Give an overview of the cardiac electrophysiology and an outline of specific cardiac dysrhythmias that affect heart rhythm, heart rate, or both.
 Describe principles of therapy in the management of dysrhythmias, including measures that do not involve antidysrhythmic drugs.
Describe principles of therapy in the management of dysrhythmias, including measures that do not involve antidysrhythmic drugs.
 Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for class I sodium channel blockers.
Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for class I sodium channel blockers.
 Identify the prototype and outline the action, use, adverse effects, contraindications, and nursing implications for beta-adrenergic blockers.
Identify the prototype and outline the action, use, adverse effects, contraindications, and nursing implications for beta-adrenergic blockers.
 Identify the prototype and explain the action, use, adverse effects, contraindications, and nursing implications for potassium channel blockers.
Identify the prototype and explain the action, use, adverse effects, contraindications, and nursing implications for potassium channel blockers.
 Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for calcium channel blockers.
Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for calcium channel blockers.
 Describe the nursing process implications and actions related to caring for patients using selected antidysrhythmic drugs.
Describe the nursing process implications and actions related to caring for patients using selected antidysrhythmic drugs.
Clinical Application Case Study
Bill Brown is a 74-year-old man with cardiovascular disease. He has just undergone cardiac bypass surgery for two coronary artery bypasses. During the postoperative period, he develops premature ventricular complexes followed by atrial fibrillation.
KEY TERMS
Antidysrhythmic: medication used for prevention and treatment of a cardiac dysrhythmia.
Automaticity: ability of the heart to generate an electrical impulse.
Conductivity: ability of cardiac tissue to transmit electrical impulses.
Dysrhythmia: abnormality in heart rate or rhythm.
Ectopic: when an electrical impulse arises from an abnormal focus, anywhere other than the sinoatrial node.
Excitability: ability of a cardiac muscle cell to respond to an electrical stimulus.
Prodysrhythmic effects: tendency of antidysrhythmic drugs to cause the development of new dysrhythmias.
Tachydysrhythmia: dysrhythmia of greater than 100 beats per minute.
Introduction
This chapter discusses the antidysrhythmic agents, the medications that are used for prevention and treatment of cardiac dysrhythmias. A dysrhythmia is an abnormality in heart rate or rhythm. It can become significant if it interferes with cardiac function, thereby altering the ability to adequately pump and causing inadequate perfusion of the body tissues.
Overview of Dysrhythmias
Physiology
To aid in understanding antidysrhythmic drug therapy, it is necessary to review the physiology of the cardiac electrophysiologic conduction system. The heart is an electrical pump. The “electrical” activity resides primarily in the specialized tissues that can generate and conduct an electrical impulse. The mechanical or “pump” activity resides in contractile tissue. Normally, the synchronization of these activities results in effective cardiac contraction and distribution of blood throughout the body. Each heartbeat occurs at regular intervals and consists of four events: stimulation from an electrical impulse, transmission of the electrical impulse to adjacent conductive or contractile tissue, contraction of atria and then ventricles, and then relaxation of atria and then ventricles. Certain properties are inherent in cardiac cells. Two of these properties are automaticity and conductivity.
Automaticity
Automaticity is the heart’s ability to generate an electrical impulse. Any part of the conduction system can spontaneously start an impulse, but the sinoatrial (SA) node normally has the fastest rate of automaticity and therefore the faster rate of spontaneous impulse formation.
Initiation of an electrical impulse depends predominately on the movement of sodium and calcium ions into a myocardial cell and movement of potassium ions out of the cell. Normally, the cell membrane becomes more permeable to sodium and opens certain channels to allow rapid movement of sodium into the cell. Calcium ions follow sodium ions into the cell at a slower rate and through different channels. As sodium and calcium ions move into cells, potassium ions move out of cells. The movement of the ions changes the membrane from its resting state of electrical neutrality to an activated state of electrical energy buildup. After the electrical energy is discharged (depolarization), muscle contraction occurs. The ease in which cardiac cells undergoes this series of events is call cardiac excitability.
Conductivity
Conductivity is the ability of cardiac tissue to transmit electrical impulses. The orderly, rhythmic transmission of impulses to all cells is needed for effective myocardial contraction. The cardiac conduction system is shown in Figure 25.1. Normally, electrical impulses originate in the SA node and are transmitted through internodal pathways to the atrioventricular (AV) node, where the impulse is delayed for a period of time. Then the impulse travels through the bundle of His, bundle branches, Purkinje fibers, and throughout the ventricular muscle.

