ECGs
Interpreting them with ease and accuracy
Interpreting them with ease and accuracy
Normal ECG
Analyzing the ECG waveform
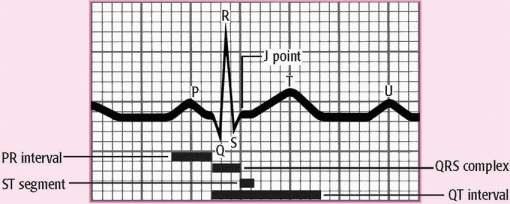
An electrocardiogram (ECG) complex represents the electrical events occurring in one cardiac cycle. A complex consists of five waveforms labeled with the letters P, Q, R, S, and T. The letters Q, R, and S are referred to as a unit known as the QRS complex. The ECG tracing represents the conduction of electrical impulses from the atria to the ventricles. (See Components of an ECG waveform.)
♦ The P wave is the first component of the normal ECG waveform. It represents atrial depolarization.
♦ The PR interval tracks the atrial impulse from the atria through the atrioventricular (AV) node, the bundle of His, and the right and left bundle branches. It begins with atrial depolarization and ends with the beginning of ventricular depolarization.
♦ The QRS complex follows the P wave and represents ventricular depolarization.
♦ The ST segment represents the end of ventricular depolarization and the beginning of ventricular repolarization. The J point marks the end of the QRS complex and the beginning of the ST segment.
♦ The T wave represents ventricular repolarization.
♦ The QT interval measures the time needed for ventricular depolarization and repolarization.
♦ The U wave represents His-Purkinje repolarization.
How to read an ECG rhythm strip: The 8-step method
Analyzing a rhythm strip is a skill that’s developed through practice. You can use several methods, as long as you’re consistent. (See The 8-step method of rhythm strip analysis, pages 105 and 106.)
The 8-step method of rhythm strip analysis
Rhythm strip analysis requires a sequential and systematic approach. The following eight steps provide a good outline for you to follow.
Step 1: Determine rhythm
To determine the heart’s atrial and ventricular rhythms, use either the pen-andpencil method or the caliper method.
To determine the atrial rhythm, measure the P-P intervals, the intervals between consecutive P waves. These intervals should occur regularly, with only small variations associated with respirations. Then compare the P-P intervals in several cycles. Consistently similar P-P intervals indicate regular atrial rhythm; dissimilar P-P intervals indicate irregular atrial rhythm.
To determine the ventricular rhythm, measure the intervals between two consecutive R waves in the QRS complexes. If an R wave isn’t present, use either Q waves or S waves of consecutive QRS complexes. The R-R intervals should occur regularly. Then compare the R-R intervals in several cycles. As with atrial rhythms, consistently similar intervals mean a regular rhythm; dissimilar intervals point to an irregular rhythm.
After completing your measurements, ask yourself:
♦ Is the rhythm regular or irregular? Consider a rhythm with only slight variations (up to 0.04 second) to be regular.
♦ If the rhythm is irregular, is it slightly irregular or markedly irregular? Does the irregularity occur in a pattern (a regularly irregular pattern)?
Step 2: Calculate rate
You can use one of three methods to determine the atrial and ventricular heart rates from an ECG waveform. Although these methods can provide accurate information, you shouldn’t rely solely on them when assessing your patient. Keep in mind that the ECG waveform represents electrical, not mechanical, activity. Therefore, although an ECG can show that ventricular depolarization has occurred, it doesn’t mean that ventricular contraction has occurred. To determine this, you must assess the patient’s pulse.
♦ Times-ten method. The simplest, quickest, and most common way to calculate rate is the times-ten method, especially if the rhythm is irregular. ECG paper is marked in increments of 3 seconds, or 15 large boxes. To calculate the atrial rate, obtain a 6-second strip, count the number of P waves that appear on it, and multiply this number by 10. Ten 6-second strips equal 1 minute. Calculate the ventricular rate the same way, using the R waves.
