2, a product of arachidonic acid metabolism, also promotes platelet aggregation and thrombosis.
Vasodilators decrease vascular tone and blood pressure. Major vasodilating substances produced by the endothelium include nitric oxide and prostacyclin (prostaglandin I2).
Nitric oxide (NO) is a gas that can diffuse through cell membranes, trigger biochemical reactions, and then dissipate rapidly. It is formed by the action of the enzyme NO synthase on the amino acid L-arginine and continually released by normal endothelium. Its production is tightly regulated and depends on the amount of ionized calcium in the fluid portion of endothelial cells. Several substances (e.g., acetylcholine, bradykinin, catecholamines, substance P, and products of aggregating platelets such as adenosine diphosphate and serotonin) act on receptors in endothelial cell membranes to increase the cytosolic concentration of ionized calcium, activate NO synthase, and increase NO production. In addition, increased blood flow or blood pressure increases shear stress at the endothelial surface and stimulates production of NO.
Once produced, endothelium-derived NO produces vasodilation primarily by activating guanylyl cyclase in vascular smooth muscle cells and increasing intracellular cyclic 3’,5’-guanosine monophosphate as a second messenger. NO also inhibits platelet aggregation and production of platelet-derived vasoconstricting substances. Because NO is released into the vessel wall (to relax smooth muscle) and into the vessel lumen (to inactivate platelets), it is thought to have protective effects against vasoconstriction and thrombosis.
NO is also produced in leukocytes, fibroblasts, and vascular smooth muscle cells and may have pathologic effects when large amounts are produced. In these tissues, NO seems to have other functions, such as modifying nerve activity in the nervous system.
Prostacyclin is synthesized and released from endothelium in response to stimulation by several factors (e.g., bradykinin, interleukin-1, serotonin, thrombin, PDGF). It produces vasodilation by activating adenylyl cyclase and increasing levels of cyclic adenosine monophosphate in smooth muscle cells. In addition, like NO, prostacyclin also inhibits platelet aggregation and production of platelet-derived vasoconstricting substances. The vasodilating effects of prostacyclin may occur independently or in conjunction with NO.
Overall, excessive vasoconstrictors or deficient vasodilators may contribute to the development of atherosclerosis, hypertension, and other diseases. Injury to the endothelial lining of blood vessels (e.g., by the sheer force of blood flow with hypertension or by rupture of atherosclerotic plaque) decreases vasodilators and leads to vasoconstriction, vasospasm, thrombus formation, and thickening of the blood vessel wall. All of these factors require the blood to flow through a narrowed lumen and increase blood pressure.
Vascular Remodeling
Vascular remodeling is similar to the left ventricular remodeling that occurs in heart failure (see Chap. 24). It results from endothelial dysfunction and produces a thickening of the blood vessel wall and a narrowing of the blood vessel lumen. Thickening of the wall makes blood vessels less flexible and less able to respond to vasodilating substances. There are also changes in endothelial cell structure (i.e., the connections between endothelial cells become looser) that lead to increased permeability. The mechanisms of these vascular changes, which promote and aggravate hypertension, are described below.
As discussed in previous chapters, normal endothelium helps maintain a balance between vasoconstriction and vasodilation, procoagulation and anticoagulation, proinflammation and anti-inflammation, and progrowth and antigrowth. In the inflammatory process, normal endothelium acts as a physical barrier against the movement of leukocytes into the subendothelial space. Endothelial products such as nitric oxide may also inhibit leukocyte activity. However, inflammatory cytokines such as tumor necrosis factor-alpha and interleukin-1 activate endothelial cells to produce adhesion molecules (which allow leukocytes to adhere to the endothelium), interleukin-8 (which attracts leukocytes to the endothelium and allows them to accumulate in subendothelial cells), and foam cells (lipid-filled monocyte/macrophages that form fatty streaks, the beginning lesions of atherosclerotic plaque). Although activation of endothelial cells may be a helpful component of the normal immune response, the resulting inflammation may contribute to disease development.
In terms of cell growth, normal endothelium limits the growth of vascular smooth muscle that underlies the endothelium and forms the vessel wall. Growth-inhibiting products of the endothelium include nitric oxide, which also inhibits platelet activation and production of growth-promoting substances. When the endothelium is damaged, endothelial cells become activated and also produce growth-promoting products. Other endothelial products (e.g., angiotensin II and endothelin-1) may also stimulate growth of vascular smooth muscle cells. Thus, damage or loss of endothelial cells stimulates growth of smooth muscle cells in the intimal layer of the blood vessel wall.
