Understand the pathophysiology of right-sided and left-sided heart failure.
 Identify the major manifestations of heart failure.
Identify the major manifestations of heart failure.
 Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for the inotrope (cardiac glycoside) drug class.
Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for the inotrope (cardiac glycoside) drug class.
 Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for the phosphodiesterase inhibitors (cardiotonic–inotropic agents).
Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for the phosphodiesterase inhibitors (cardiotonic–inotropic agents).
 Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for human B-type natriuretic peptide.
Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for human B-type natriuretic peptide.
 Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for adjuvant drugs used in the treatment of heart failure.
Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for adjuvant drugs used in the treatment of heart failure.
 Implement the nursing process in the care of patients undergoing drug therapy for heart failure.
Implement the nursing process in the care of patients undergoing drug therapy for heart failure.
Clinical Application Case Study
Dr. Adams is a 59-year-old professor of history at a 4-year college. He states to the nurse practitioner at the campus health center that he has been experiencing shortness of breath and fatigue for the last 4 weeks. The nurse practitioner asks Dr. Adams questions to ascertain his past medical history. He states that he has been taking enalapril maleate, 20 mg one time per day for hypertension. Dr. Adams also states that his ankles seem to be swollen. On examination, the nurse practitioner notes that Dr. Adams has pitting edema in his feet and ankles. The nurse practitioner advises Dr. Adams to make an appointment with his physician immediately. The physician diagnoses Dr. Adams with heart failure and prescribes digoxin (Lanoxin), 0.125 mg every morning, and spironolactone (Aldactone), 25 mg every morning in addition to the enalapril maleate.
KEY TERMS
Catecholamines: active amines (e.g., epinephrine, norepinephrine, dopamine) that have an effect on the cardiovascular system
Decompensation: the inability of the heart to adequately circulate oxygenated blood to the body’s vital organs
Diastolic dysfunction: impaired relaxation and filling of the ventricles during diastole
Digitalis toxicity: an accumulation of digitalis in the body that leads to nausea, vomiting, and atrial tachycardia
Digitalization: the administration of a loading dose of digoxin (Lanoxin) to achieve a therapeutic blood level of the medication more rapidly
Endothelin: a peptide that raises blood pressure, constricts blood vessels, and contributes to the onset of heart failure
Inotropic: related to or influencing the force of myocardial contractility
Renin: an enzyme produced by the kidney that divides angiotensinogen to form angiotensin I, which is then changed to angiotensin II to produce vasoconstriction
Systolic dysfunction: impaired myocardial contraction during systole
Therapeutic index: the blood level of a medication that will produce therapeutic effects
Ventricular remodeling: dilatation and hypertrophy of the ventricles in the initial phases of heart failure, causing the ventricle to assume a spherical shape
Introduction
In this chapter, you are introduced to the pharmacological care of the patient who is experiencing heart failure. Heart failure is a complex clinical condition that occurs when the heart cannot pump enough blood to meet the body tissue’s needs for oxygen and nutrients. Heart failure can result from impaired myocardial contraction during systole (systolic dysfunction), impaired relaxation and filling of ventricles during diastole (diastolic dysfunction), or a combination of both systolic and diastolic dysfunction. Heart failure can result in an accumulation of fluid in the lungs and peripheral tissues.
Overview of Heart Failure
To adequately understand the pharmacologic treatment of heart failure, it is important to understand the causes, pathophysiology, and clinical manifestations of heart failure. It is also important to understand the difference between right-sided and left-sided heart failure.
Etiology
Heart failure is caused by various conditions that prevent the contractile myocardial cells and the endothelial cells that line the heart and blood vessels from functioning properly. Hypertension, cardiomyopathy, and acute myocardial infarction can affect myocardial or endothelial cell function, leading to heart failure. Heart failure can also be caused by volume overload, renal failure, or hypermetabolic states.
Endothelial dysfunction promotes processes that can lead to narrowing of the blood vessel lumen, such as the accumulation of atherosclerotic plaque, abnormal cell growth, inflammation, or platelet activation. The narrowing of the lumen can lead to blood clot formation and vasoconstriction. These are the major factors in coronary artery disease and hypertension and the most common conditions that lead to heart failure.
Hyperthyroidism is a hypermetabolic condition that is a major causative factor in the development of heart failure. Thyroid function is increased, which causes an increase in heart rate and myocardial contractility and ultimately cardiac output. The patient is prone to heart failure due to the increased cardiac output.