♦ 1,500 method. If the heart rhythm is regular, use the 1,500 method, so named because 1,500 small squares equal 1 minute. Count the number of small squares between identical points on two consecutive P waves, and then divide 1,500 by that number to determine the atrial rate. To obtain the ventricular rate, use the same method with two consecutive R waves.
♦ Sequence method. The third method of estimating heart rate is the sequence method, which requires memorizing a sequence of numbers. For the atrial rate, find a P wave that peaks on a heavy black line, and assign the following numbers to the next six heavy black lines: 300, 150, 100, 75, 60, and 50. Then find the next P-wave peak and estimate the atrial rate, based on the number assigned to the nearest heavy black line. Estimate the ventricular rate the same way, using the R wave.
Step 3: Evaluate P waves
When examining a rhythm strip for P waves, ask yourself:
♦ Are P waves present?
♦ Do the P waves have a normal configuration?
♦ Do all of the P waves have a similar size and shape?
♦ Is there one P wave for every QRS complex?
Step 4: Determine PR interval duration
To measure the PR interval, count the small squares between the start of the P wave and the start of the QRS complex; then multiply the number of squares by 0.04 second. After you perform this calculation, ask yourself:
♦ Does the duration of the PR interval fall within normal limits, 0.12 to 0.20 second (or 3 to 5 small squares)?
♦ Is the PR interval constant?
Step 5: Determine QRS complex duration
When determining QRS complex duration, make sure to measure straight across from the end of the PR interval to the end of the S wave, not just to the peak. Remember, the QRS complex has no horizontal components. To calculate duration, count the number of small squares between the beginning and the end of the QRS complex and multiply this number by 0.04 second. Then ask yourself the following questions:
♦ Does the duration of the QRS complex fall within normal limits, 0.06 to 0.10 second?
♦ Are all QRS complexes the same size and shape? (If not, measure each one and describe them individually.)
♦ Does a QRS complex appear after every P wave?
Step 6: Evaluate T wave
Examine the T waves on the ECG strip. Then ask yourself:
♦ Are T waves present?
♦ Do all of the T waves have a normal shape?
♦ Could a P wave be hidden in a T wave? ♦ Do all of the T waves have a normal amplitude?
♦ Do the T waves have the same deflection as the QRS complexes?
Step 7: Determine QT interval duration
Count the number of small squares between the beginning of the QRS complex and the end of the T wave, where the T wave returns to the baseline. Multiply this number by 0.04 second. Ask yourself:
♦ Does the duration of the QT interval fall within normal limits, 0.36 to 0.44 second?
Step 8: Evaluate other components
Note the presence of ectopic or aberrantly conducted beats or other abnormalities. Also, check the ST segment for abnormalities and look for the presence of a U wave.
Next, interpret your findings by classifying the rhythm strip according to one or all of the following features:
♦ Site of origin of the rhythm. For example, sinus node, atria, atrioventricular node, or ventricles.
♦ Rate. Normal (60 to 100 beats/minute), bradycardia (less than 60 beats/minute), or tachycardia (greater than 100 beats/minute).
♦ Rhythm. Normal or abnormal; for example, flutter, fibrillation, heart block, escape rhythm, or other arrhythmias.
Normal sinus rhythm
When the heart functions normally, the sinoatrial (SA) node acts as the primary pacemaker, initiating the electrical impulses. The SA node assumes this role because its automatic firing rate exceeds that of the heart’s other pacemakers, allowing cells to depolarize spontaneously.
Normal sinus rhythm records an impulse that starts with the sinus node and progresses to the ventricles through a normal conduction pathway—from the sinus node to the atria and AV node, through the bundle of His, to the bundle branches, and onto the Purkinje fibers. Normal sinus rhythm is the standard against which all other rhythms are compared; you must be able to recognize normal sinus rhythm before you can recognize an arrhythmia.
Based on the location of the electrical disturbance, arrhythmias can be classified as sinus, atrial, junctional, or ventricular arrhythmias, or as AV blocks. Functional disturbances in the SA node produce sinus arrhythmias. Enhanced automaticity of atrial tissue or reentry may produce atrial arrhythmias, the most common arrhythmias.
