Describe the basic structures and functions of the eye.
 Understand the pathophysiology of glaucoma as well as ocular infections and inflammation.
Understand the pathophysiology of glaucoma as well as ocular infections and inflammation.
 Identify the prototypes and describe the action, use, adverse effects, contraindications, and nursing implications for medications administered for diagnosis and treatment of ocular disorders.
Identify the prototypes and describe the action, use, adverse effects, contraindications, and nursing implications for medications administered for diagnosis and treatment of ocular disorders.
 Identify the prototypes and describe the action, use, adverse effects, contraindications, and nursing implications for medications administered for glaucoma.
Identify the prototypes and describe the action, use, adverse effects, contraindications, and nursing implications for medications administered for glaucoma.
 Identify the prototypes and describe the action, use, adverse effects, contraindications, and nursing implications for medications administered for ocular infections and inflammation.
Identify the prototypes and describe the action, use, adverse effects, contraindications, and nursing implications for medications administered for ocular infections and inflammation.
 Understand how to implement the nursing process in the care of the patient with an ocular disorder.
Understand how to implement the nursing process in the care of the patient with an ocular disorder.
Clinical Application Case Study
Irene Molnar is a 75-year-old woman who has open-angle glaucoma. Her physician has prescribed the following: acetazolamide (Diamox), 250 mg orally, every 6 hours; timolol (Timoptic), one drop in each eye, twice daily; and pilocarpine (Isopto-Carpine), one drop of 2% solution in each eye, three times daily. You are a home care nurse visiting Mrs. Molnar.
KEY TERMS
Conjunctiva: mucous membrane lining the eyelids
Glaucoma: group of diseases characterized by optic nerve damage and changes in visual fields, which is characterized by increased intraocular pressure (IOP) (greater than 22 mm Hg), although it may also occur with normal IOP (less than 21 mm Hg); one of the leading causes of blindness in the United States
Intraocular pressure (IOP): pressure inside the eye; normally less than 21 mm Hg (average 15—16 mm Hg)
Keratitis: inflammation of the cornea
Lacrimation: production of tears
Miosis: pupil constriction
Mydriasis: pupil dilation
Nasolacrimal occlusion: application of pressure to the tear duct
Refraction: deflection of light rays in various directions according to the density of the ocular structures through which they pass
Tonometry: diagnostic test to measure the pressure inside the eye to determine if glaucoma is present
Introduction
This chapter introduces the eye and its disorders. It addresses the drug therapy implemented to enhance visualization of the eye for eye examination and the drug therapy for ocular disorders, including glaucoma, ocular infection, and ocular inflammation.
Basic Structure and Function of the Eye
The eye is the major sensory organ through which a person receives information about the external environment. Extensive discussion of vision and ocular anatomy is beyond the scope of this chapter, but some characteristics and functions are described to facilitate understanding of ocular drug therapy.
The eyelids and lacrimal system function to protect the eye. The eyelid is a barrier to the entry of foreign bodies, strong light, dust, and other potential irritants. The conjunctiva is the mucous membrane lining the eyelids. The canthi (singular, canthus) are the angles where the upper and lower eyelids meet. The lacrimal system produces a fluid that constantly moistens and cleanses the anterior surface of the eyeball. The fluid drains through two small openings in the inner canthus and flows through the nasolacrimal duct into the nasal cavity. When the conjunctiva is irritated or certain emotions are experienced (e.g., sadness), the lacrimal gland produces more fluid than the drainage system can accommodate. The excess fluid overflows the eyelids and becomes tears. Production of tears is known as lacrimation.
The eyeball is a spherical structure composed of the sclera, cornea, choroid, and retina, plus special refractive tissues. The sclera is a white, opaque, fibrous tissue that covers the posterior five sixths of the eyeball. The cornea is a transparent, special connective tissue that covers the anterior sixth of the eyeball. It contains no blood vessels. The choroid, composed of blood vessels and connective tissue, continues forward to form the iris. The iris is composed of pigmented cells, the opening called the pupil, and muscles that control the size of the pupil by contracting or dilating in response to stimuli. Pupil constriction is called miosis, and pupil dilation is called mydriasis. The retina is the innermost layer of the eyeball.