Fluid volume overload impairs the pumping ability of the heart, contributing to the development of heart failure. Fluid volume overload can occur in patients with renal failure. Fluid volume overload can also be caused by the excessive administration of intravenous (IV) fluids or blood transfusions, or therapy with certain medications such as corticosteroids, estrogens, and nonsteroidal anti-inflammatory agents (which promote sodium and water retention).
Pathophysiology
Heart failure results in low cardiac output and inadequate filling of the arteries. As a result, the neurohormonal system activates several feedback mechanisms. The baroreceptors in the aortic arch and carotid sinus that normally inhibit sympathetic nervous system activity are blunted in the patient who is experiencing heart failure. This results in high levels of circulating catecholamines (active amines, such as epinephrine, norepinephrine, and dopamine, that have an effect on the cardiovascular system). The circulating catecholamines increase the force of myocardial contractility, as does the increased activity of the sympathetic nervous system. The patient’s heart rate increases, and the blood vessels constrict. Levels of endothelin, a peptide secreted by the endothelial cells, are increased in heart failure. Endothelin is a potent vasoconstrictor and may exert direct toxic effects on the heart.
The renin–angiotensin–aldosterone system is also activated. Renin is an enzyme produced in the kidneys in response to impaired blood flow and tissue perfusion. The release of renin stimulates the production of angiotensin II. Angiotensin II is a powerful vasoconstrictor. Arterial vasoconstriction impairs cardiac function by increasing the resistance (afterload) against which the ventricle ejects blood. This increases the filling pressures inside the heart, which in turn, increases the stress on the heart by stretching the walls of the heart muscle, predisposing the patient to subendocardial ischemia. Patients with severe heart failure have constriction of the arterioles in the cerebral, myocardial, renal, hepatic, and mesenteric vascular beds. This results in increased organ hypoperfusion and dysfunction.
Right-Sided Heart Failure
Right-sided heart failure results from an accumulation of blood in the systemic venous system. There are two pumps within the heart. The right-sided pump pumps unoxygenated blood from the systemic circulation into the pulmonary circulation. Failure of the right-sided pump results in an increase in the right atrial, right ventricular, end-diastolic, and systemic venous pressures.
The causes of right-sided heart failure are stenosis or regurgitation of the pulmonic or tricuspid valves, right-sided ventricular infarction, cardiomyopathy, or recurrent left-sided heart failure. In some cases severe pneumonia, pulmonary embolus, or pulmonary hypertension can result in right-sided heart failure.
Left-Sided Heart Failure
Left-sided heart failure results in a decrease in cardiac output related to an increase in left atrial and left ventricular end-diastolic pressures and congestion in the pulmonary circulation. The left side of the heart normally moves blood from the low-pressure pulmonary circulation to the higher pressure arterial side of the systemic circulation.
Hypoxic Liver Injury
by ELLEN C. EBERT, MD
September 2006, 81(9), 1232–1236
Retrieved: July 13, 2009
Hypoxic liver injury (hypoxic hepatitis) is caused by insufficient hepatic perfusion. It primarily occurs in elderly patients with right-sided heart failure. Factors that precipitate the development of hypoxic liver injury include arrhythmias or pulmonary edema. The patient will have weakness, dyspnea, and right upper quadrant pain. A massive but transient increase in serum transaminase levels in the absence of other acute causes of liver damage is seen. This increase in serum transaminase levels is related to the imbalance between hepatic oxygen supply and demand.
IMPLICATIONS FOR NURSING PRACTICE: When providing care to a geriatric patient with right-sided heart failure, it is important to assess liver enzymes due to the hepatotoxic effects of medications and the possible development of hypoxic liver injury.
Left-sided heart failure is most commonly caused by a myocardial infarction or cardiomyopathy. The patient experiences pulmonary edema at night while supine in bed because the left ventricle cannot pump the blood effectively out of the ventricle into the aorta and the systemic circulation. The pressure in the left atrium increases, resulting in decreased blood flow from the pulmonary vessels. The increase in pulmonary venous pressure forces fluid from the pulmonary capillaries into the alveoli, impairing gas exchange.
