Understand the etiology, pathophysiology, and clinical manifestations of both acute otitis externa and necrotizing otitis externa.
 Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for topical medications used to treat otitis externa.
Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for topical medications used to treat otitis externa.
 Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for systemic medications used to treat necrotizing otitis externa.
Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for systemic medications used to treat necrotizing otitis externa.
 Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for systemic medications used to treat otitis media.
Identify the prototype and describe the action, use, adverse effects, contraindications, and nursing implications for systemic medications used to treat otitis media.
 Identify the adjuvant drugs used to treat otitis externa and otitis media.
Identify the adjuvant drugs used to treat otitis externa and otitis media.
 Implement the nursing process in the care of the patient with otitis externa or otitis media.
Implement the nursing process in the care of the patient with otitis externa or otitis media.
Clinical Application Case Study
Derrick Washington is a member of the high school swim team. He has been swimming two times per day for the past 3 months. The swim team has been very successful this season; it has qualified for the state finals. One morning well before the state meet, Derrick awakens with a severe earache. His mother makes an appointment with a pediatric nurse practitioner, who diagnoses acute otitis externa (swimmer’s ear). The nurse prescribes polymyxin B–neomycin–hydrocortisone suspension (Cortisporin Otic).
KEY TERMS
Otalgia: ear pain
Otic: relating to the ear
Otitis externa: inflammation of the external ear that occurs as a mild allergic dermatitis or as a severe cellulitis
Otitis media: inflammation of the middle ear
Otorrhea: purulent ear drainage
Introduction
This chapter discusses some ear-related disorders and their pharmacological treatment. Infections, whether bacterial or fungal, or allergic reactions, result in ear pain-related inflammation. Otitis externa is a disorder of the external ear that produces inflammation. This condition, most commonly known as swimmer’s ear, is more likely to occur in the summer months. People whose ears are frequently exposed to moisture are more prone to the development of this disorder. Malignant necrotizing otitis externa most commonly affects elderly patients with diabetes mellitus and patients with the human immunodeficiency virus. Otitis media is an acute infection or inflammation of the middle ear. Acute otitis media is the most common ailment for which anti-infective agents are prescribed in children.
The pharmacological therapy of choice for disorders of the ear is otic preparations. These medications, which are discussed elsewhere in this book, have special uses in the treatment of ear conditions.
Overview of Disorders of the Ear
Etiology
Otitis Externa
Causes of otitis externa include moisture in the ear canal, allergic reactions such as psoriasis, or trauma of the ear canal related to itching or scratching. Pseudomonas aeruginosa, Proteus, and Staphylococcus aureus are bacteria that may play a causal role. Aspergillus is the fungus that thrives in the most ear canal.
Otitis Media
Otitis media is more common in children than adults. The causative pathogens include Haemophilus influenzae, Streptococcus pneumoniae, and Moraxella catarrhalis. They enter the middle ear as a result of an alteration in the eustachian tube. This can be caused by upper respiratory congestion, inflammation, or an allergic reaction. Bacteria may enter the middle ear from the contaminated secretions of the nasopharynx or perforation of the tympanic membrane of the middle ear.
Pathophysiology
Otitis Externa
Otitis externa involves the presence of moisture in the external ear canal, leading to the development of inflammation of the pinna and canal. The canal becomes itchy, red, and tender, and increased swelling makes it narrower. Ear pain occurs with movement because of the inflammation. There may be watery or purulent drainage, and intermittent hearing loss may result (Porth & Matfin, 2009).
Necrotizing otitis externa is a soft tissue infection of the external auditory canal. The epidermis becomes thickened and inflamed and the underlying dermis exhibits chronic inflammation. Involvement of the osseous portion of the external auditory canal can lead to temporal bone osteomyelitis. The infection is progressive causing rapid debilitation. If the infection spreads to the base of the skull, it can be fatal.
Otitis Media
In otitis media, infection causes an obstruction of the eustachian tube, resulting in fluid retention and suppuration of retained secretions. This infection is more common in children because the eustachian tube is straighter, allowing the pathogen to enter the ear more easily.