For vision to occur, light rays must enter the eye through the cornea; travel through the pupil, lens, and vitreous body (discussed below); and be focused on the retina. Light rays do not travel directly to the retina. Instead, they are deflected in various directions according to the density of the ocular structures through which they pass. This process, called refraction, is controlled by the aqueous humor, lens, and vitreous body. The optic disk is the area of the retina where ophthalmic blood vessels and the optic nerve enter the eyeball.
The structure and function of the eyeball are further influenced by the lens, aqueous humor, and vitreous body. The lens is an elastic, transparent structure; its function is to focus light rays to form images on the retina. It is located behind the iris and is held in place by ligaments attached to the ciliary body. The aqueous humor is a clear fluid produced by capillaries in the ciliary body. Most of the fluid flows through the pupil into the anterior chamber (between the cornea and the lens and anterior to the iris). A small amount flows into a passage called Schlemm’s canal, from which it enters the venous circulation. Normally, production and drainage of aqueous humor are approximately equal, and the intraocular pressure (IOP) is normal. Impaired drainage of aqueous humor causes increased IOP. The vitreous body is a transparent, jelly-like mass located in the posterior portion of the eyeball. It functions to refract light rays and maintain the normal shape of the eyeball.
Overview of Disorders of the Eye
The eye is subject to many disorders that threaten its structure, function, or both. Some disorders in which ophthalmic drugs play a prominent role are discussed in this section.
Specific Disorders of the Eye
Refractive Errors
Refractive errors include myopia (nearsightedness), hyperopia (farsightedness), presbyopia, and astigmatism. These conditions impair vision by interfering with the eye’s ability to focus light rays on the retina. Ophthalmic drugs are used only in the diagnosis of the conditions; treatment involves prescription of eyeglasses or contact lenses.
Glaucoma
Glaucoma is one of the leading causes of blindness in the United States and the most common cause of blindness in African Americans. It is a group of diseases characterized by optic nerve damage and changes in visual fields. It is often characterized by increased IOP (above 22 mm Hg) but may also occur with normal IOP (below 21 mm Hg; average 15-16 mm Hg). Diagnostic tests for glaucoma include ophthalmoscopic examination of the optic disk; measurement of IOP, or tonometry; and testing of visual fields.
Ocular Infections and Inflammation
Ocular infections may result from foreign bodies, contaminated hands, contaminated eye medications, or infections in contiguous structures (e.g., nose, face, sinuses). Ocular inflammation may be caused by bacteria, viruses, allergic reactions, or irritating chemicals. These conditions include the following:
• Conjunctivitis, which is inflammation of the conjunctiva
• Blepharitis, which is a chronic infection of glands and lash follicles on the margins of the eyelids
• Keratitis, which is inflammation of the cornea
• Corneal ulcers
• Fungal infections
Etiology
Refractive errors of the eye result in impaired vision. Light rays cannot focus sharply on the retina if the eyeball is lengthened or shortened. When the distance to the eyeball is shortened, the visual image is focused at the front of the retina, resulting in myopia. If the focus is beyond the retina, the result is hyperopia. The most common cause of refractive errors is astigmatism or an irregular curve of the cornea.
The cause of open-angle glaucoma is unknown, but contributing factors include advanced age; family history of glaucoma and elevated IOP; diabetes mellitus; hypertension; myopia; long-term use of corticosteroid drugs; and previous eye injury, inflammation, or infection. The incidence of glaucoma in African Americans is about three times higher than in non-African Americans. Closed-angle glaucoma may occur when pupils are dilated and the outflow of aqueous humor is blocked. Inflammatory or infectious conditions may be caused by several factors.
Conjunctivitis, a common eye disorder, may be caused by allergens (e.g., airborne pollens), bacterial or viral infections, or physical or chemical irritants. Bacterial conjunctivitis is often caused by Staphylococcus aureus, Streptococcus pneumoniae, or Haemophilus influenzae. Conjunctivitis with a purulent discharge is caused by Neisseria gonorrhoeae infection. Neonates are infected as they pass through the birth canal of infected mothers. Neonates can also develop keratoconjunctivitis if mothers are infected with Chlamydia trachomatis. Blepharitis, a chronic ocular condition, refers to a family of inflammatory disease processes of the eyelid(s). The condition usually results from seborrhea and staphylococcal infections. Keratitis results from infection with microorganisms, trauma, allergy, ischemia, and drying of the cornea (e.g., from inadequate lacrimation).
