Drug administration
Reviewing the methods
Reviewing the methods
Administration guidelines
Precautions for drug administration
Whenever you administer medication, observe these precautions to ensure that you’re giving the right drug in the right dose to the right patient.
Check the order
Check the order on the patient’s medication record against the physician’s order.
Check the label
Check the label on the medication three times before administering it to a patient to ensure that you’re administering the prescribed medication in the prescribed dose. Check it when you take the container from the shelf or drawer, right before pouring the medication into the medication cup or drawing it into the syringe, and before returning the container to the shelf or drawer. If you’re administering a unitdose medication, check the label for the third time immediately after pouring the medication and again before discarding the wrapper. Don’t open a unit-dose medication until you’re at the patient’s bedside.
Confirm the patient’s identity
Before giving the medication, confirm the patient’s identity by checking two patient identifiers. Then make sure that you have the correct medication.
Explain the procedure to the patient and provide privacy.
Have a written order
Make sure that you have a written order for every medication that’s to be given. If the order is verbal, make sure that the physician signs for it within the time specified by facility policy.
Give labeled medication
Don’t give medication from a poorly labeled or unlabeled container. Furthermore, don’t attempt to label drugs or reinforce drug labels yourself; a pharmacist must do that.
Monitor medication
Never give a medication that someone else has poured or prepared. Never allow your medication cart or tray out of your sight. Never return unwrapped or prepared medications to stock containers. Instead, dispose of them and notify the pharmacy.
Respond to the patient’s questions
If the patient questions you about his medication or the dosage, check his medication record again. If the medication is correct, reassure him that it’s correct. Make sure to tell him about changes in his medication or dosage. Instruct him, as appropriate, about possible adverse reactions and encourage him to report any that he experiences.
Monitor the patient’s response to medication
To assess the patient’s response to medication, be aware of his condition and what the drug’s desired or expected effect should be. For example, if the patient is receiving an antiarrhythmic but continues to have premature ventricular contractions, tell the physician that the drug isn’t having the desired effect. Monitor the patient’s condition carefully; changes such as weight loss or gain can affect the action of some drugs. Other factors, such as the patient’s age, body build, gender, and emotional state, may also affect his
response to drug therapy. Also, check the results of laboratory tests, which can indicate a therapeutic effect, an adverse effect, or a toxic level.
response to drug therapy. Also, check the results of laboratory tests, which can indicate a therapeutic effect, an adverse effect, or a toxic level.
Monitor drug interactions
Because many patients receive more than one drug, it’s important to understand drug interactions. A drug interaction is a change in drug absorption, distribution, metabolism, and excretion that may occur with or shortly after administration of another drug. A desirable interaction is used to help to maintain an effective blood level, or minimize or prevent adverse effects.
Some interactions, however, can have undesirable results, such as weakening a drug’s desired effects or exaggerating its toxic ones. For example, a patient who smokes require larger doses of theophylline than a nonsmoking patient because cigarette smoke activates oxidative enzymes in the liver, increasing drug metabolism.
Watch for adverse effects
When you administer a drug, you must be able to recognize and identify adverse effects and toxic and allergic reactions. Some adverse effects are transient and subside as the patient develops a tolerance for the drug; others may require a change in therapy.
A toxic reaction to a drug can be acute, resulting from an excessive dose (an acetaminophen overdose, for instance), or chronic, resulting from progressive accumulation of the drug in the body. It can also result from impaired metabolism or excretion that results in elevated blood levels of a drug.
A drug allergy (hypersensitivity) results from an antigen-antibody reaction in a susceptible patient. Such a reaction can range from mild urticaria to potentially fatal anaphylaxis. Always check for known drug allergies before administering medications. In some instances, sensitivity tests may be performed before the first dose is given. For some patients, genetic testing for the detection of certain alleles can reveal increased risks for hypersensitivity reactions. Be aware that a negative history doesn’t rule out future allergic reactions. Other undesirable effects to watch for when administering drugs include idiosyncratic reactions and dependence.