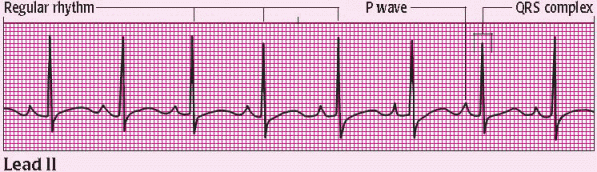
Characteristics of normal sinus rhythm
|
Atrial rhythm: regular
Ventricular rhythm: regular
Atrial rate: 60 to 100 beats/minute (80 beats/minute shown)
Ventricular rate: 60 to 100 beats/minute (80 beats/minute shown)
P wave: normally shaped (All P waves have similar size and shape; a P wave precedes each QRS complex.)
PR interval: within normal limits (0.12 to 0.20 second) and constant (0.20-second duration shown)
QRS complex: within normal limits (0.06 to 0.10 second) (All QRS complexes have the same configuration. The duration shown here is 0.12 second.)
T wave: normally shaped; upright and rounded in lead II (Each QRS complex is followed by a T wave.)
QT interval: within normal limits (0.36 to 0.44 second) and constant (0.44-second duration shown)
Junctional arrhythmias originate in the area around the AV node and bundle of His. These arrhythmias usually result from a suppressed higher pacemaker or from blocked impulses at the AV node.
Ventricular arrhythmias originate in ventricular tissue below the bifurcation of the bundle of His. These rhythms may result from reentry or enhanced automaticity or may occur after depolarization.
An AV block results from an abnormal interruption or delay of atrial impulse conduction to the ventricles. It may be partial or total and may occur in the AV node, bundle of His, or Purkinje system.
Arrhythmias
Sinus arrhythmia
In sinus arrhythmia, the heart rate stays within normal limits, but the rhythm is irregular and corresponds to the respiratory cycle and to variations in vagal tone. During inspiration, an increased volume of blood returns to the heart, reducing vagal tone and increasing sinus rate. During expiration, venous return decreases, vagal tone increases, and sinus rate slows.
Conditions unrelated to respiration may also produce sinus arrhythmia. These conditions include inferior wall myocardial infarction (MI) and digoxin toxicity.
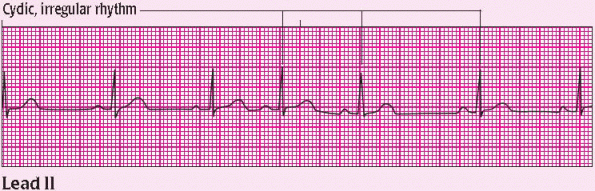
Characteristics of sinus arrhythmia
|
Atrial rhythm: irregular, corresponding to the respiratory cycle
Ventricular rhythm: irregular, corresponding to the respiratory cycle
Atrial rate: within normal limits; varies with respiration (60 beats/minute shown)
Ventricular rate: within normal limits; varies with respiration (60 beats/ minute shown)
P wave: normal size and configuration (One P wave precedes each QRS complex.)
PR interval: within normal limits (0.16-second, constant interval shown)
QRS complex: normal duration and configuration (0.06-second duration shown)
T wave: normal size and configuration
QT interval: within normal limits (0.36-second interval shown)
Other: phasic slowing and quickening of the rhythm
Sinus arrhythmia is easily recognized in elderly, pediatric, and sedated patients. The patient’s pulse rate increases with inspiration and decreases with expiration. Usually, the patient is asymptomatic.
Intervention
Treatment isn’t necessary unless the patient is symptomatic or the sinus arrhythmia stems from an underlying cause. If symptoms are associated with symptomatic bradycardia, atropine may be administered.
Sinus bradycardia
Characterized by a sinus rate of less than 60 beats/minute, sinus bradycardia usually occurs as the normal response to a reduced demand for blood flow. It’s common among athletes, whose well-conditioned hearts can maintain stroke volume with reduced effort. It may also be caused by drugs, such as cardiac glycosides, calcium channel blockers, and beta-adrenergic blockers. Sinus bradycardia may occur after an inferior wall MI involving the right coronary artery, which supplies the blood to the SA node. This rhythm may develop during sleep and in patients with increased intracranial pressure. It may also result from vagal stimulation caused by vomiting or defecating. Pathologic sinus bradycardia may occur with sick sinus syndrome.