Figure 25.1 The conducting system of the heart. Impulses originating in the sinoatrial (SA) node are transmitted through the atria, into the atrioventricular (AV) node to the Bundle of His, and by way of Purkinje fibers through the ventricles.
Etiology
Cardiac dysrhythmias originate in any part of the conduction system or in atrial or ventricular muscle. They result from disturbances in electrical impulse formation (automaticity), conduction (conductivity), or both. The inherent characteristic of automaticity allows myocardial cells other than the SA node to depolarize and initiate the electrical impulse that culminates in contraction. This may occur when the SA node fails to initiate an impulse or does so too slowly. When the electrical impulse arises anywhere other than the SA node, the focus is abnormal or ectopic. If the ectopic focus depolarizes at a rate faster than the SA node, the ectopic focus becomes the dominant pacemaker. Conditions such as hypoxia, ischemia, or hypokalemia may activate ectopic pacemakers. Ectopic foci indicate myocardial irritability, which can increase responsiveness to stimuli, leading to potentially serious impairment of cardiac function. Atrial fibrillation is the most common dysrhythmia.
Pathophysiology
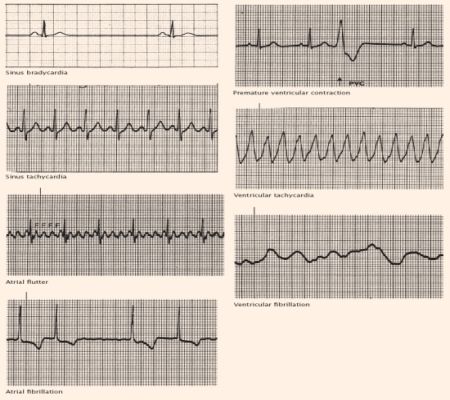
Dysrhythmias may be clinically significant if they interfere with cardiac function and thus alter the heart’s ability to pump sufficient blood to body tissues. The normal heart can maintain an adequate cardiac output with ventricular rates ranging from 40 to 150 beats per minute. The diseased heart, however, may not be able to maintain an adequate cardiac output with heart rates below 60 or above 120 beats per minute. These alterations in rates are referred to as dysrhythmias, which are usually categorized by rate, location, or patterns of conduction. Tachydysrhythmias are heart rates greater than 100 beats per minute. Bradydysrhythmias are those less than 60 beats per minute. Atropine, which is used to treat bradydysrhythmias, is discussed in Chapter 47, and digoxin, which is used to treat atrial fibrillation, is discussed in Chapter 24. Box 25.1 describes various types of dysrhythmias.
BOX 25.1 Types of Dysrhythmias
Clinical Manifestations
Some clinical manifestations of dysrhythmias include shortness of breath, hypotension, and anxiety. Some patients may be noticeably pale in color, and others may be flushed. Syncope or mental confusion may occur. Oliguria may be present. For more information, see The Nursing Process, Assessment.
Nondrug Therapy
Management without the use of drugs may be preferable, at least initially, for several dysrhythmias. For example, sinus tachycardia usually results from such disorders as dehydration, fever, infection, or hypotension, and intervention and management should attempt to relieve the underlying cause. For paroxysmal supraventricular tachycardia with mild or moderate symptoms, Valsalva maneuver, carotid sinus massage, or other measures to increase vagal tone are preferred. For ventricular fibrillation, immediate defibrillation is the initial management of choice.
In addition to these strategies, use of other measures is increasing. The impetus for nonpharmacologic management developed mainly from studies demonstrating that antidysrhythmic drugs could worsen existing dysrhythmias, cause new dysrhythmias, and cause higher mortality rates in patients receiving the drugs than patients not receiving the drugs. Current technology allows clinicians to insert pacemakers and defibrillators (e.g., implantable cardioverter defibrillators) to control bradydysrhythmias or tachydysrhythmias and to use radio waves (radiofrequency catheter ablation) or surgery to deactivate ectopic foci.