Corneal ulcers may be bacterial, fungal, or viral. Bacterial ulcers most often occur because of infections with pneumococci and staphylococci. Pseudomonal ulcers are less common. Fungal ulcers may follow topical corticosteroid therapy or injury with plant matter, such as a tree branch. Viral ulcers are usually caused by the herpesvirus. Other fungal infections may often be attributed to frequent use of ophthalmic antibiotics and corticosteroids.
Pathophysiology
As previously stated, refractive errors impair vision by interfering with the eye’s ability to focus light rays on the retina. When the dimension of the eyeball is too short, near images are blurred. Conversely, if the eyeball dimension is too long, distant objects will be blurred.
Glaucoma is characterized by increased IOP, possibly damaging the optic nerve, which transmits images to the brain. If damage to the optic nerve from high IOP continues, glaucoma leads to loss of vision. The most common type of glaucoma is open-angle glaucoma, which is characterized by IOP. In this type of glaucoma, there is no obstruction at the iridocorneal angle. This form of open-angle glaucoma most commonly occurs due to an abnormality of the trabecular meshwork that controls the flow of aqueous humor into the canal of Schlemm. A secondary form of open-angle glaucoma occurs with the formation of red cell fragments after trauma or iris pigment epithelial granules clogging the trabecular mesh. Closed-angle glaucoma is usually an acute situation requiring emergency surgery. It may occur when pupils are dilated and the outflow of aqueous humor is blocked.
Inflammatory or infectious conditions may lead to conjunctivitis, blepharitis, keratitis, bacterial corneal ulcers, or fungal infections of the eye. Conjunctivitis typically is a self-limited process. However, depending on the immune status of the patient and the etiology, conjunctivitis can progress to more severe and sight-threatening infections. Blepharitis involves bacterial colonization of the eyelids, which results in direct microbial invasion of tissues, immune system-mediated damage, or damage caused by the production of bacterial toxins, waste products, and enzymes. Keratitis may not initially affect vision. However, if the condition is not treated effectively, corneal ulceration, scarring, and impaired vision may result. In non-ulcerative keratitis, the layers of the epithelium are affected but remain intact. Ulcerative keratitis affects the epithelium, stroma, or both. Chronic ulcerative keratitis will result in deformities of the eyelid, paralysis of the lid muscles, or severe exophthalmos.
Clinical Manifestations
Refractive errors are manifested by loss of near or far vision. Glaucoma is characterized by blurred vision, halos around lights, difficulty focusing, difficulty adjusting to low lighting, loss of peripheral vision, headache, and aching around the eye. Conjunctivitis involves redness, tearing, itching, edema, and burning or gritty sensations. Blepharitis is an inflammation of the anterior or posterior structures of the eyelids. Anterior blepharitis presents with burning, redness, and itching of the anterior eyelids. Posterior blepharitis is eyelid inflammation with inflammation of the meibomian glands. An infected sebaceous gland is noted as a hordeolum or stye-producing pain, redness, and swelling of the site. Keratitis is characterized by irritation, increased tear production, and photophobia. Corneal ulcers and fungal infections also produce eye pain, discharge, changes in vision, swelling, and redness.
Clinical Application 58-1
• Mrs. Molnar has been diagnosed with open-angle glaucoma. What is the pathophysiology of this disease?
• If untreated, what is the outcome of this disease?
NCLEX Success
1. A nursing student is reviewing a 72-year-old man’s chart. In the diagnostic section of the chart, the student notices that the man’s intraocular pressure is 23 mm Hg. What should the student suspect regarding this pressure?
A. glaucoma
B. blepharitis
C. diminished vision
D. macular degeneration
2. When applying mascara, a woman may have scratched her cornea. She states she does not have time to go to the ophthalmologist. What ocular disorder could this result in?