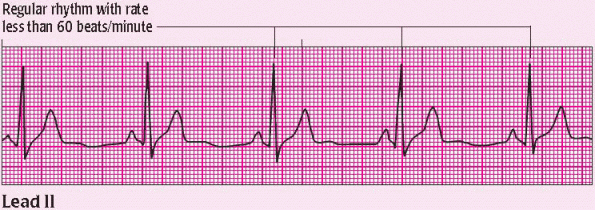
Characteristics of sinus bradycardia
|
Atrial rhythm: regular
Ventricular rhythm: regular
Atrial rate: less than 60 beats/minute (50 beats/minute shown)
Ventricular rate: less than 60 beats/minute (50 beats/minute shown)
P wave: normal size and configuration (One P wave precedes each QRS complex.)
PR interval: within normal limits and constant (0.14-second duration shown)
QRS complex: normal duration and configuration (0.08-second duration shown)
T wave: normal size and configuration
QT interval: within normal limits (0.40-second interval shown)
The patient with sinus bradycardia is asymptomatic if he can compensate for the decrease in heart rate by increasing stroke volume. If he cannot, he may have signs and symptoms of decreased cardiac output, such as hypotension, syncope, confusion, and blurred vision.
Intervention
If the patient is asymptomatic, treatment isn’t necessary. If he has signs and symptoms, the goal of treatment is to identify and correct the underlying cause. The heart rate may be increased with drugs such as atropine. A temporary (transcutaneous or transvenous) or permanent pacemaker may be necessary if bradycardia persists.
Sinus tachycardia
Sinus tachycardia is an acceleration of firing of the SA node beyond its normal discharge rate. In an adult, it’s characterized by a sinus rate of more than 100 beats/minute. The rate rarely exceeds 180 beats/minute except during strenuous exercise. The maximum rate achieved with exercise decreases with age.
A normal response to cellular demands for increased oxygen delivery and blood flow commonly produces sinus tachycardia. Conditions that cause such a demand include heart failure, shock, anemia, exercise, fever, hypoxia, pain, and stress. Drugs that stimulate the beta receptors in the heart also cause sinus tachycardia. They include aminophylline, epinephrine, dobutamine, and dopamine. Alcohol, caffeine, and nicotine may also produce sinus tachycardia.
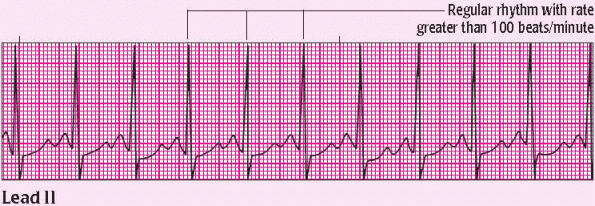
Characteristics of sinus tachycardia
|
Atrial rhythm: regular
Ventricular rhythm: regular
Atrial rate: 100 to 160 beats/minute (110 beats/minute shown)
Ventricular rate: 100 to 160 beats/minute (110 beats/minute shown)
P wave: normal size and configuration (One P wave precedes each QRS complex. As the sinus rate reaches about 150 beats/minute, the P wave merges with the preceding T wave and may be difficult to identify. Examine the descending slope of the preceding T wave closely for notches, indicating presence of the P wave. The P wave shown is normal.)
PR interval: within normal limits and constant (0.16-second duration shown)
QRS complex: normal duration and configuration (0.10-second duration shown)
T wave: normal size and configuration
QT interval: within normal limits and constant (0.36-second duration shown)
Other: gradual onset and cessation
An elevated heart rate increases myocardial oxygen demands. If the patient can’t meet these demands (for example, because of coronary artery disease), ischemia and further myocardial damage may occur.