Types of Hypertension
Hypertension is persistently high blood pressure that results from abnormalities in regulatory mechanisms. It is usually defined as a systolic pressure above 140 mm Hg or a diastolic pressure above 90 mm Hg on multiple blood pressure measurements. The Eighth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 8) is long awaited and expected to be released in 2012. The recommendations have been the cornerstone in the detection, evaluation, and treatment of high blood pressure. The Seventh Report, published in 2004, classifies blood pressures in adults (in mm Hg) into four categories (Box 28.2). These guidelines also recommend a goal blood pressure of less than 130/80 mm Hg for people with diabetes or renal disease.
BOX 28.2 Classification of Hypertension (all values in mm Hg)
 Normal = systolic <120 and diastolic <80
Normal = systolic <120 and diastolic <80
 Prehypertension = systolic 120-139 or diastolic 80-89
Prehypertension = systolic 120-139 or diastolic 80-89
 Stage 1 hypertension = systolic 140-159 or diastolic 90-99
Stage 1 hypertension = systolic 140-159 or diastolic 90-99
 Stage 2 hypertension = systolic > 160 or diastolic 100 or more
Stage 2 hypertension = systolic > 160 or diastolic 100 or more
From U.S. Department of Health and Human Services, National Institutes of Health, National Heart, Lung, and Blood Institute, National High Blood Pressure Education Program. The Seventh Report of the Joint National Committee on Prevention, Detection, Evolution, and Treatment of High Blood Pressure (JNC 7). NIH Publication No. 04–5230, August 2004.
A systolic pressure of 140 mm Hg or greater, with a diastolic pressure of less than 90 mm Hg, is called isolated systolic hypertension and is more common in the elderly. Systolic–diastolic hypertension, which may also occur in older adults, involves elevations of both systolic and diastolic pressures. Both types increase cardiovascular morbidity and mortality, especially heart failure and stroke, and warrant treatment.
A hypertensive emergency or crisis is a diastolic pressure of 120 mm Hg or higher and possible target organ damage. (A hypertensive urgency is an episode of marked elevation in blood pressure without target organ damage. The goal of management is to lower blood pressure within 24 hours.)
Etiology
Although it has frequently been indicated that the causes of primary hypertension, or essential hypertension, are not known, this is only partially true; genetic variations and inherited, behavioral, and environmental factors may increase blood pressure. These include obesity, high alcohol intake, insulin resistance, high salt intake in salt-sensitive people, aging, sedentary lifestyle, and stress. Furthermore, many of these factors are additive, such as obesity and alcohol intake. Primary hypertension makes up 90% to 95% of known cases. Appropriate therapy usually controls primary hypertension.
Secondary hypertension may result from renal, endocrine, or central nervous system disorders and from drugs that stimulate the SNS or cause retention of sodium and water, producing adverse effects. Secondary hypertension can sometimes be cured by managing the underlying condition or cause. Hypertensive emergencies often result from such conditions as cerebral hemorrhage, dissecting aortic aneurysm, renal disease, pheochromocytoma, or eclampsia.
Pathophysiology
Hypertension profoundly alters cardiovascular function by increasing the workload of the heart and causing thickening and sclerosis of arterial walls. The increased cardiac workload leads to myocardial hypertrophy as a compensatory mechanism, with eventual heart failure. As a result of endothelial dysfunction and arterial changes (vascular remodeling), the arterial lumen narrows, blood supply to tissues decreases, and the risk of thrombosis increases. In addition, necrotic areas may develop in arteries, and these may rupture with sustained high blood pressure. The areas of most serious damage are the heart, brain, kidneys, and eyes. These are often called target organs.
Response to Hypotension
When hypotension (and decreased tissue perfusion) occurs, the SNS is stimulated, the hormones epinephrine and norepinephrine are secreted by the adrenal medulla, angiotensin II and aldosterone are formed, and the kidneys retain fluid. These compensatory mechanisms raise the blood pressure. Specific effects include the following:
• Constriction of arterioles, which increases peripheral vascular resistance
• Constriction of veins and increased venous tone
• Stimulation of cardiac beta-adrenergic receptors, which increases heart rate and force of myocardial contraction
• Activation of the renin-angiotensin-aldosterone mechanism
Chapter 27 contains an additional discussion of the effects and management of hypotension.