A. corneal redness
B. corneal ulceration
C. blepharitis
D. conjunctivitis
Drug Therapy
Drug therapy of ophthalmic conditions is unique because of the location, structure, and function of the eye. Many systemic drugs are unable to cross the blood-eye barrier and achieve therapeutic concentrations in ocular structures. In general, penetration is greater if the drug achieves a high concentration in the blood, is fat soluble, is poorly bound to serum proteins, and if inflammation is present.
Because of the difficulties associated with systemic therapy, various methods of administering drugs locally have been developed. The most common and preferred method is topical application of ophthalmic solutions or suspensions (eye drops) to the conjunctiva. Drugs are distributed through the tear film covering the eye and may be used for superficial disorders (e.g., conjunctivitis) or for relatively deep ocular disorders (e.g., glaucoma). Topical ophthalmic ointments may also be used. In addition, ophthalmologists may inject medications (e.g., antibiotics, corticosteroids, local anesthetics) into or around various eye structures. A major use of topical ophthalmic drugs in children is to dilate the pupil and paralyze accommodation for ophthalmoscopic examination. As a general rule, practitioners prefer the short-acting mydriatics and cycloplegics (e.g., cyclopentolate, tropicamide) because they cause fewer systemic adverse effects than atropine and scopolamine. In addition, children usually receive lower drug concentrations (given empirically) because of their smaller size and the potential risk of systemic adverse effects.
Drug Therapy for the Diagnosis and Treatment of Ocular Disorders
Drugs used to diagnose or treat ophthalmic disorders represent numerous therapeutic classifications, most of which are discussed in other chapters. This chapter describes the major classes of drugs used in ophthalmology. Later, the chapter discusses drugs used in the treatment of glaucoma. Table 58.1 summarizes the medications used to diagnose and treat some ocular disorders. Ocular medications are administered topically with limited systemic effects.
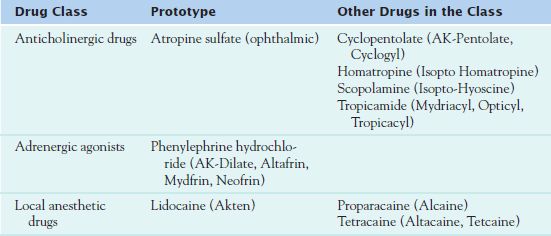
ANTICHOLINERGIC DRUGS
Anticholinergic drugs dilate the pupil to provide greater observation of the inner aspect of the eye. The prototype of this class is  atropine sulfate (ophthalmic).
atropine sulfate (ophthalmic).
Pharmacokinetics and Action
The onset of action of atropine (ophthalmic) is 5 to 10 minutes, with a peak of action in 30 to 40 minutes and a duration of action of 7 to 14 days. Metabolism occurs in the liver, and excretion takes place in the urine.
Atropine (ophthalmic) blocks the effects of acetylcholine in the central nervous system (CNS). It produces mydriatic effects by relaxing the pupil of the eye and prevents accommodation of near vision.
Use
Diagnostic use of atropine (ophthalmic) involves production of mydriasis and cycloplegia-pupillary dilation in acute and inflammatory conditions of the iris and uveal tract. Other uses include measurement of refractive errors and treatment of uveitis. Table 58.2 presents route and dosage information for atropine and related drugs in adults and children.
 TABLE 58.2
TABLE 58.2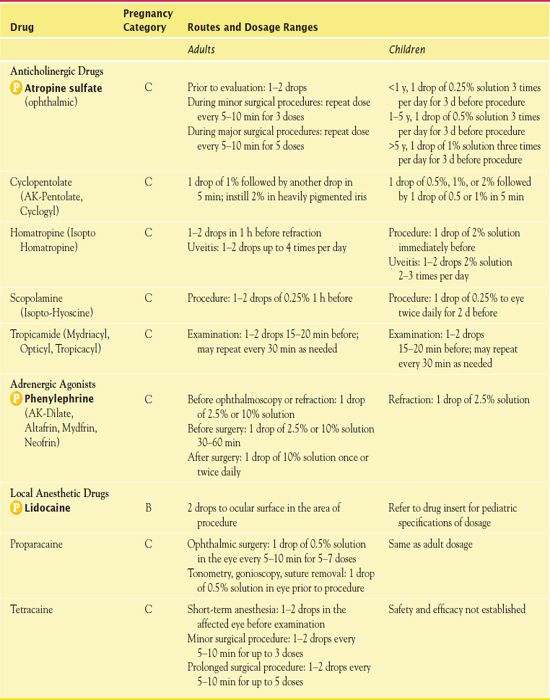
Adverse Effects and Contraindications
Atropine (ophthalmic) may cause local transient stinging. The systemic effects of this medication depend on the amount of medication absorbed and rarely lead to an inhibition of vagal stimulation affecting the heart or diminished bronchial or gastric secretions.