Drug Therapy
All drugs used to combat dysrhythmias alter the electrical conduction system of the heart. The drugs used for the treatment of tachydysrhythmias are the focus of this chapter. They reduce automaticity, which is the spontaneous depolarization of myocardial cells, including ectopic pacemakers. They also slow conduction of electrical impulses through the heart and prolong the refractory period of myocardial cells so they are less likely to be prematurely activated by adjacent cells. Antidysrhythmic drug therapy is commonly indicated in the following conditions:
• Conversion of atrial fibrillation or atrial flutter to normal sinus rhythm (NSR)
• Maintaining NSR after conversion from atrial fibrillation or atrial flutter
• Suppression of a fast or irregular ventricular rate, which alters the cardiac output. Altered cardiac output leads to symptoms of decreased coronary, cerebral, and/or systemic circulation.
• Presence of dangerous dysrhythmias that may be fatal if not quickly terminated. For example, ventricular tachycardia may cause cardiac arrest.
The clinical use of antidysrhythmic drugs for tachydysrhythmias has changed over the years. Clinicians use drugs not just to suppress dysrhythmias but to prevent or relieve symptoms or prolong survival. Symptoms may manifest as shortness of breath, anxiety, or racing heart. This change resulted from study outcomes in which patients treated for some dysrhythmias had a higher mortality rate than patients who did not receive antidysrhythmic drug therapy. Researchers attributed the higher mortality rate to prodysrhythmic effects, which are those effects that worsen existing dysrhythmias or cause new dysrhythmias.
Many of the agents used to treat dysrhythmias are in fact prodysrhythmics. Thus, rational drug therapy for a cardiac dysrhythmia requires accurate identification of the dysrhythmia, understanding of the basic mechanisms causing the dysrhythmia, observation of the hemodynamic and electrocardiogram (ECG) effects of the dysrhythmia, knowledge of the pharmacologic actions of specific antidysrhythmic drugs, and the expectation that therapeutic effects will outweigh potential adverse effects. Even when these criteria are met, antidysrhythmic drug therapy is somewhat empiric.
Several different groups of drugs function as antidysrhythmics. They are classified according to their mechanisms of action and effects on the conduction system, even though they differ in other respects. Some drugs have characteristics of more than one group. There are various types of antidysrhythmics: class I sodium channel blockers, class II beta-adrenergic blockers, class III potassium channel blockers, and class IV calcium channel blockers (Table 25.1).

A-fib, atrial fibrillation; PVC, premature ventricular contractions; SVT, supraventricular tachycardia; V-fib, ventricular fibrillation; VT, ventricular tachycardia.
Class I Sodium Channel Blockers
Class I drugs block cardiac sodium channels and slow conduction velocity, prolonging refractoriness and decreasing automaticity of sodium-dependent tissue. This results in a membrane-stabilizing effect and also decreases formation and conduction of electrical impulses. Within the category of class I drugs are subcategories, the class IA, class IB, and class IC medications.
CLASS IA
The prototype class IA drug is  quinidine. Table 25.2 presents dosages for quinidine and the other class IA sodium channel blockers.
quinidine. Table 25.2 presents dosages for quinidine and the other class IA sodium channel blockers.
 TABLE 25.2
TABLE 25.2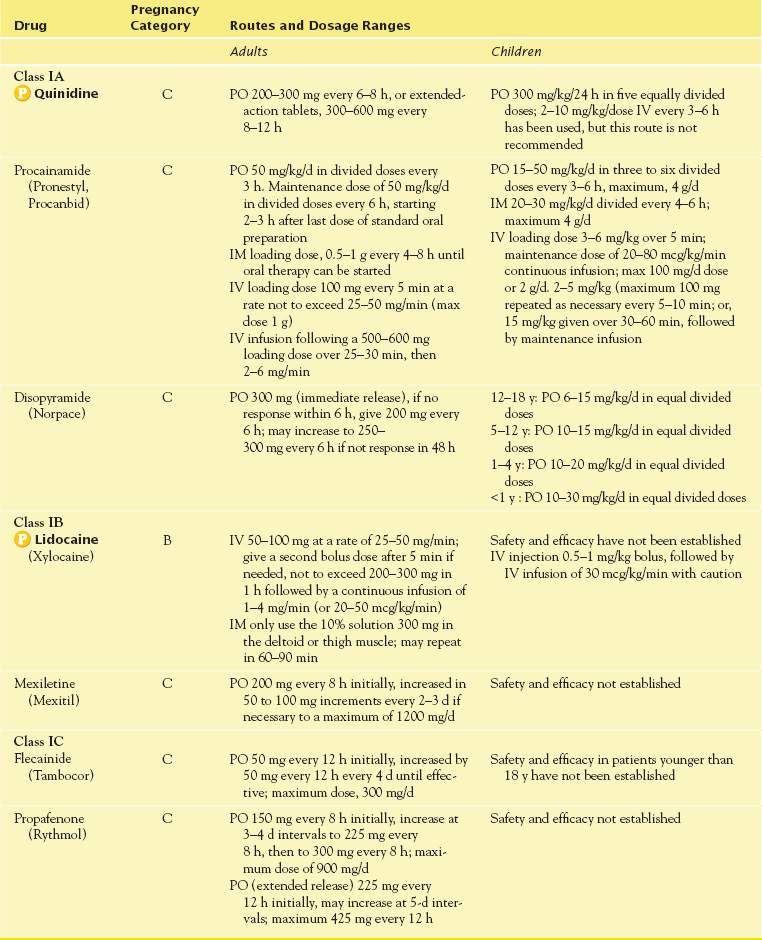
Pharmacokinetics