Clinical Manifestations
The cardinal manifestations of heart failure are dyspnea and fatigue, which can lead to exercise intolerance and fluid retention. Fluid retention results in the development of pulmonary congestion and peripheral edema. Patients with compensated or asymptomatic heart failure usually have no symptoms at rest and no edema. In these patients, dyspnea and fatigue occur only with activities that require moderate-to high-level exertion. Patients with symptomatic heart failure have symptoms that occur with minimal exertion or at rest, ankle edema, and distention of the jugular vein. These signs and symptoms reflect decompensation (the inability of the heart to adequately circulate oxygenated blood to the body’s vital organs). Acute, severe cardiac decompensation is manifested by pulmonary edema, a medical emergency that requires immediate treatment. Clinical manifestations of heart failure are summarized in Box 24.1.
BOX 24.1 Clinical Manifestations of Heart Failure
Right-Sided Heart Failure
 Edema of the lower extremities
Edema of the lower extremities
 Weight gain
Weight gain
 Dyspnea
Dyspnea
 Fatigue
Fatigue
 Hepatomegaly
Hepatomegaly
 Ascites
Ascites
 Anorexia
Anorexia
 Nausea or abdominal pain
Nausea or abdominal pain
Left-Sided Heart Failure
 Pulmonary congestion
Pulmonary congestion
 Dyspnea with possible orthopnea
Dyspnea with possible orthopnea
 Cough
Cough
 Audible crackles in the bases of the lung
Audible crackles in the bases of the lung
 Audible S3 or ventricular gallop
Audible S3 or ventricular gallop
Drug Therapy
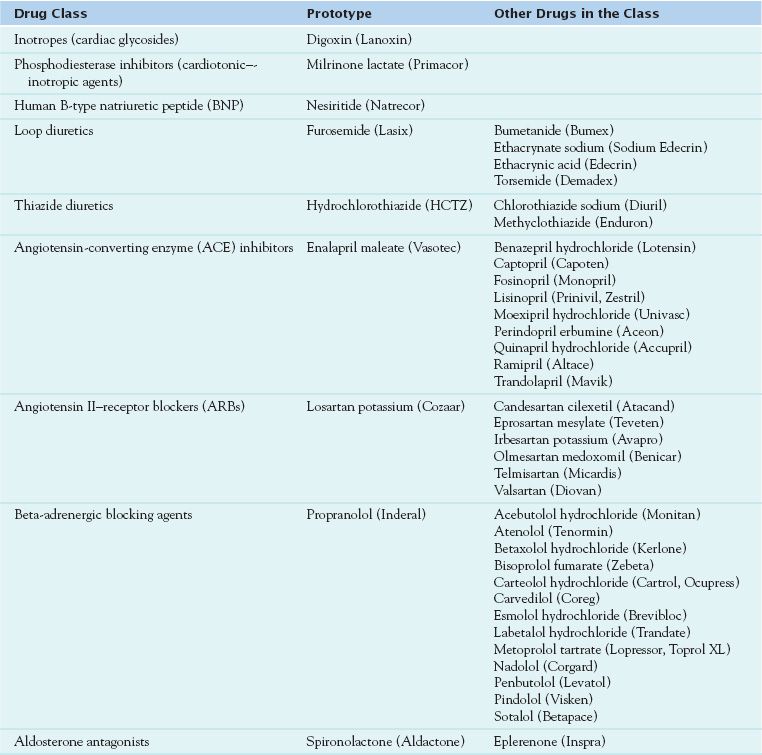
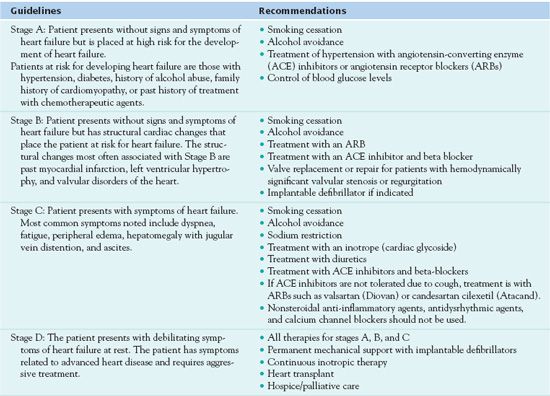
Medications used in the treatment of heart failure are summarized in Table 24.1. Treatment guidelines are based on signs and symptoms (Table 24.2).