Intervention
Treatment focuses on finding the primary cause. If it’s high catecholamine levels, a beta-adrenergic blocker may slow the heart rate. After MI, persistent sinus tachycardia may precede heart failure or cardiogenic shock.
Sinus arrest
In sinus arrest, the normal sinus rhythm is interrupted by an occasional, prolonged failure of the SA node to initiate an impulse. Therefore, sinus arrest is caused by episodes of failure in the automaticity of impulse formation of the SA node. The atria aren’t stimulated, and an entire PQRST complex is missing from the ECG strip. Except for the missing complex, or pause, the ECG usually remains normal.
During a sinus arrest, the sinus node resets itself so that when the impulse is initiated, the complex that occurs after the pause will be out of the cycle and the rate will usually be different from the rate before the pause.
Sinus arrest may result from an acute inferior wall MI, increased vagal tone, or the use of certain drugs, such as cardiac glycosides, calcium channel blockers, and beta-adrenergic blockers. The arrhythmia may also be linked to sick sinus syndrome. The patient has an irregular pulse rate associated with the pauses in sinus rhythm. If the pauses are infrequent, the patient is asymptomatic. If they occur frequently and last for several seconds, however, the patient may have signs of decreased cardiac output.
Characteristics of sinus arrest
|
Atrial rhythm: regular, except for the missing PQRST complexes
Ventricular rhythm: regular, except for the missing complex
Atrial rate: within normal limits but varies because of pauses (94 beats/minute shown)
Ventricular rate: within normal limits but varies because of pauses (94 beats/minute shown)
P wave: normal size and configuration (One P wave precedes each QRS complex but is absent during a pause.)
PR interval: within normal limits and constant when the P wave is present; not measurable when the P wave is absent (0.20-second duration shown on all complexes surrounding the arrest)
QRS complex: normal duration and configuration; absent during pause (0.08-second duration shown)
T wave: normal size and configuration; absent during pause
QT interval: within normal limits; not measurable during pause (0.40-second, constant interval shown)
Intervention
For a symptomatic patient, treatment focuses on maintaining cardiac output and discovering the cause of sinus arrest. If indicated, atropine may be given or a temporary (transcutaneous or transvenous) or permanent pacemaker may be inserted.
Premature atrial contractions
Premature atrial contractions (PACs) usually result from an irritable focus in the atrium that supersedes the SA node as the pacemaker for one or more beats.
Although PACs commonly occur in normal hearts, they’re also associated with coronary and valvular heart disease. In an inferior wall MI, PACs may indicate a concomitant right atrial infarct. In an anterior wall MI, PACs are an early sign of left-sided heart failure. They may also warn of more severe atrial arrhythmia, such as atrial flutter or atrial fibrillation.
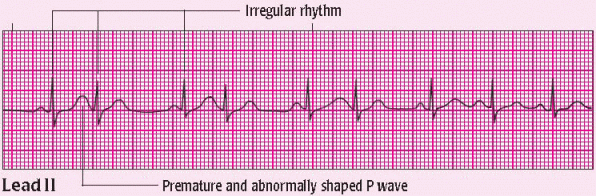
Characteristics of premature atrial contractions
|
Atrial rhythm: irregular (Incomplete compensatory pause follows premature arterial contraction [PAC]. Underlying rhythm may be regular.)
Ventricular rhythm: irregular (Incomplete compensatory pause follows PAC. Underlying rhythm may be regular.)
Atrial rate: varies with underlying rhythm (90 beats/minute shown)
Ventricular rate: varies with underlying rhythm (90 beats/minute shown)
P wave: premature and abnormally shaped; possibly lost in previous T wave (Varying configurations indicate multiform PACs.)
PR interval: usually normal but may be shortened or slightly prolonged, depending on the origin of ectopic focus (0.16-second, constant interval shown)
QRS complex: usually normal duration and configuration (0.08-second, constant duration shown)
T wave: usually normal configuration; may be distorted if the P wave is hidden in the previous T wave
QT interval: usually normal (0.36-second, constant interval shown)
Other: may occur in bigeminy or couplets
Possible causes include digoxin toxicity, hyperthyroidism, elevated catecholamine levels, acute respiratory failure, and chronic obstructive pulmonary disease. Alcohol, caffeine, or tobacco use can also trigger PACs. Patients who eliminate or control these factors can usually correct the arrhythmia.