Quinidine is well absorbed after oral administration, with a usual onset of 1 to 3 hours. After intramuscular (IM) administration, onset occurs within 30 to 90 minutes, and after intravenous (IV) administration, onset is rapid. Therapeutic serum levels (2-6 mcg/mL) are attained within 1 hour and persist for 6 to 8 hours. (Serum levels greater than 6 mcg/mL are toxic.) Quinidine is highly bound to serum albumin and has a half-life of about 6 to 7 hours. It is metabolized by the liver (about 80%) and excreted in the urine (about 20%) as well as the feces. In alkaline urine (i.e., pH > 7), renal excretion of quinidine decreases, and serum levels may rise.
Action
Quinidine reduces automaticity and slows conduction throughout the cardiac system. In addition, it prolongs the refractory period of the myocardial cells.
Use
Indications for quinidine include the treatment of (1) atrial dysrhythmias and (2) paroxysmal supraventricular tachycardia or chronic ventricular tachycardia without heart block. However, the drug is usually contraindicated in patients with severe, uncompensated heart failure or with heart block because it depresses myocardial contractility and conduction through the AV node. For disopyramide, another class IA drug, the Food and Drug Administration (FDA) has issued a BLACK BOX WARNING ♦ because of the drug’s known prodysrhythmic properties; the drug should be reserved for patients with life- threatening ventricular dysrhythmias.
Use in Children
Pediatric patients take quinidine in the oral form. Although the IV route may be used, it is not recommended.
Use in Older Adults
There are no recommendations for precautions regarding the use of quinidine in older adults. However, because of the likelihood that aging may result in renal and hepatic problems, precautions regarding the use of quinidine in older patients should be considered.
Use in Patients With Renal Impairment
Reduced dosages of quinidine are necessary, with close monitoring. Caution is necessary, especially in patients with renal tubular acidosis.
Use in Patients With Hepatic Impairment
Hepatic impairment increases the plasma half-life of several antidysrhythmic drugs, including quinidine, and patients with hepatic impairment usually receive a reduced dosage. Close monitoring is essential. In addition, caution is warranted, especially in patients with hepatic insufficiency.
Use in Patients With Critical Illness
Critically ill patients often have multiple cardiovascular disorders as well as other conditions that increase the risk of acute, serious, and potentially life-threatening dysrhythmias. Patients may also have refractory dysrhythmias that require strong, potentially toxic antidysrhythmic drugs. Thus, antidysrhythmic drugs are often given intravenously in critical care settings for rapid reversal of a fast rhythm. After reversal, transitioning from IV drugs to oral ones is often necessary to prevent recurrence of the dysrhythmia. Frequently, potentials for renal and/or hepatic involvement are greater in patients who are critically ill. It is important to monitor responses to quinidine carefully, especially when beginning therapy.
Use in Patients Receiving Home Care
Patients receiving chronic antidysrhythmic drug therapy are likely to have significant cardiovascular disease. At each visit to the home, the nurse assesses the patient’s physical, mental, and functional status and evaluates pulse and blood pressure. In addition, he or she also instructs patients and caregivers to report symptoms (e.g., dizziness or fainting, chest pain) and avoid over-the-counter agents unless approved by a health care provider.