Response to Hypertension
• When arterial blood pressure is elevated, the following sequence of events occurs:
• Kidneys excrete more fluid (increase urine output).
• Fluid loss reduces both extracellular fluid volume and blood volume.
• Decreased blood volume reduces venous blood flow to the heart and therefore decreases cardiac output.
• Decreased cardiac output reduces arterial blood pressure.
• The vascular endothelium produces vasodilating substances (e.g., nitric oxide, prostacyclin), which reduce blood pressure.
Clinical Manifestations
Initially, and perhaps for years, primary hypertension may produce no symptoms. If symptoms occur, they are usually vague and nonspecific. Hypertension may go undetected, or it may be incidentally discovered when blood pressure measurements are taken as part of a routine physical examination, screening test, or assessment of other disorders. Eventually, symptoms reflect target organ damage. Hypertension is often discovered after a person experiences angina pectoris, MI, heart failure, stroke, or renal disease.
Symptoms include severe headache, nausea, vomiting, visual disturbances, neurologic disturbances, disorientation, and decreased level of consciousness (drowsiness, stupor, coma). Hypertensive emergencies require immediate blood pressure reduction with parenteral antihypertensive drugs to limit damage to target organs.
Therapy
Goals of Treatment
After the diagnosis of hypertension is established, it is essential that a therapeutic regimen be designed and implemented. The goal of management for most patients is to achieve and maintain blood pressure well below 140/90 mm Hg. The target blood pressure for people with diabetes is 130/80 mm Hg. If the goal is impossible to achieve, lowering blood pressure to any extent is still considered beneficial in decreasing the incidence of coronary artery disease (CAD) and stroke. In most instances, it is better to lower blood pressure gradually and to avoid wide fluctuations in blood pressure.
Nonpharmacologic Treatment
The Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) recommends management guidelines in which initial interventions include lifestyle modifications (i.e., reduction of weight and sodium intake, regular physical activity, moderate alcohol intake, and no smoking) to maintain normal blood pressure. If these modifications do not produce the target blood pressure or substantial progress toward the target blood pressure, it is important to initiate antihypertensive drug therapy and continue lifestyle modifications.
Dietary Management
Key behavioral determinants of blood pressure are related to dietary consumption of calories and salt; the prevalence of hypertension rises proportionally to average body mass index. The Dietary Approaches to Stop Hypertension (DASH) study demonstrated that people with prehypertension or stage 1 hypertension can reduce their blood pressures by adhering to a diet abundant in fresh fruits and vegetables and low-fat dairy products even without restricting calorie or sodium intake. The effects of the DASH diet demonstrate blood pressure–lowering effects that parallel the degree of benefit from drug monotherapy and may include dietary sodium restriction. Effects are evident in all ethnic groups, particularly African Americans.
Severe restrictions of sodium intake usually are not acceptable to people; however, moderate restrictions (4–6 g of salt a day) are beneficial and more easily implemented. Avoiding heavily salted foods (e.g., cured meats, sandwich meats, pretzels, potato chips) and not adding salt to food at the table can achieve this. Research and clinical observations indicate the following:
• Sodium restriction alone reduces blood pressure.
• Sodium restriction potentiates the antihypertensive actions of diuretics and other antihypertensive drugs. Conversely, excessive sodium intake decreases the antihypertensive actions of all antihypertensive drugs. Patients with unrestricted salt intake who are taking thiazides may lose excessive potassium and become hypokalemic.
• Sodium restriction may decrease dosage requirements of antihypertensive drugs, thereby decreasing the incidence and severity of adverse effects.
Lifestyle Management
Considerable evidence demonstrates that regular aerobic exercise by itself effectively reduces blood pressure. However, the direct benefits of exercise on blood pressure control are often difficult to isolate from those of the changes that often accompany exercise, such as improved diet, weight loss, decreased alcohol consumption, and decreased cigarette smoking. The JNC 7 recommendations include increasing exercise to at least 30 minutes per day at least 4 days per week, achieving a weight loss goal of at least 10 pounds, limiting alcohol consumption to two drinks or less per day for men and one drink or less per day for women, and ceasing smoking.