Document carefully
Documenting all medications given to a patient provides a legal record of drugs the patient received during his stay in the facility. Medication administration involves documenting on a medication administration record (MAR) as well as in the nurse’s notes. After administering a drug, document on the patient’s Kardex or computer files the drug name, dosage, route and time of administration, and your signature and title. In the nurse’s notes, include any assessment data that refer to the patient’s response to the medication and any adverse effects of the medication.
If your facility documents medications digitally, make sure you enter each drug immediately after you give it. This gives all health care team members access to current medication information and is especially important if the system has no hard-copy backup.
Always write legibly. Use only acceptable abbreviations, and use them correctly. When in doubt as to how to abbreviate a term, spell it out. When documenting parenteral medications, be sure to include the injection site and the route used. After administering the first dose, sign your full name, licensure status, and identifying initials in the appropriate place on the MAR.
Topical administration
Topical drugs
Topical drugs, such as lotions and ointments, are applied directly to the patient’s skin. They’re commonly used for local, rather than systemic, effects. Typically, they must be applied two or three times per day to achieve a full therapeutic effect.
Equipment
Patient’s medication record and chart ♦ prescribed medication ♦ sterile tongue blades ♦ gloves ♦ sterile 4″ × 4″ gauze pads ♦ transparent semipermeable dressing ♦ adhesive tape ♦ solvent (such as cottonseed oil) ♦ optional: cotton-tipped applicators, cotton gloves, or terry cloth scuffs
Implementation
♦ Verify the order on the patient’s medication record by checking it against the physician’s order. Check the patient’s medication record for allergies.
♦ Confirm the patient’s identity using two patient identifiers.
♦ Explain the procedure to the patient because, after discharge, he may have to apply the medication by himself.
♦ Wash your hands to prevent crosscontamination and glove your dominant hand.
♦ Help the patient into a comfortable position and expose the area to be treated. Make sure that the skin or mucous membrane is intact (unless the medication has been ordered to treat a skin lesion). Application of medication to broken or abraded skin may cause unwanted systemic absorption and result in further irritation.
♦ If necessary, clean the skin of debris. You may need to change the glove if it becomes soiled.
To apply a paste, a cream, or an ointment
♦ Open the container. Place the cap upside down to avoid contaminating its inner surface.
♦ Remove a tongue blade from its sterile wrapper and cover one end of it with medication from the tube or jar. Transfer the medication from the tongue blade to your gloved hand.
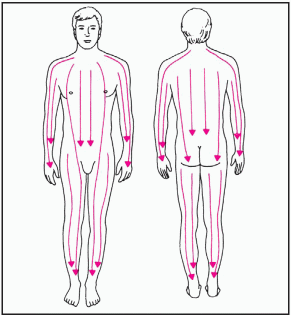
♦ Apply the medication to the affected area with long, smooth strokes that follow the direction of hair growth, as shown below.
|
This technique avoids forcing medication into the hair follicles, which can cause irritation and lead to folliculitis.
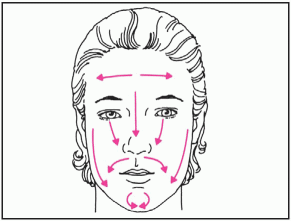
♦ When applying medication to the patient’s face, use a cotton-tipped applicator for small areas such as under the eyes. For larger areas, use a sterile gauze pad and follow the directions shown below.
|
♦ To prevent contamination of the medication, use a new sterile tongue blade each time you remove medication from the container.
To remove an ointment
♦ Wash your hands and put on gloves. Then gently swab ointment from the patient’s skin with a sterile 4″ × 4″ gauze pad saturated with a solvent such as cottonseed oil. Remove remaining oil by wiping the area with a clean sterile gauze pad. Don’t wipe too hard because you could irritate the skin.