Hunt, S. A., Abraham, W. T., Chin, M. H., Feldman, F. A., Francis, G. S., Ganiats, T. G., et al. (2005). ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure for the adult-summary article: A report of the American College of Cardiology/American Heart Association Task Force for Practice Guidelines (writing committee to revise the 2001 Guidelines for the Evaluation and Management of Heart Failure). Retrieved July 14, 2009, from http://www.guidelines.gov/summary/summary.aspx?doc_id=7664
Clinical Application 24-1
 Does Dr. Adams have right-sided or left-sided heart failure?
Does Dr. Adams have right-sided or left-sided heart failure?
NCLEX Success
1. An elderly patient is admitted to the cardiac intensive care unit with right-sided heart failure. Which of the following blood values is most important to monitor based on the patient’s risk factors?
A. complete blood count (CBC)
B. blood glucose
C. bleeding and clotting time
D. liver enzymes
2. A patient is diagnosed with acute myocardial infarction. Which of the following medications will precipitate the development of left-sided heart failure in this patient?
A. ibuprofen (Motrin)
B. furosemide (Lasix)
C. gabapentin (Neurontin)
D. fexofenadine (Allegra)
Inotropes (Cardiac Glycosides)
Inotropes (cardiac glycosides) act to influence the contractility of the heart muscle. (Inotropic means related to, or influencing the force of, myocardial contractility.)  Digoxin (Lanoxin) is the prototype drug of this class. Digoxin is derived from the digitalis plant. It is used to treat heart failure, atrial fibrillation, and atrial flutter.
Digoxin (Lanoxin) is the prototype drug of this class. Digoxin is derived from the digitalis plant. It is used to treat heart failure, atrial fibrillation, and atrial flutter.
Pharmacokinetics
There are various preparations of digoxin. It is primarily given orally either as a tablet or elixir. The elixir is absorbed more effectively than the tablet and is used primarily with infants and children. When digoxin is given orally, absorption varies among available preparations. With tablets, the most frequently used formulation, differences in bioavailability are important because a person who is stabilized on one formulation may be underdosed or overdosed if another formulation is administered. The differences are attributed to the rate and extent of tablet dissolution rather than the amounts of digoxin. Another popular form of the medication is Lanoxicaps, which are liquid-filled capsules. Digoxin is also given by injection and is supplied as 0.25 mg/mL or 0.1 mg/mL. Digoxin dosages are summarized in Table 24.3.
 TABLE 24.3
TABLE 24.3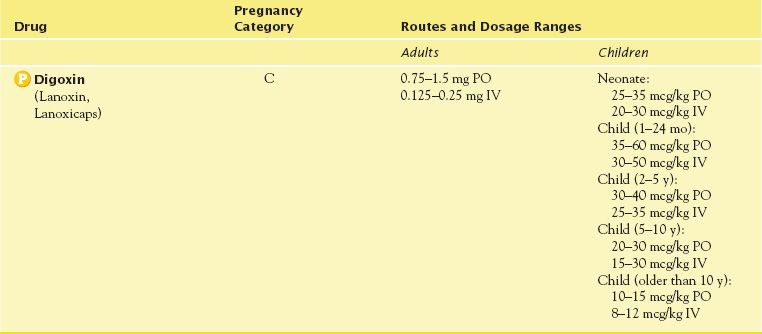
When given orally, the onset of action occurs in 30 minutes to 2 hours, with the peak effect of the medication occurring in approximately 6 hours. When digoxin is given parenterally through the IV route, the onset of action occurs within 10 to 30 minutes and reaches a peak effect in 1 to 5 hours.
Digitalization is the administration of a loading dose (a dose larger than the regular prescribed daily dosage) of digoxin to reach the therapeutic index (the blood level of the medication that will produce therapeutic effects) rapidly. The administration of digoxin for rapid digitalization is usually done for atrial tachydysrhythmias rather than heart failure. The digitalizing dosage schedule requires the nurse to administer a total dose of 0.75 to 1.5 mg of digoxin in divided doses, 6 to 8 hours apart, over a 24-hour period. It is important to note that rapid digitalization places the patient at risk for developing digoxin toxicity. Thus, the nurse must be alert to signs and symptoms of toxicity, which include very slow or very rapid ventricular rhythm, nausea, vomiting, loss of appetite, abdominal distention, blurred vision, and mental changes. During rapid digitalization, the patient is monitored continuously on a cardiac monitor.