Drug Treatment
Drugs used in the management of primary hypertension belong to several different groups, including angiotensin-converting enzyme (ACE) inhibitors; angiotensin II receptor blockers (ARBs), also called angiotensin II receptor antagonists; antiadrenergics; calcium channel blockers; diuretics; and direct vasodilators. In general, these drugs act to decrease blood pressure by decreasing cardiac output or peripheral vascular resistance. This chapter focuses on ACE inhibitors and ARBs. Various chapters describe other drugs discussed in this chapter—for example, chapters related to heart failure (see Chap. 24), dysrhythmias (see Chap. 25), and angina (see Chap. 26).
Table 28.1 outlines the antihypertensive drugs, and Table 28.2 lists antihypertensive–diuretic combination products. Product labeling and JNC 7 recommendations are the basis for adult dosages. Product labeling and recommendations from the National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents (2004) are the basis for pediatric dosages.
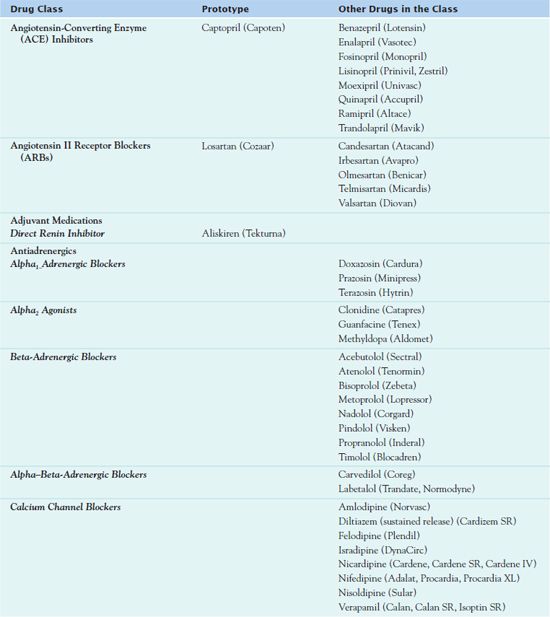
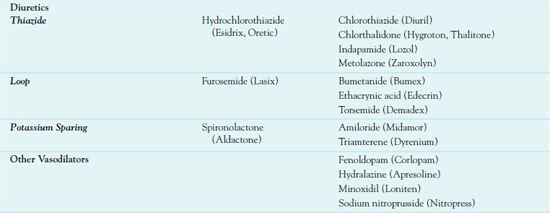
 TABLE 28.2
TABLE 28.2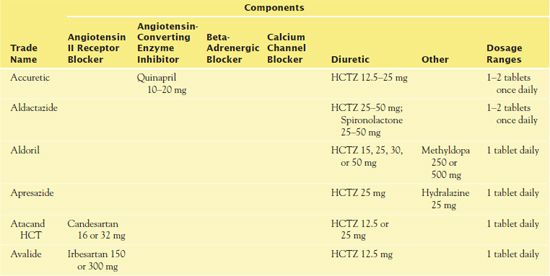
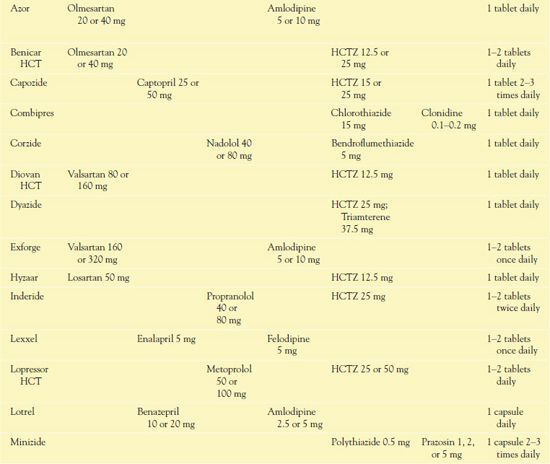
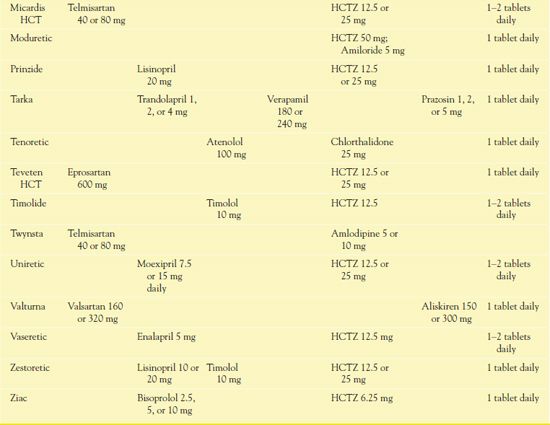
*Note that one trade-name product may be available in multiple formulations, with variable amounts of antihypertensive, diuretic, or both components.