Contraindications to atropine (ophthalmic) include the presence of glaucoma or the tendency to this condition.
Nursing Implications
Administering the Medication
For uveitis, it is necessary to instill one to two drops of atropine (ophthalmic) in the eye 1 hour prior to examination or three times per day to decrease inflammation of the iris and uveal tract. The nurse uses nasolacrimal occlusion to prevent the systemic absorption of the ophthalmic medication. He or she applies finger pressure over the lacrimal sac for 1 to 2 minutes after instillation to decrease the risk of absorption and systemic effects. Box 58.1 presents general nursing guidelines for the topical administration of eye medications.
BOX 58.1 General Nursing Guidelines for the Administration of Topical Ophthalmic Medications
 Topical application is the most common route of administration for ophthalmic drugs, and correct administration is essential for optimal therapeutic effects.
Topical application is the most common route of administration for ophthalmic drugs, and correct administration is essential for optimal therapeutic effects.
 Systemic absorption of eye drops can be decreased by closing the eye and applying pressure over the tear duct (nasolacrimal occlusion) for 3 to 5 minutes after instillation.
Systemic absorption of eye drops can be decreased by closing the eye and applying pressure over the tear duct (nasolacrimal occlusion) for 3 to 5 minutes after instillation.
 When multiple eye drops are required, there should be an interval of 5 to 10 minutes between drops because of limited eye capacity and rapid drainage into tear ducts.
When multiple eye drops are required, there should be an interval of 5 to 10 minutes between drops because of limited eye capacity and rapid drainage into tear ducts.
 Absorption of eye medications is increased in eye disorders associated with hyperemia and inflammation.
Absorption of eye medications is increased in eye disorders associated with hyperemia and inflammation.
 Many ophthalmic drugs are available as eye drops (solutions or suspensions) and ointments. Ointments are administered less frequently than drops and often produce higher concentrations of drug in target tissues. However, they also cause blurred vision, which limits their daytime use, at least for ambulatory patients. For some patients, drops may be used during waking hours and ointments at bedtime.
Many ophthalmic drugs are available as eye drops (solutions or suspensions) and ointments. Ointments are administered less frequently than drops and often produce higher concentrations of drug in target tissues. However, they also cause blurred vision, which limits their daytime use, at least for ambulatory patients. For some patients, drops may be used during waking hours and ointments at bedtime.
 Topical ophthalmic medications should not be used after the expiration date; cloudy, discolored solutions should be discarded.
Topical ophthalmic medications should not be used after the expiration date; cloudy, discolored solutions should be discarded.
 Topical eye medications contain a number of inactive ingredients, such as preservatives, buffers, tonicity drugs, antioxidants, and so on. Some contain sulfites, to which some people may have an allergic reaction.
Topical eye medications contain a number of inactive ingredients, such as preservatives, buffers, tonicity drugs, antioxidants, and so on. Some contain sulfites, to which some people may have an allergic reaction.
 Some eye drops contain benzalkonium hydrochloride, a preservative, which is absorbed by soft contact lenses. The medications should not be applied while wearing soft contacts and should be instilled 15 minutes or longer before inserting soft contacts.
Some eye drops contain benzalkonium hydrochloride, a preservative, which is absorbed by soft contact lenses. The medications should not be applied while wearing soft contacts and should be instilled 15 minutes or longer before inserting soft contacts.
 To increase safety and accuracy of ophthalmic drug therapy, the labels and caps of eye medications are color coded.