To apply other topical medications
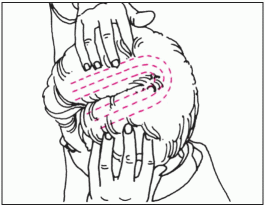
♦ To apply a shampoo, follow package directions. Apply medication with your fingertips, or instruct the patient to do so, as shown below. Massage it into the scalp, if appropriate.
|
♦ To apply topical antifungal creams and nail lacquers, wash the affected area with soap and water. Apply cream and rub it gently into the nail beds. If the patient has athlete’s foot, you can enhance absorption by applying the medication at night and covering the affected area with clean socks. Apply nail lacquers to the entire nail, starting at the nail bed. Allow the lacquer to dry thoroughly, which takes 5 to 10 minutes.
♦ To apply an aerosol spray, shake the container, if indicated, to mix the medication. Hold the container 6″ to 12″ (15 to 30.5 cm) from the skin or follow the manufacturer’s recommendation. Spray the medication evenly over the treatment area to apply a thin film.
♦ To apply a powder, dry the skin surface and apply a thin layer of powder over the treatment area.
♦ To protect applied medications and prevent them from soiling the patient’s clothes, tape a sterile gauze pad or a transparent semipermeable dressing over the treated area. If you’re applying topical medication to his hands, cover them with cotton gloves; if you’re applying medication to his feet, cover them with terry cloth scuffs.
♦ Assess the patient’s skin for signs of irritation, allergic reaction, or breakdown.
Special considerations
♦ To prevent skin irritation from an accumulation of medication, remove residue from previous applications before each new application.
♦ Always wear gloves to prevent your skin from absorbing the medication.
♦ Never apply ointment to the eyelids or ear canal unless ordered. The ointment may congeal and occlude the tear duct or ear canal.
♦ Inspect the treated area frequently for adverse or allergic reactions.
Transdermal medications
Given through an adhesive patch or a measured dose of ointment applied to the skin, transdermal drugs deliver constant, controlled medication directly into the bloodstream for a prolonged systemic effect.
Medications that are available in transdermal form include nitroglycerin, which is used to control angina; scopolamine, which is used to treat
motion sickness; estradiol, which is used for postmenopausal hormone replacement; clonidine, which is used to treat hypertension; nicotine, which is used for smoking cessation; fentanyl, which is used to control chronic pain; and estrogen and progesterone, which are used for hormonal birth control.
motion sickness; estradiol, which is used for postmenopausal hormone replacement; clonidine, which is used to treat hypertension; nicotine, which is used for smoking cessation; fentanyl, which is used to control chronic pain; and estrogen and progesterone, which are used for hormonal birth control.
Nitroglycerin ointment dilates the coronary vessels for 4 hours; a patch can produce the same effect for as long as 24 hours.
The scopolamine patch can relieve motion sickness for as long as 72 hours. Transdermal estradiol and hormonal birth control last for up to 1 week; clonidine and nicotine, 24 hours; and fentanyl, up to 72 hours.
Equipment
Patient’s medication record and chart ♦ gloves ♦ prescribed medication (patch or ointment) ♦ application strip or measuring paper (for nitroglycerin ointment) ♦ adhesive tape ♦ optional: plastic wrap or semipermeable dressing (for nitroglycerin ointment)
Implementation
♦ Verify the order on the patient’s medication record by checking it against the physician’s order. Check the patient’s medication record for allergies.
♦ Confirm the patient’s identity using two patient identifiers.
♦ Wash your hands and put on gloves.
♦ Make sure that previously applied medication has been removed.
♦ Locate a new site for application, different from the previous site.
To apply transdermal ointment
♦ Place the prescribed amount of ointment on the application strip or measuring paper, taking care not to get any on your skin.
♦ Apply the strip to any dry, hairless area of the body. Don’t rub the ointment into the skin.
♦ Tape the application strip and ointment to the skin. If desired, cover the application strip with plastic wrap and tape the wrap in place.
To apply a transdermal patch
♦ Open the package and remove the patch.