Intervention
Symptomatic patients may be treated with beta-adrenergic blockers or calcium channel blockers.
Atrial tachycardia
Atrial tachycardia is a supraventricular tachycardia, which means that the impulse originates above the ventricles. In this rhythm, the impulse originates in the atria. The rapid atrial rate shortens diastole, resulting in a loss of atrial kick, reduced cardiac output, reduced coronary perfusion, and ischemic myocardial changes.
Although atrial tachycardia can occur in healthy patients, it’s usually associated with high catecholamine levels, digoxin toxicity, MI, cardiomyopathy, hyperthyroidism, hypertension, and valvular heart disease. Three types of atrial tachycardia exist: atrial tachycardia with block, multifocal atrial tachycardia, and paroxysmal atrial tachycardia.
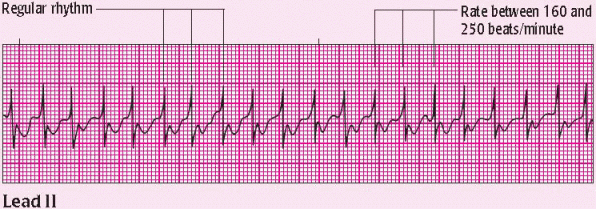
Characteristics of atrial tachycardia
|
Atrial rhythm: regular
Ventricular rhythm: regular
Atrial rate: three or more successive ectopic atrial beats at a rate of 160 to 250 beats/minute (210 beats/minute shown)
Ventricular rate: varies with atrioventricular conduction ratio (210 beats/minute shown)
P wave: 1:1 ratio with QRS complex, although commonly indiscernible because of rapid rate; may be hidden in previous ST segment or T wave
PR interval: may not be measurable if P wave can’t be distinguished from preceding T wave (If P wave is present, PR interval is short when conduction through the AV node is 1:1. On this strip, the PR interval isn’t discernible.)
QRS complex: usually normal unless aberrant intraventricular conduction is present (0.10-second duration shown)
T wave: may be normal or inverted if ischemia is present (inverted T waves shown)
QT interval: usually normal but may be shorter because of rapid rate (0.20-second interval shown)
Other: appearance of ST-segment and Twave changes if tachyarrhythmia persists longer than 30 minutes
Intervention
If the patient has atrial tachycardia or paroxysmal atrial tachycardia and is symptomatic, prepare for immediate cardioversion. If the patient is stable, the physician may perform carotid sinus massage (if no bruits are present) or order drug therapy, such as adenosine (Adenocard), a calcium channel blocker, a beta-adrenergic blocker, or digoxin (Lanoxin). If these treatments are ineffective in rhythm conversion, then procainamide or amiodarone may be needed. If these measures fail, cardioversion may be necessary.
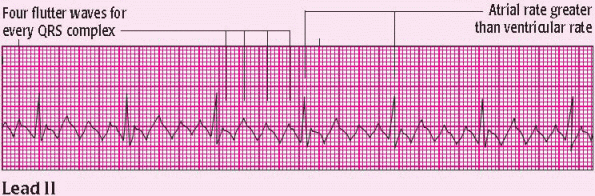
Atrial flutter
Characterized by an atrial rate of 250 beats/minute or more, atrial flutter is caused by multiple reentry circuits within the atrial tissue. On the ECG, the P waves lose their normal appearance as a result of rapid atrial rate and blend together in a sawtooth configuration known as flutter waves. These waves are the hallmark of atrial flutter.
Causes of atrial flutter include conditions that enlarge atrial tissue and elevate atrial pressures. Atrial flutter is associated with MI, increased catecholamine levels, hyperthyroidism, and digoxin toxicity.
If the patient’s pulse rate is normal, he usually has no symptoms. If his pulse rate is high, however, he’ll probably have signs and symptoms of decreased cardiac output, such as hypotension and syncope.