Clinical Manifestations
Otitis Externa
In acute otitis externa, the patient complains of ear pain and discharge from the external auditory canal. The discharge may be yellow or green, possessing a foul odor. The patient may also report a feeling of “fullness” in the ear, decreased hearing, and pruritus.
In necrotizing otitis externa, the presenting symptoms are otalgia, or ear pain, and otorrhea, or purulent drainage. The pain is primarily experienced at night and may extend to the temporomandibular joint when chewing. The advancement of the infection results in osteomyelitis of the skull and temporomandibular joint.
Otitis Media
In acute otitis media, marked fluid and inflammation in the mucosa lining the middle ear space are present (Fig. 59.1). Otalgia and diminished hearing occur. Fever may or may not be present. An upper respiratory tract infection or seasonal allergic rhinitis commonly precedes acute otitis media. Changes in equilibrium may occur. If the tympanic membrane ruptures, patients report a reduction or relief of ear pain.

Figure 59.1 Acute otitis media. (From Weber, J. & Kelly, J. H. (2010). Health assessment in nursing. (4th ed.). Philadelphia, PA: Wolters Kluwer Health | Lippincott Williams & Wilkins.)
Drug Therapy
Table 59.1 lists the various drugs used to treat ear disorders.
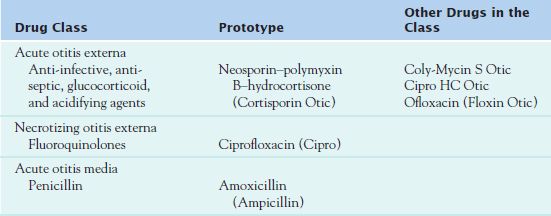
Otitis Externa
For acute otitis externa, use of topical agents, as opposed to systemic agents, is more common. Systemic medications are indicated only if a deep tissue infection develops outside the external canal or if immunocompromised status is an issue. Topical drugs are more effective because they deliver higher concentrations of medication to the infected, inflamed tissue. The use of these agents also reduces adverse effects.
When the infection extends to the pinna, prescribers order oral anti-infective agents. For necrotizing otitis externa, the primary treatment is systemic antipseudomonal antimicrobial agents. Ciprofloxacin is the drug of choice for adults, whereas cephalexin (Keflex) is the preferred drug for children (see Chaps. 16 and 17). The otic solutions most commonly prescribed for acute otitis externa are combination solutions. These medications contain an anti-infective agent, antiseptic, glucocorticoid, and acidifying agent.
Otitis Media
Oral amoxicillin (Amoxil) is the drug of choice for the treatment of acute otitis media (see Table 59.3). Patients who are allergic to penicillins may take cephalosporins.
 TABLE 59.3
TABLE 59.3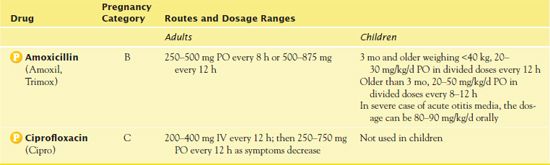
Anti-Infective, Antiseptic, Glucocorticoid, and Acidifying Agents
Health care providers use the combination drug  neomycin–polymyxin B–hydrocortisone (Cortisporin Otic) for the treatment of acute external otitis media. Neomycin and polymyxin B are antibiotics, which combat bacterial infections. Hydrocortisone is a steroid, which reduces the actions of chemicals in the body that cause inflammation, redness, and swelling.
neomycin–polymyxin B–hydrocortisone (Cortisporin Otic) for the treatment of acute external otitis media. Neomycin and polymyxin B are antibiotics, which combat bacterial infections. Hydrocortisone is a steroid, which reduces the actions of chemicals in the body that cause inflammation, redness, and swelling.
Pharmacokinetics
The metabolism and transport effects of polymyxin and neomycin are unknown. Hydrocortisone is metabolized in the liver, and excretion occurs in the urine.
