Documentation systems
Completing forms fully and concisely
Completing forms fully and concisely
Documentation refers to the preparation and maintenance of records that describe a patient’s care. If you document with attention to detail, you’ll clearly show the quality of care your patient received, the outcome of that care, and the treatment he still needs.
The detailed information you assemble will be scrutinized by many reviewers, including other health care team members; accrediting, certifying, and licensing organizations; performance improvement monitors; peer reviewers; and Medicare and insurance company reviewers. Attorneys and judges may also examine your documentation. Researchers and educators may use it to improve patient care and to provide continuing education.
Although each health care facility determines its own requirements for documentation and evaluation, those requirements must comply with legal, accreditation, and professional standards.
Similarly, a nursing department can select the documentation system it wants to use as long as the system demonstrates adherence to standards and care requirements. Regardless of the documentation system used, specific policies and procedures for documentation must be in place and known. Understanding them will help you document care accurately. It will also serve you well when evaluating or modifying your documentation system or when selecting a new one.
Depending on the policies of your health care facility, you’ll use one or more documentation systems to record your nursing interventions and evaluations and the patient’s response.
Health care facilities may use traditional narrative charting or an alternative system, such as problem-oriented medical record (POMR), problem-intervention-evaluation (PIE), FOCUS, charting-by-exception (CBE), FACT, core, and outcome documentation systems. In addition, many heath care facilities use computerized charting systems.
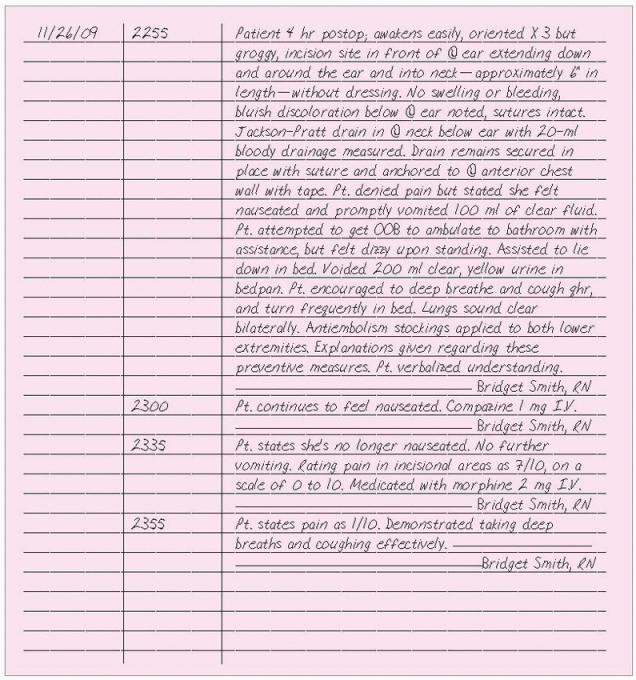
Traditional narrative charting
Narrative charting is a straightforward chronological account of the patient’s status, the nursing interventions performed, and the patient’s response to those interventions that is suitable in any clinical setting. Documentation is usually included in the progress notes and is supplemented by flow sheets. The Joint Commission standards require all health care facilities to set policies on how frequently patients should be assessed. Document patient assessments as often as your institution requires and more frequently when you observe any of the following:
♦ change in the patient’s condition
♦ patient’s response to a treatment or medication
♦ lack of improvement in the patient’s condition
♦ patient’s or family member’s response to teaching.
Document exactly what you hear, observe, inspect, do, or teach. Include as much specific, descriptive information as possible. Always document how your patient responds to care, treatments, and medications and his progress toward the desired outcome. Also include notification to the physician for changes that have occurred. Document this communication, the physician’s response, new orders that are followed, and the patient’s response.
You can organize your notes by using a head-to-toe approach or by referring
to the care plan and documenting the patient’s progress in relation to the plan and any unresolved problems. Regardless of the way you organize your narrative note, be specific and document chronologically, recording exact times.
to the care plan and documenting the patient’s progress in relation to the plan and any unresolved problems. Regardless of the way you organize your narrative note, be specific and document chronologically, recording exact times.