Characteristics of atrial flutter
|
Atrial rhythm: regular
Ventricular rhythm: may be regular or irregular, depending on the conduction ratio (regular rhythm shown)
Atrial rate: 300 to 350 beats/minute (300 beats/minute shown)
Ventricular rate: variable (70 beats/minute shown)
P wave: atrial activity seen as flutter waves, with a classic sawtooth appearance
PR interval: not measurable
QRS complex: usually normal but can be distorted by the underlying flutter waves (0.10-second, normal duration shown)
T wave: unidentifiable
QT interval: not measurable
Intervention
If the patient is symptomatic, prepare for immediate cardioversion. The focus of treatment for stable patients with atrial flutter includes controlling the rate and converting the rhythm. Specific interventions depend on the patient’s cardiac function, the presence of preexcitation syndromes, and the duration (less than or greater than 48 hours) of arrhythmia. For example, in patients with atrial flutter, normal cardiac function, and duration of rhythm less than 48 hours, cardioversion may be considered. When duration is greater than 48 hours, avoid nonemergent cardioversion unless adequate anticoagulation has been achieved.
Drugs that may be ordered to control atrial rate include amiodarone, ibutilide, procainamide, calcium channel blockers, and beta-adrenergic blockers.
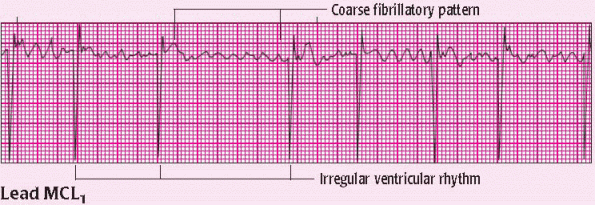
Atrial fibrillation
Atrial fibrillation is chaotic, asynchronous electrical activity in the atrial tissue. It results from impulses in many reentry pathways. These multiple and multidirectional impulses cause the atria to quiver instead of contracting regularly.
With this type of arrhythmia, blood may pool in the left atrial appendage and form thrombi that can be ejected into the systemic circulation. An associated rapid ventricular rate can decrease cardiac output.
Possible causes include valvular disorders, hypertension, coronary artery disease, MI, chronic lung disease, ischemia, thyroid disorders, and Wolff-Parkinson-White syndrome. The disorder may also result from high adrenergic tone as a result of physical exertion, sepsis, alcohol withdrawal, or the use of drugs, such as aminophylline (theophylline ethylenediamine) and cardiac glycosides.
Characteristics of atrial fibrillation
|
Atrial rhythm: grossly irregular
Ventricular rhythm: grossly irregular
Atrial rate: greater than 400 beats/minute
Ventricular rate: varies from 40 to 250 beats/minute (80 beats/minute shown)
P wave: absent; appearance of erratic baseline fibrillatory waves (f waves) (When the f waves are pronounced, the arrhythmia is called coarse atrial fibrillation. When the f waves aren’t pronounced, the arrhythmia is known as fine atrial fibrillation. On this strip, the f waves are pronounced.)
PR interval: indiscernible
QRS complex: duration usually within normal limits, with aberrant intraventricular conduction (0.08-second duration shown)
T wave: indiscernible
QT interval: not measurable
Intervention
If the patient is symptomatic, synchronized cardioversion should be used immediately. Vagal stimulation may be used to slow the ventricular response, but it won’t convert the arrhythmia. Drugs that may be ordered to slow AV conduction include calcium channel blockers and beta-adrenergic blockers. Digoxin may be ordered if the patient is stable. After the rate slows, if conversion to a normal sinus rhythm hasn’t occurred, amiodarone (Cordarone), flecainide, or sotalol may be ordered. If atrial fibrillation is of several days’ duration, anticoagulant therapy is recommended before pharmacologic or electrical conversion. If atrial fibrillation is of recent onset, ibutilide (Corvert) may be used to convert the rhythm.