Another form of digitalization is slow digitalization. This can be accomplished by initiating therapy with a maintenance dose of digoxin (i.e., a dose administered daily to control symptoms). Digitalization with a maintenance dose will reach therapeutic effects in approximately 1 week. Decreased absorption of digoxin can result in digitalis toxicity (an accumulation of digitalis in the body that leads to nausea, vomiting, and atrial tachycardia). Factors that decrease the absorption of digoxin include the presence of food in the gastrointestinal (GI) tract, malabsorption syndromes, and the concurrent administration of antacids or cholestyramine. The administration of digoxin should take place at least 1 hour before the administration of an antacid. It is important to note that when digoxin is discontinued, it takes approximately 1 week for the drug to be eliminated from the body.
Action
A patient with heart failure is experiencing decreased contractility of the heart, which impairs the heart’s ability to pump blood adequately. Digoxin produces a cardiotonic (positive inotropic) effect that improves the contractility and pumping ability of the heart. Digoxin increases the force of myocardial contractility by inhibiting sodium, potassium, adenosine triphosphatase (Na, K-ATPase), an enzyme in cardiac cell membranes that decreases the movement of sodium out of myocardial cells after contraction. As a result, calcium enters the cell in exchange for sodium, causing additional calcium to be released from intracellular binding sites and increasing myocardial contractility.
In a patient with an atrial dysrhythmia, digoxin slows the rate of ventricular contraction (negative chronotropic effect). Negative chronotropic effects are probably caused by several factors. First, digoxin has a direct depressant effect on cardiac contraction tissues, especially at the atrioventricular (AV) node. This action decreases the number of electrical impulses allowed to reach the ventricles from supraventricular sources. Second, digoxin indirectly stimulates the vagus nerve. Third, increased efficiency of myocardial contraction and vagal stimulation decrease compensatory tachycardia that results from the sympathetic nervous system response to inadequate circulation.
Use of Digoxin in the Treatment of Chronic Heart Failure
by WONG, B., AND FLATTERY, M. P.
Progress in Cardiovascular Nursing
Summer 2006, 158–161
Retrieved: July 22, 2009
This review of literature revealed that digoxin improves symptoms in patients with systolic heart failure with neutral effect on mortality regardless of the presence of atrial fibrillation. Based on guidelines from the Heart Failure Society of America, patients with left ventricular systolic dysfunction and who have persistent symptoms of heart failure should be treated with digoxin, angiotensin-converting enzyme (ACE) inhibitors, beta-blockers, diuretics, and possibly aldosterone antagonists.
IMPLICATIONS FOR NURSING PRACTICE: The nurse must be aware of the effects of all these medications in the treatment of the patient with heart failure. The nurse must assess for adverse effects and the patient’s response to treatment. The nurse must educate the patient and family on the need to these medications to control symptoms of heart failure.
Use
The clinical indications for use of digoxin include the management of heart failure, atrial fibrillation, and atrial flutter. Digoxin is administered to patients with acute or chronic conditions, patients who are being digitalized, or for maintenance therapy.
Use in Children
Digoxin is commonly used in children and has the same indications as in adults. When used in children, digoxin therapy should be prescribed and supervised by a pediatric cardiologist when possible. The response to a given dose varies with age and size. The child’s renal and hepatic function also affect the child’s response to the medication. There may be little difference between a therapeutic dose and a toxic dose. Very small amounts are often given to children. These factors increase the risk for dosage errors in children. In a hospital setting, institutional policies may require that each dose be verified with another nurse before it is administered. Liquid digoxin must be precisely measured in a syringe and the dose should never be rounded. It is imperative that the dosage administered is accurate. Electrocardiographic monitoring is desirable when digoxin therapy is initiated.
As in adults, the dosage of digoxin in children is individualized and carefully titrated. Digoxin is primarily excreted by the kidneys, and the dosage should be reduced in the presence of renal impairment. In general, divided daily doses should be given to infants and children younger than 10 years of age, and adult dosages adjusted to weight should be given to children older than 10 years of age. Larger doses are usually needed to slow a too rapid ventricular rate in children with atrial fibrillation or flutter. Differences in bioavailability of different preparations (parenterals, capsules, tablets, and elixirs) must be considered when switching from one preparation to another.