♦ Without touching the adhesive surface, remove the clear plastic backing.
♦ Apply the patch to a dry, hairless area—behind the ear, for example, as with scopolamine. Avoid areas that may cause uneven absorption, such as skin folds or scars, or irritated or damaged skin. Don’t apply the patch below the elbow or knee.
After applying transdermal medications
♦ Instruct the patient to keep the area around the patch or ointment as dry as possible.
♦ Wash your hands immediately after applying the patch or ointment.
Special considerations
♦ Apply daily transdermal medications at the same time every day to ensure a continuous effect, but alternate the application sites to avoid skin irritation.
♦ Before applying nitroglycerin ointment, obtain the patient’s baseline blood pressure. Obtain another blood pressure reading 5 minutes after applying the ointment. If the blood pressure has dropped significantly and the patient has a headache, notify the physician immediately. If the blood pressure has dropped but the patient has no symptoms, instruct him to lie still until the blood pressure returns to normal.
♦ Before reapplying nitroglycerin ointment, remove the plastic wrap, the application strip, and any ointment
remaining on the skin at the previous site.
remaining on the skin at the previous site.
♦ When applying a scopolamine patch, instruct the patient not to drive or operate machinery until his response to the drug has been determined.
♦ If the patient is using a clonidine patch, encourage him to check with his physician before using over-the-counter cough preparations. They may counteract the effects of clonidine.
Nitroglycerin ointment
Unlike most topical medications, nitroglycerin ointment is used for its transdermal systemic effect. It’s used to dilate the arteries and veins, thus improving cardiac perfusion in a patient with cardiac ischemia or angina pectoris.
Nitroglycerin ointment is prescribed by the inch and comes with a rectangular piece of ruled paper to be used in applying the medication.
Equipment
Patient’s medication record and chart ♦ ointment ♦ ruled paper ♦ plastic wrap or transparent semipermeable dressing ♦ adhesive tape ♦ sphygmomanometer ♦ optional: gloves
Implementation
♦ Verify the order on the patient’s medication record by checking it against the physician’s order. Check the patient’s medication record for allergies.
♦ Confirm the patient’s identity using two patient identifiers.
♦ Take a patient’s baseline blood pressure for comparison with later readings.
♦ Wash your hands. Then put on gloves if you wish to avoid contact with the medication.
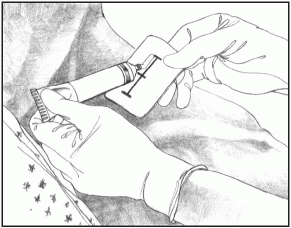
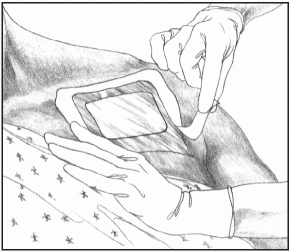
♦ Squeeze the prescribed amount of ointment onto the ruled paper, as shown below.
|
♦ After measuring the correct amount of ointment, tape the paper, with the drug side down, directly to the skin. Some health care facilities require you to use the paper to apply the medication to the patient’s skin, usually on the chest or arm. Spread a thin layer of ointment over a 3″ (7.5-cm) area.
Special considerations
♦ For increased absorption, the physician may request that you cover the site with plastic wrap or transparent semipermeable dressing, as shown below.
|
♦ After 5 minutes, record the patient’s blood pressure. If it has dropped significantly and he has a headache (as a
result of vasodilation of blood vessels in his head), notify the physician.
result of vasodilation of blood vessels in his head), notify the physician.
♦ If the patient’s blood pressure has dropped but he has no adverse reactions, instruct him to lie still until it returns to normal.
Eye medications
Eye medications—drops or ointment —serve diagnostic and therapeutic purposes. During an eye examination, these medications can be used to anesthetize the eye, dilate the pupil, and stain the cornea to identify anomalies. Therapeutic uses include lubrication of the eye and treatment of such conditions as glaucoma and infections.