To increase safety and accuracy of ophthalmic drug therapy, the labels and caps of eye medications are color coded.
Assessing for Therapeutic and Adverse Effects
One hour following administration, the ophthalmologist uses an ophthalmic scope to assess the ability to visualize the inner aspect of the eye. In the treatment of uveitis, the nurse assesses for diminished blurred vision and diminished photophobia.
It is necessary to assess for pain and stinging. In addition, the nurse assesses for blurred vision and sensitivity to light. These effects should diminish and are reversible over time.
Patient Teaching
The nurse instructs patients about the effects of the medication such as photophobia and stinging on administration. It is essential to tell patients not to drive if their vision is impaired. The nurse should tell them to wear sunglasses. Box 58.2 presents additional patient teaching guidelines for ophthalmic medications, including atropine.
BOX 58.2  Patient Teaching Guidelines for Topical Eye Medications
Patient Teaching Guidelines for Topical Eye Medications
General Considerations
 Prevent eye disorders, when possible. For example, try to avoid long periods of reading and computer work; minimize exposure to dust, smog, cigarette smoke, and other eye irritants; and wash hands often and avoid touching the eyes to decrease risk of infection. Use protective eyewear when indicated.
Prevent eye disorders, when possible. For example, try to avoid long periods of reading and computer work; minimize exposure to dust, smog, cigarette smoke, and other eye irritants; and wash hands often and avoid touching the eyes to decrease risk of infection. Use protective eyewear when indicated.
 Do not use nonprescription eye drops (e.g., Murine, Visine) on a regular basis for longer than 48 to 72 hours. Report persistent eye irritation and redness to a health care provider.
Do not use nonprescription eye drops (e.g., Murine, Visine) on a regular basis for longer than 48 to 72 hours. Report persistent eye irritation and redness to a health care provider.
 Have regular eye examinations and testing for glaucoma after 40 years of age.
Have regular eye examinations and testing for glaucoma after 40 years of age.
 Eye-drop preparations often contain sulfites, which can cause allergic reactions in some people.
Eye-drop preparations often contain sulfites, which can cause allergic reactions in some people.
 If you have glaucoma, do not take any drugs without your ophthalmologist’s knowledge and consent. Many drugs given for purposes other than eye disorders may cause or aggravate glaucoma. Also, wear a medical alert bracelet or carry identification that states you have glaucoma. This helps avoid administration of drugs that aggravate glaucoma or to maintain treatment of glaucoma, in emergencies.
If you have glaucoma, do not take any drugs without your ophthalmologist’s knowledge and consent. Many drugs given for purposes other than eye disorders may cause or aggravate glaucoma. Also, wear a medical alert bracelet or carry identification that states you have glaucoma. This helps avoid administration of drugs that aggravate glaucoma or to maintain treatment of glaucoma, in emergencies.
 If you have an eye infection, wash your hands before and after contact with the infected eye to avoid spreading the infection to the unaffected eye or to other people. Also, avoid touching the unaffected eye.
If you have an eye infection, wash your hands before and after contact with the infected eye to avoid spreading the infection to the unaffected eye or to other people. Also, avoid touching the unaffected eye.
 If you wear contact lenses, wash your hands before inserting them and follow instructions for care (e.g., cleaning, inserting, or removing, and duration of wear). Improper or infrequent cleaning may lead to infection. Over wearing is a common cause of corneal abrasions and should be avoided to prevent the development of ulcers.
If you wear contact lenses, wash your hands before inserting them and follow instructions for care (e.g., cleaning, inserting, or removing, and duration of wear). Improper or infrequent cleaning may lead to infection. Over wearing is a common cause of corneal abrasions and should be avoided to prevent the development of ulcers.
 If you wear soft contact lenses, do not use any eye medication without consulting a specialist in eye care. Some eye drops contain benzalkonium hydrochloride, a preservative, which is absorbed by soft contacts. The medication should not be applied while wearing soft contacts and should be instilled 15 minutes or longer before inserting soft contacts.
If you wear soft contact lenses, do not use any eye medication without consulting a specialist in eye care. Some eye drops contain benzalkonium hydrochloride, a preservative, which is absorbed by soft contacts. The medication should not be applied while wearing soft contacts and should be instilled 15 minutes or longer before inserting soft contacts.