Neonates vary in tolerance of digoxin, depending on their degree of maturity. Premature infants are especially sensitive to drug effects. The dosage must be reduced, and digitalization should be even more individualized and cautiously approached than in more mature infants and children. Early signs of toxicity in newborns are undue slowing of the sinus rate, sinoatrial (SA) arrest, and prolongation of the P–R interval.
Use in Older Adults
Digoxin is a frequent cause of adverse effects in older adults. Reduced dosages are usually required because of decreased liver or kidney function, decreased lean body weight, and advanced cardiovascular disease. Impaired renal function leads to slower drug excretion and increased risk of accumulation. Dosage must be reduced by approximately 50% with renal failure or concurrent administration of amiodarone hydrochloride (Cordarone), quinidine, nifedipine (Procardia), or verapamil hydrochloride (Calan). These drugs increase the serum digoxin level and increase the risk for toxicity if the dosage is not reduced. The most commonly recommended dose is 0.125 mg daily.
Use in Patients With Renal Impairment
Digoxin must be used cautiously in patients with diminished renal function, because renal impairment delays the drug’s excretion. Both loading and maintenance doses should be reduced. Patients with advanced renal impairment can achieve therapeutic serum concentrations with a dosage of 0.125 mg three to five times per week. In patients with reduced blood flow to the kidneys (e.g., as a result of fluid volume depletion or acute heart failure), digoxin may be reabsorbed in the renal tubules. As a result, less digoxin is excreted through the kidneys, and maintenance doses may need to be even less than the dosage amount calculated according to creatinine clearance.
Digoxin toxicity develops more often and lasts longer in patients with renal impairment. Patients with renal impairment who are receiving digoxin, even in small doses, must be monitored for adverse effects, and serum digoxin levels must be monitored periodically.
Digoxin can be administered with milrinone lactate (Primacor) to control acute, severe heart failure. Milrinone lactate is excreted primarily by the kidneys; thus, renal impairment significantly increases elimination half-life, drug accumulation, and adverse effects. Dosage must be reduced according to the creatinine clearance. The nurse consults the manufacturer’s instructions for reduced dosages related to the creatinine clearance.
Use in Patients With Hepatic Impairment
Hepatic function has little effect on digoxin clearance. Adjustments in the dosage amount are not required for patients with hepatic impairment.
Use in Patients With Critical Illness
Critically ill patients often have multiple cardiovascular and other disorders that require drug therapy. Acute heart failure may be the patient’s primary critical illness. However, that episode of heart failure may be precipitated by other illnesses and treatments that alter fluid balance, impair myocardial contractility, or increase the workload of the heart beyond its capacity to accommodate. Management of the critically ill patient is often symptomatic, with the choice of drug and dosage requiring careful titration and frequent monitoring of the patient’s response. Cardiotonic, diuretic, and vasodilator drugs are often required. All of these medications should be used cautiously in critically ill patients.
Use in Patients Receiving Home Care
Most digoxin is taken at home, and the home care nurse shares the responsibility for teaching patients how to use the drug effectively and how to recognize medication responses that should be reported to the health care provider. Accurate dosing is vitally important because underuse may cause the recurrence of symptoms and overuse may cause toxicity. Either condition may be life-threatening. The nurse instructs the patient and any caregivers that if symptoms of heart failure or digoxin toxicity develop, it is necessary to seek medical intervention immediately. The home care nurse also monitors the patient’s response to the drug and changes in the patient’s condition or drug therapy that increase the patient’s risk for toxicity.
When a patient is receiving a combination of drugs for management of heart failure, the nurse assists the patient in understanding that the different types of drugs have different actions and produce different responses. As a result, the medications work together to be more effective and maintain a more balanced state of cardiovascular function. Changing medications or dosages can upset the balance and lead to acute and severe symptoms that require hospitalization and may even cause death from heart failure. Thus, it is extremely important that the patient takes all the medications that have been prescribed. If the patient is unable to take the medications for any reason, the health care provider should be notified.
Adverse Effects
Because of digoxin’s narrow therapeutic index, the patient is at greater risk for developing digoxin toxicity. Factors that contribute to the development of digoxin toxicity are summarized in Box 24.2. Patients with hypokalemia can develop digoxin toxicity even when the serum digoxin level is not considered to be elevated.
BOX 24.2 Factors That Contribute to Digoxin (Lanoxin) Toxicity