Adverse Effects
Adverse effects of quinidine include central nervous system (CNS) changes, cardiac dysrhythmias, and gastrointestinal (GI) changes, as well as hematologic and hypersensitivity alterations. Most of the CNS changes relate to vision changes, including photophobia, blurring, loss of night vision, and diplopia. Cardiac dysrhythmias include conduction disturbances, including heart block and hypotension. GI effects include nausea, vomiting, diarrhea, and liver toxicity.
Contraindications
Quinidine is contraindicated in patients with an allergy to the drug. It is also contraindicated in second-or third-degree heart block, myasthenia gravis, pregnancy, lactation, and thrombocytopenic purpura.
Nursing Implications
Prior to the start of any new therapy, it is necessary to assess for allergies, second-or third-degree heart block, myasthenia gravis, pregnancy, lactation, and thrombocytopenic purpura. Physical assessment includes inspection of skin for color and the presence of lesions, determination of orientation status, assessment of cranial nerves, determination of bilateral grip strength and reflexes, auscultation of pulse and blood pressure, interpretation of the ECG, checking for edema, and auscultation of bowel sounds. It is also necessary to evaluate hepatic and renal function as well as to perform a urinalysis and complete blood count. The findings of the physical assessment as well as results of the laboratory work and diagnostic tests help develop the nursing plan of care for the patient who is beginning sodium channel blocker therapy.
Preventing Interactions
Preventing drug-drug and drug-food interactions requires knowledge of potential effects. Several medications interact with quinidine, increasing or decreasing its effect (Box 25.2). Use of quinidine with certain other drugs has specific results. With succinylcholine, neuromuscular blocking effects may increase. With digoxin, increased digoxin level and toxicity result. With oral anticoagulants, anticoagulant effect increases, and bleeding may occur. In addition, grapefruit juice, when given with quinidine, decreases the metabolism of quinidine and increases the risk of toxic drug effects.
BOX 25.2  Drug Interactions: Quinidine
Drug Interactions: Quinidine
Drugs That Increase the Effects of Quinidine
 Cimetidine, amiodarone, verapamil
Cimetidine, amiodarone, verapamil
Increase the risk of possible quinidine toxicity
Drugs That Decrease the Effects of Quinidine
 Sodium bicarbonate
Sodium bicarbonate
Increases cardiac depressant effects
 Phenobarbital, hydantoins, rifampin, sucralfate
Phenobarbital, hydantoins, rifampin, sucralfate
Decrease the levels of quinidine, leading to dysrhythmias
Administering the Medication
When administering quinidine in the IV form, preparation includes diluting 800 mg in 50 mL of 5% dextrose. With an IV infusion, it is necessary to inject the quinidine slowly at a rate of 1 mL/min. The nurse should note that if Y-site administration is needed, quinidine is not compatible with furosemide.
Assessing for Therapeutic Effects
The nurse assesses for improvement in symptoms and for return of an organized cardiac rhythm. Physical assessment includes inspection of skin for adequate color and perfusion, clear mentation, and pulse and blood pressure within the patient’s normal limits. It is also necessary to evaluate the adequacy of hepatic and renal function through laboratory testing.
Assessing for Adverse Effects
The nurse monitors patients who are taking quinidine for adverse effects. Physical assessment of the body systems that are potentially affected by the action of quinidine provide this surveillance. Of particular concern are the CNS, cardiac, GI, and hematologic systems, as well as possible hypersensitivity. It is necessary to determine whether adverse effects, particularly diarrhea, are manageable and are not complicating treatment.
Patient Teaching
The nurse gives teaching points to each patient to empower the patient and encourage and foster an environment inclusive of the patient’s opinion and perspective. Quinidine, like any other drug, is taken exactly as prescribed. Sustained-release tablets should not be chewed. If GI upset occurs, then the medication may be taken with food. The nurse reminds the patient that frequent cardiac monitoring and blood tests are important for follow-up; these include regular checks of heart rhythm and blood counts. The patient teaching guidelines presented in Box 25.3 are important.
BOX 25.3  Patient Teaching Guidelines for Antidysrhythmic Drugs
Patient Teaching Guidelines for Antidysrhythmic Drugs
 A fast heartbeat normally occurs in response to exercise, fever, and other conditions so that more blood can be pumped and carried to body tissues. An irregular heartbeat occurs occasionally in most people. However, when your health care provider prescribes a long-term medication to slow or regularize your heartbeat, this means that you have a potentially serious condition. In addition, the medications can cause potentially serious adverse effects. So, it is extremely important that you take the medications exactly as prescribed. Taking extra doses is dangerous; skipping doses or waiting longer between doses may lead to loss of control of the heart problem.