 Never use eye medications used by someone else and never allow your eye medications to be used by anyone else. These preparations should be used by one person only, and they are dispensed in small amounts for this purpose. Single-person use minimizes cross-contamination and risks of infection.
Never use eye medications used by someone else and never allow your eye medications to be used by anyone else. These preparations should be used by one person only, and they are dispensed in small amounts for this purpose. Single-person use minimizes cross-contamination and risks of infection.
 Many eye drops and ointments cause temporary blurring of vision. Do not use such medications just before driving or operating potentially hazardous machinery.
Many eye drops and ointments cause temporary blurring of vision. Do not use such medications just before driving or operating potentially hazardous machinery.
 Avoid straining at stool (use laxatives or stool softeners if necessary), heavy lifting, bending over, coughing, and vomiting when possible. These activities increase intraocular pressure, which may cause eye damage in glaucoma and after eye surgery.
Avoid straining at stool (use laxatives or stool softeners if necessary), heavy lifting, bending over, coughing, and vomiting when possible. These activities increase intraocular pressure, which may cause eye damage in glaucoma and after eye surgery.
Self-Administration
 If using more than one eye medication, be sure to administer the correct one at the correct time. Benefits depend on accurate administration.
If using more than one eye medication, be sure to administer the correct one at the correct time. Benefits depend on accurate administration.
 Check expiration dates; do not use any eye medication after the expiration date and do not use any liquid medication that has changed colors or contains particles.
Check expiration dates; do not use any eye medication after the expiration date and do not use any liquid medication that has changed colors or contains particles.
 Shake the container if instructed on the label to do so. Suspensions should be shaken well to ensure the drug is evenly dispersed in the liquid and not settled in the bottom of the container.
Shake the container if instructed on the label to do so. Suspensions should be shaken well to ensure the drug is evenly dispersed in the liquid and not settled in the bottom of the container.
 Wash hands thoroughly.
Wash hands thoroughly.
 Tilt the head back or lie down and look up.
Tilt the head back or lie down and look up.
 Pull the lower lid down to expose the conjunctiva (mucous membrane).
Pull the lower lid down to expose the conjunctiva (mucous membrane).
 Place the dropper directly over the eye. Avoid contact of the dropper with the eye, finger, or any other surface. Such contact contaminates the solution and may cause eye infections and serious damage to the eye, with possible loss of vision.
Place the dropper directly over the eye. Avoid contact of the dropper with the eye, finger, or any other surface. Such contact contaminates the solution and may cause eye infections and serious damage to the eye, with possible loss of vision.
 Look up just before applying a drop; look down for several seconds after applying the drop.
Look up just before applying a drop; look down for several seconds after applying the drop.
 Release the eyelid, close the eyes, and press the inside corner of the eye with a finger for 3 to 5 minutes. Closing the eyes and blocking the tear duct helps the medication be more effective by slowing its drainage out of the eye.
Release the eyelid, close the eyes, and press the inside corner of the eye with a finger for 3 to 5 minutes. Closing the eyes and blocking the tear duct helps the medication be more effective by slowing its drainage out of the eye.
 Do not blink for 30 seconds after the administration of eye medications and during the eye examination.
Do not blink for 30 seconds after the administration of eye medications and during the eye examination.
 Do not rub the eye; do not rinse the dropper.
Do not rub the eye; do not rinse the dropper.
 If more than one eye drop is ordered, wait 10 minutes before instilling the second medication.
If more than one eye drop is ordered, wait 10 minutes before instilling the second medication.
 Use the same basic procedure to insert eye ointments.
Use the same basic procedure to insert eye ointments.
Other Drugs in the Class
Cyclopentolate (Cyclogyl) is useful when given prior to ophthalmic examinations that involve diagnostic testing. It increases the papillary size so the fundus of the eye can be thoroughly examined. Five minutes before the examination, the ophthalmologist or nurse administers the drug (2% solution) to patients who have a heavily pigmented iris. To avoid excessive systemic absorption, it is necessary to use nasolacrimal occlusion during and for 1 to 2 minutes following administration. Patients who have uveitis should receive cyclopentolate in combination with atropine (ophthalmic). Caution is important in the elderly due to increased IOP. Psychotic reactions and behavioral disturbances have occurred in children. It is important to withhold infant feeding for 4 hours after ophthalmic examination due to feeding intolerance.