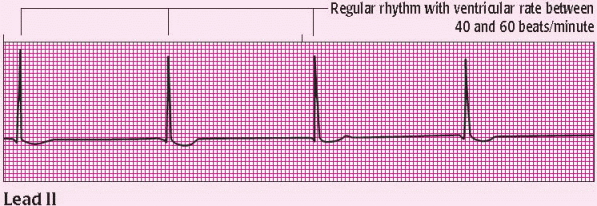
Junctional rhythm
Junctional rhythm, also known as junctional escape rhythm, occurs in the AV junctional tissue. It causes retrograde depolarization of the atrial tissue and antegrade depolarization of the ventricular tissue. It results from conditions that depress SA node function, such as an inferior wall MI, digoxin toxicity, and vagal stimulation. The arrhythmia may also stem from increased automaticity of the junctional tissue, which can be caused by digoxin toxicity or ischemia associated with an inferior wall MI.
Junctional rhythm is a regular rhythm with a ventricular rate of 40 to 60 beats/minute. A junctional rhythm with a ventricular rate of 60 to 100 beats/minute is known as an accelerated junctional rhythm. If the ventricular rate exceeds 100 beats/minute, the arrhythmia is called junctional tachycardia.
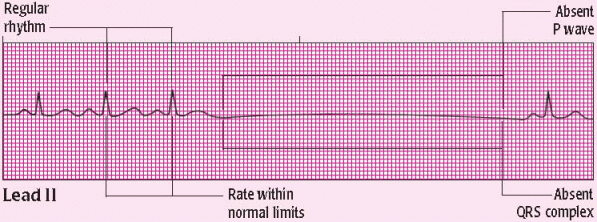
Characteristics of junctional rhythm
|
Atrial rhythm: regular
Ventricular rhythm: regular
Atrial rate: if discernible, 40 to 60 beats/minute (On this strip, the rate isn’t discernible.)
Ventricular rate: 40 to 60 beats/minute (40 beats/minute shown)
P wave: usually inverted; may precede, follow, or fall within the QRS complex; may be absent (On this strip, the P wave is absent.)
PR interval: less than 0.12 second and constant if the P wave precedes the QRS complex; otherwise, not measurable (not measurable on this strip)
QRS complex: duration normal; configuration usually normal (0.08-second duration shown)
T wave: usually normal configuration
QT interval: usually normal (0.32-second duration shown)
Intervention
Treatment aims to identify and manage the primary cause of arrhythmia. If the patient is symptomatic, treatment may include atropine to increase the sinus or junctional rate. Alternately, the physician may insert a pacemaker or use transcutaneous pacing to maintain an effective heart rate.
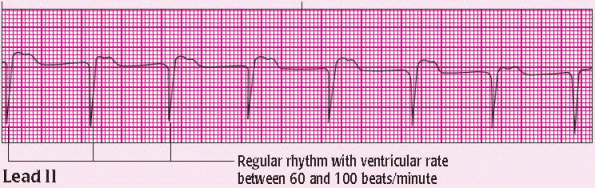
Accelerated junctional rhythm
An accelerated junctional rhythm is an arrhythmia that originates in the AV junction and is usually caused by enhanced automaticity of the AV junctional tissue. It’s called “accelerated” because it occurs at a rate of 60 to 100 beats/minute, exceeding the inherent junctional rate of 40 to 60 beats/minute.
Digoxin toxicity is a common cause of accelerated junctional rhythm. Other causes include electrolyte disturbances, ventricular heart disease, heart failure, and inferior or posterior MI.
Characteristics of accelerated junctional rhythm
|
Atrial rhythm: regular
Ventricular rhythm: regular
Atrial rate: if discernible, 60 to 100 beats/minute (On this strip, the rate isn’t discernible.)
Ventricular rate: 60 to 100 beats/minute (75 beats/minute shown)
P wave: usually inverted; may precede, follow, or fall within the QRS complex; may be absent (On this strip, the P wave is absent.)
PR interval: less than 0.12 second and constant if the P wave precedes the QRS complex; otherwise, not measurable (not measurable on this strip)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access