Action
Each component of Cortisporin Otic has its own mechanism of action. Neomycin, an aminoglycoside, inhibits bacterial protein synthesis by irreversibly binding to the 30S ribosome of the susceptible bacteria. Polymyxin B, a miscellaneous anti-infective agent, binds to the lipid phosphates in the bacterial cell membrane, which changes the membrane permeability to prevent leakage of cytoplasm from the bacterial cell wall, contributing to cell death. Hydrocortisone, a steroid, decreases inflammation by stabilizing the leukocyte lysosome membrane, inhibiting phagocytosis and release of allergic substances.
Use
Health care providers use Cortisporin Otic for the treatment of acute otitis externa caused by P. aeruginosa, Proteus, and S. aureus. Table 59.2 presents route and dosage information for Cortisporin Otic.
 TABLE 59.2
TABLE 59.2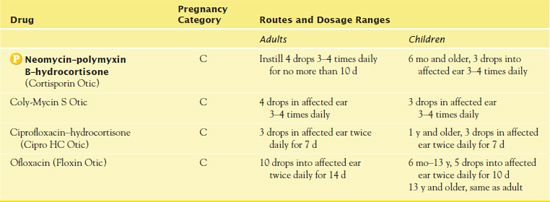
Use in Children
Authorities recommend Cortisporin Otic in children only for bacterial infections of the external auditory canal due to the adverse effect of ototoxicity. The hydrocortisone may cause suppression of the hypothalamic-pituitary-adrenal axis in younger children.
Adverse Effects and Contraindications
Adverse effects of Cortisporin Otic include burning, stinging, and ototoxicity.
Contraindications include a known hypersensitivity to the drug’s components. Prescribers should not order it for viral, fungal, or mycobacterial infections.
Nursing Implications
Preventing Interactions
Cortisporin Otic is associated with no significant drug or herbal interactions.
Pseudomonas aeruginosa Isolated from Otitis Externa Associated with Recreational Waters in some Public Swimming Pools in Tehran
by MOHAMMAD HAJJARTABAR
Iranian Journal of Clinical Infectious Diseases 2010, 5(3), 142-151
Pseudomonas aeruginosa, the most significant bacteria in swimming pools, is the most common bacteria in otitis externa. This study analyzed the bacteriological quality of 11 public outdoor and indoor swimming pools in east and northeast Tehran. It isolated P. aeruginosa from 81.8% of the pools as well as from ear swabs of 79.3% of swimming pool users. The study results revealed that otitis externa was strongly related to the swimming pools contaminated with P. aeruginosa. Based on this study, the public pools in the city enacted strict standards for bathing prior to swimming and policies to prevent overuse of the pools.
IMPLICATIONS FOR NURSING PRACTICE: Although this study is international, it has implications for nursing practice in the United States. Nurses in schools and in the public health sector should ensure the maintenance of strict standards for bathing prior to using public pools; this practice can reduce the rate of otitis externa in the general population. Nurses should be at the forefront of establishment and enforcement of public health initiatives.
Administering the Medication
Administration of Cortisporin Otic is directly in the external ear canal. Prior to administering the otic suspension, it is necessary to shake the medication well. In addition, if cerumen is present, cleaning of the ear canal with a cotton swab is important.
QSEN Safety Alert 
It is necessary to assess the tympanic membrane with an otoscope before inserting Cortisporin Otic. If the tympanic membrane is torn, then the medication is absorbed directly by the inner ear, leading to hearing loss.
The proper administration of ear drops requires tilting the head toward the opposite shoulder, pulling the superior aspect of the auricle upward, and instilling the ear drops into the ear canal. The patient should then lie on the side opposite the side of administration for 20 minutes. To maximize medication absorption, the patient should have a cotton ball placed in the ear canal.
Assessing for Therapeutic and Adverse Effects
The nurse assesses for decreased ear pain and itching as well as for decreased drainage from the ear canal.
It is also necessary to assess for signs of hearing loss due to ototoxicity. He or she also assesses for burning and stinging.
Patient Teaching
Box 59.1 lists patient teaching guidelines for Cortisporin.
BOX 59.1  Patient Teaching Guidelines for Cortisporin Otic
Patient Teaching Guidelines for Cortisporin Otic