Equipment and preparation
Patient’s medication record and chart ♦ prescribed eye medication ♦ sterile cotton balls ♦ gloves ♦ warm water or normal saline solution ♦ sterile gauze pads ♦ facial tissue ♦ optional: ocular dressing
Make sure that the medication is labeled for ophthalmic use. Then check the expiration date. Remember to date the container after the first use.
Inspect ocular solutions for cloudiness, discoloration, and precipitation, but remember that some eye medications are suspensions and normally appear cloudy. Don’t use a solution that appears abnormal.
Implementation
♦ Verify the order on the patient’s medication record by checking it against the physician’s order. Check the patient’s medication record for allergies.
♦ Make sure that you know which eye to treat because different medications or doses may be ordered for each eye. Know that “OD” means right eye, “OS” means left eye, and “OU” means both eyes.
♦ Wash your hands and put on gloves.
♦ If the patient has an ocular dressing, remove it by pulling it down and away from his forehead. Avoid contaminating your hands.
♦ To remove exudate or meibomian gland secretions, clean around the eye with sterile cotton balls or sterile gauze pads moistened with warm water or normal saline solution. Have the patient close his eye and then gently wipe the eyelids from the inner to the outer canthus. Use a fresh cotton ball or gauze pad for each stroke.
♦ Have the patient sit or lie in the supine position. Instruct him to tilt his head back and toward his affected eye so that excess medication can flow away from the tear duct, minimizing systemic absorption through the nasal mucosa.
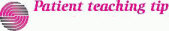
♦ Remove the dropper cap from the medication container and draw the medication into it.
♦ Before instilling eyedrops, instruct the patient to look up and away. This moves the cornea away from the lower lid and minimizes the risk of touching it with the dropper.
To instill eyedrops
♦ Steady the hand that’s holding the dropper by resting it against the patient’s forehead. With your other hand, pull down the lower lid of the affected eye and instill the drops in the conjunctival sac. Never instill eyedrops directly onto the eyeball.
To apply eye ointment
♦ Squeeze a small ribbon of medication on the edge of the conjunctival sac, from the inner to the outer canthus, as shown below. Cut off the ribbon by turning the tube.
|
After instilling eyedrops or applying ointment
♦ Instruct the patient to close his eyes gently, without squeezing the lids shut. If you instilled drops, tell him to blink. If you applied ointment, tell him to roll his eyes behind closed lids to help to distribute the medication over the eyeball.
♦ Use a clean facial tissue to remove excess medication leaking from the eye. Use a fresh tissue for each eye to prevent cross-contamination.
♦ Apply a new ocular dressing, if necessary.
♦ Remove and discard gloves. Then wash your hands.
Special considerations
♦ When administering an eye medication that may be absorbed systemically, press your thumb on the inner canthus for 1 to 2 minutes after instillation, while the patient closes his eyes.
♦ To maintain the sterility of the drug container, never touch the tip of the dropper or bottle to the eye area. Discard any solution that remains in the dropper before returning it to the bottle. If the dropper or bottle tip becomes contaminated, discard it and use another sterile dropper.
Eye medication disks
Small and flexible, an eye medication disk is an oval disk that can release medication (such as pilocarpine) in the eye for up to 1 week. Floating between the eyelids and the sclera, the disk stays in the eye while the patient sleeps and even during swimming and other athletic activities. The disk frees the patient from the need to remember to instill his eye medication. Moisture in the eye or the use of contact lenses doesn’t adversely affect the disk.
Equipment
Patient’s medication record and chart ♦ prescribed eye medication ♦ sterile gloves
Implementation
♦ Verify the order on the patient’s medication record by checking it against the physician’s order. Check the patient’s medication record for allergies.
♦ Confirm the patient’s identity using two patient identifiers.
♦ Make sure that you know which eye to treat because different medications or doses may be ordered for each eye.
To insert an eye medication disk
♦ Wash your hands and put on sterile gloves.