HCTZ, hydrochlorothiazide.
The JNC 7 guidelines suggest thiazide diuretics be used as first-line therapy, either alone (monotherapy) or with a beta blocker, ACE inhibitor, ARB, or calcium channel blocker. If the initial drug (and dose) does not produce the desired blood pressure, options for further management include increasing the dose, substituting another drug, or adding a second drug from a different group. If the response is still inadequate, addition of a second or third drug, including a diuretic if not previously prescribed, is a possibility. When current management is ineffective, it is necessary to reassess the patient’s adherence to lifestyle modifications and drug therapy. In addition, it is also important to review other factors that may decrease the therapeutic response, such as the use of over-the-counter appetite suppressants, dietary or herbal supplements, or nasal decongestants, which raise blood pressure.
The guidelines of the World Health Organization and the International Society of Hypertension for management of hypertension include considering age, ethnicity, and concomitant cardiovascular disorders when choosing an antihypertensive drug; starting with a single drug, in the lowest available dose; changing to a drug from a different group, rather than increasing dosage of the first drug or adding a second drug, if the initial drug is ineffective or not well tolerated; and using long-acting drugs (i.e., a single dose effective for 24 hours). The guidelines also note that many patients require two or more drugs to achieve adequate blood pressure control. When this is the case, fixed-dose combinations or long-acting agents may be preferred, because they decrease the number of drugs and doses that are required and may increase compliance.
Variation exists in the response to drug therapy for hypertension in ethnic populations. Experts credit nearly 70% of the familial considerations related to blood pressure to shared genes rather than to shared environment. For most antihypertensive drugs, few research studies have compared effects among different genetic or ethnic groups. However, several studies indicate that beta blockers have greater effects in people of Asian heritage compared with those of Caucasian background. For hypertension, Asians in general need much smaller doses because they metabolize and excrete beta blockers slowly. Other populations known to metabolize beta blockers slowly include Arab and Egyptian Americans and possibly German Americans. In African Americans, diuretics are effective and recommended as initial drug therapy. Calcium channel blockers, alpha1 receptor blockers, and the alpha–beta blocker labetalol are reportedly equally effective in African Americans and Caucasians. ACE inhibitors, some ARBs (e.g., losartan and telmisartan), and beta blockers are less effective as monotherapy in African Americans. When beta blockers are used, they are usually one component of a multidrug regimen, and higher doses may be necessary. Overall, African Americans are more likely to have severe hypertension and require multiple drugs as a result of having low circulating renin, increased salt sensitivity, and a higher incidence of obesity.
Angiotensin-Converting Enzyme Inhibitors
Authorities recommend  captopril (Capoten), the prototype angiotensin-converting enzyme (ACE) inhibitor, and other drugs in this class as first-line agents for treating hypertension in people with diabetes, particularly those with type 1 diabetes and/or diabetic nephropathy. These drugs reduce proteinuria and slow progression of renal impairment in people with this disease. (However, they may cause or aggravate proteinuria and renal damage in people who do not have diabetes.) ACE inhibitors may be used alone or in combination with other antihypertensive agents, such as thiazide diuretics.
captopril (Capoten), the prototype angiotensin-converting enzyme (ACE) inhibitor, and other drugs in this class as first-line agents for treating hypertension in people with diabetes, particularly those with type 1 diabetes and/or diabetic nephropathy. These drugs reduce proteinuria and slow progression of renal impairment in people with this disease. (However, they may cause or aggravate proteinuria and renal damage in people who do not have diabetes.) ACE inhibitors may be used alone or in combination with other antihypertensive agents, such as thiazide diuretics.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