A fast heartbeat normally occurs in response to exercise, fever, and other conditions so that more blood can be pumped and carried to body tissues. An irregular heartbeat occurs occasionally in most people. However, when your health care provider prescribes a long-term medication to slow or regularize your heartbeat, this means that you have a potentially serious condition. In addition, the medications can cause potentially serious adverse effects. So, it is extremely important that you take the medications exactly as prescribed. Taking extra doses is dangerous; skipping doses or waiting longer between doses may lead to loss of control of the heart problem.
 You may be given a drug classified as an antidysrhythmic or a drug from another group that has antidysrhythmic effects (e.g., a beta blocker such as propranolol, a calcium channel blocker such as diltiazem or verapamil). Follow the instructions for the specific drug ordered.
You may be given a drug classified as an antidysrhythmic or a drug from another group that has antidysrhythmic effects (e.g., a beta blocker such as propranolol, a calcium channel blocker such as diltiazem or verapamil). Follow the instructions for the specific drug ordered.
 Be sure you know the names (generic and brand) of the medication, why you are receiving it, and what effects you can expect (therapeutic and adverse).
Be sure you know the names (generic and brand) of the medication, why you are receiving it, and what effects you can expect (therapeutic and adverse).
 You will need continued medical supervision, along with periodic measurements of heart rate and blood pressure, blood tests, and electrocardiograms. Be sure to keep all health care appointments.
You will need continued medical supervision, along with periodic measurements of heart rate and blood pressure, blood tests, and electrocardiograms. Be sure to keep all health care appointments.
 Try to learn the triggers for your irregular heartbeats and avoid them when possible (e.g., excessive caffeinated beverages, strenuous or excessive exercise).
Try to learn the triggers for your irregular heartbeats and avoid them when possible (e.g., excessive caffeinated beverages, strenuous or excessive exercise).
 Avoid over-the-counter cold and asthma remedies, appetite suppressants, and antisleep preparations, which are all stimulants that can cause or aggravate irregular heartbeats.
Avoid over-the-counter cold and asthma remedies, appetite suppressants, and antisleep preparations, which are all stimulants that can cause or aggravate irregular heartbeats.
 Take or give medications at evenly spaced intervals to maintain adequate blood levels. Take your medications at the same time each day.
Take or give medications at evenly spaced intervals to maintain adequate blood levels. Take your medications at the same time each day.
 Take amiodarone, mexiletine, and quinidine with food to decrease gastrointestinal symptoms.
Take amiodarone, mexiletine, and quinidine with food to decrease gastrointestinal symptoms.
 Do not crush or chew sustained-release tablets or capsules.
Do not crush or chew sustained-release tablets or capsules.
 Do not drink grapefruit juice if you are taking quinidine.
Do not drink grapefruit juice if you are taking quinidine.
 Wear a medical alert tag if recommended stating the health condition you have or the medications you are taking.
Wear a medical alert tag if recommended stating the health condition you have or the medications you are taking.
 Report dizziness or fainting spells to your health care provider. This may mean the medication is decreasing your blood pressure too much, which is more likely to occur when starting or increasing the dose of an antidysrhythmic drug. Drug dosages may need to be adjusted.
Report dizziness or fainting spells to your health care provider. This may mean the medication is decreasing your blood pressure too much, which is more likely to occur when starting or increasing the dose of an antidysrhythmic drug. Drug dosages may need to be adjusted.
 Report any change in vision and complaints of nausea or vomiting, sun sensitivity, tremors, or loss of coordination to your health care provider. In addition, report unusual bleeding or bruising, fever, chills, intolerance to heat or cold, shortness of breath, difficulty breathing, cough, swelling of ankles or fingers, palpitation, or difficulty with vision.
Report any change in vision and complaints of nausea or vomiting, sun sensitivity, tremors, or loss of coordination to your health care provider. In addition, report unusual bleeding or bruising, fever, chills, intolerance to heat or cold, shortness of breath, difficulty breathing, cough, swelling of ankles or fingers, palpitation, or difficulty with vision.