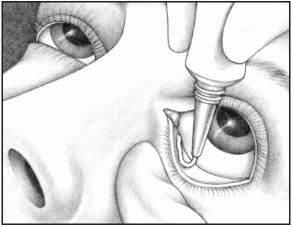
♦ Press your fingertip against the disk so that it sticks lengthwise across your fingertip.
♦ Gently pull the patient’s lower eyelid away from the eye and place the disk in the conjunctival sac. The disk
should lie horizontally, as shown below, not vertically. The disk will adhere to the eye naturally.
should lie horizontally, as shown below, not vertically. The disk will adhere to the eye naturally.
|
♦ Pull the lower eyelid out, up, and over the disk. Tell the patient to blink several times. If the disk is still visible, pull the lower lid out and over the disk again. Tell him that after the disk is in place, he can adjust its position by pressing his finger against his closed lid. Warn him not to rub his eye or move the disk across the cornea.
♦ If the disk falls out, rinse it in cool water and reinsert it. If the disk appears bent, replace it.
♦ If both eyes are being treated with medication disks, replace both disks at the same time.
♦ If the disk slips out of position repeatedly, reinsert it under the upper eyelid. To do this, gently lift and evert the upper eyelid and insert the disk in the conjunctival sac. Gently pull the lid back into position and tell the patient to blink several times. The more he uses the disk, the easier it should be for him to retain it. If not, notify the physician.
To remove an eye medication disk
♦ To remove the disk with one finger, put on sterile gloves and evert the lower eyelid to expose the disk. Use the forefinger of your other hand to slide the disk into the lid and out of the patient’s eye. To use two fingers, evert the lower lid with one hand to expose the disk. Then pinch it with the thumb and forefinger of your other hand and remove it.
♦ If the disk is located in the upper eyelid, apply long, circular strokes to the closed eyelid with your finger until you can see the disk in the corner of the eye. Then place your finger directly on the disk, move it to the lower sclera, and remove it as you would a disk located in the lower lid.
Special considerations
♦ If the patient will continue therapy with an eye medication disk after discharge, teach him to insert and remove it himself. Ask him to demonstrate the techniques for you.
♦ Explain that mild reactions are common, but should subside within the first 6 weeks of use. Foreign-body sensation in the eye, mild tearing, redness of the eye or eyelid, increased mucus discharge, and itchiness can occur. Blurred vision, stinging, swelling, and headaches can occur with pilocarpine, specifically. Tell the patient to report persistent or severe signs or symptoms.
Eardrops
Eardrops may be instilled to treat infection or inflammation, to soften cerumen for later removal, to produce local anesthesia, or to facilitate the removal of an insect trapped in the ear.
Equipment and preparation
Patient’s medication record and chart ♦ prescribed eardrops ♦ light source ♦ facial tissue or cotton-tipped applicator ♦ optional: cotton ball, bowl of warm water
Warm the medication to body temperature in the bowl of warm water or carry it in your pocket for 30 minutes before administration. If necessary, test the temperature by placing a drop on your wrist. (If the medication is too
hot, it may burn the patient’s eardrum.) To avoid injuring the ear canal, check the dropper before use to make sure that it isn’t chipped or cracked.
hot, it may burn the patient’s eardrum.) To avoid injuring the ear canal, check the dropper before use to make sure that it isn’t chipped or cracked.
Implementation
♦ Verify the order on the patient’s medication record by checking it against the physician’s order. Check the patient’s medication record for allergies.
♦ Wash your hands.
♦ Confirm the patient’s identity using two patient identifiers.
♦ Have the patient lie on the side opposite the affected ear.
♦ Straighten the patient’s ear canal. For an adult, pull the auricle up and back.
 For an infant or a child younger than age 3, gently pull the auricle down and back— the ear canal is straighter at this age.
For an infant or a child younger than age 3, gently pull the auricle down and back— the ear canal is straighter at this age.Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access