NCLEX Success
3. A nurse is administering cyclopentolate (Cyclogyl) to a patient with uveitis. What is the most important nursing intervention when administering the medication?
A. Touch the inner canthus of the eye with the medication applicator.
B. Evaluate the redness and inflammation prior to administering the medication.
C. Ask the patient to blink to enhance absorption of the medication.
D. Apply pressure to the lacrimal sac for 2 minutes after medication administration.
4. An elderly patient is receiving cyclopentolate (Cyclogyl) for visualization of the eye. What is the patient at risk for developing?
A. cataracts
B. retinal detachment
C. increased intraocular pressure
D. cerebral edema
ADRENERGIC AGONIST
 Phenylephrine, the prototype ophthalmic adrenergic agonist, is used for its mydriatic effects. Unlike anticholinergic drugs, it does not produce cycloplegic effects.
Phenylephrine, the prototype ophthalmic adrenergic agonist, is used for its mydriatic effects. Unlike anticholinergic drugs, it does not produce cycloplegic effects.
Pharmacokinetics and Action
The mydriatic effects of phenylephrine (ophthalmic) occur 15 to 30 minutes after administration. Peak plasma effects occur in less than 20 minutes, and the duration of action is 1 to 3 hours. Systemic absorption is minimal.
Phenylephrine (ophthalmic) causes contraction of the dilator muscles of the pupil. It produces mydriasis, vasoconstriction, and increased outflow of aqueous humor.
Use
Uses of phenylephrine (ophthalmic) include mydriasis prior to ophthalmic procedures and therapy of wide-angle glaucoma. It can also provide relief of redness with eye irritation. Table 58.2 presents route and dosage information for phenylephrine.
Adverse Effects and Contraindications
With phenylephrine (ophthalmic), systemic adverse effects are rare, but dysrhythmia, hypertension, myocardial infarction, syncope, and subarachnoid bleeding may occur. Ocular effects are reversible and include burning, irritation, visual changes, floaters, and rebound miosis.
Contraindications include hypersensitivity reactions, hypertension, ventricular tachycardia, and narrow-angle glaucoma.
Nursing Implications
Preventing Interactions
Phenylephrine combined with atomoxetine enhances the effects of hypertension and tachycardia. Taking phenylephrine with monoamine oxidase (MAO) inhibitors and sympathomimetic drugs also contributes to the effects of hypertension.
Administering the Medication
Box 58.1 lists general nursing guidelines for the administration of ophthalmic medications. Patients should take phenylephrine for no longer than 72 hours. To administer the ophthalmic solution, the nurse has the patient lie down with the head tilted back. Then he or she takes the following steps:
• Holds the dropper above the eye and drops the medication inside the lower lid, without touching the dropper to the eye
• Has the patient keep the eye open and avoid blinking for 30 seconds
• Applies pressure to the inside corner of the eye for 1 minute
Assessing for Therapeutic and Adverse Effects
The nurse assesses whether the inner aspect of the eye can be visualized 15 minutes after administration.
The nurse measures the blood pressure and the heart rate and checks for hypertension for dysrhythmia. He or she also asks the patient about visual floaters. In addition, it is necessary to assess for burning and irritation of the eye.
Patient Teaching
Box 58.2 presents patient teaching guidelines for topical ophthalmics, including phenylephrine.
NCLEX Success
5. A patient is receiving phenylephrine eye drops for wide-angle glaucoma. What assessment should be made following administration?
A. peripheral edema
B. lung sounds
C. visual changes
D. blood pressure
6. The nurse instructs a patient on the procedure to occlude the tear ducts for 5 minutes after administering eye drops. What is the purpose of this patient teaching?
A. It prevents eye infections.
B. It prevents systemic absorption of the medication.
C. It makes self-administration easier.
D. It allows for the administration of a smaller dose.