|
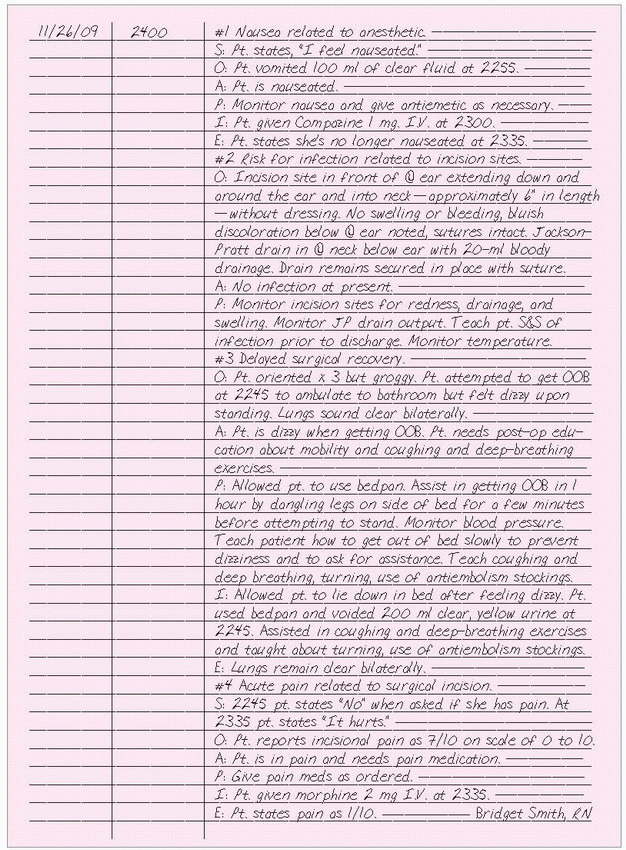
Problem-oriented medical record
The POMR system focuses on specific patient problems. Developed by physicians and later adapted by nurses, POMR has five components: the database, problem list, initial plan, progress notes, and discharge summary.
Database
Subjective and objective data about the patient form the initial care plan. These data are collected during the initial assessment of the patient and include such information as reason for hospitalization or treatment, medical history, allergies, medications, physical and psychosocial findings, self-care abilities, educational needs, and discharge planning concerns.
Problem list
A numbered list of the patient’s current problems in chronological order according to the date each was identified provides an overview of the patient’s health status. You can refer to it by number when writing your notes. When a problem is resolved, note the date and time and highlight the problem with a felt-tip pen.
Initial plan
This includes expected outcomes and plans for further data collection, patient care, and teaching. Involve patients and significant others in planning and setting goals.
Progress notes
Typically you must write a note for each current problem every 24 hours or when the patient’s condition changes. SOAP, SOAPIE, or SOAPIER is used to structure progress notes. If you have nothing to record for a component, simply omit the letter from the note. The components of SOAPIER include:
♦ Subjective data: chief complaint or other information the patient or family members tell you
♦ Objective data: factual, measurable data, such as observable signs and symptoms, vital signs, or test values
♦ Assessment data: conclusions based on subjective and objective data and formulated as patient problems or nursing diagnoses
♦ Plan: strategy for relieving the patient’s problems, including short- and long-term actions
♦ Interventions: measures you’ve taken to achieve expected outcomes
♦ Evaluation: analysis of the effectiveness of your interventions
♦ Revision: changes from the original care plan.
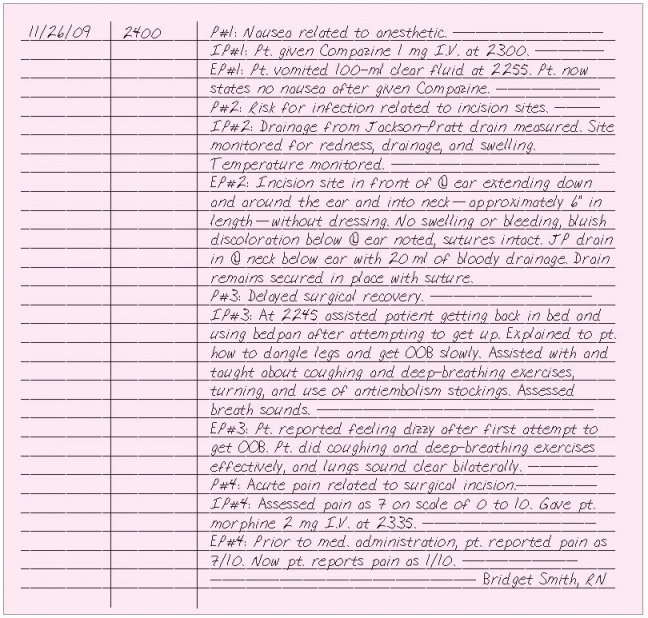
Problem-intervention-evaluation system
The PIE system organizes information according to patients’ problems. It requires that you keep a daily assessment flow sheet and progress notes. Integrating the care plan into the nurses’ progress notes eliminates the need for a separate care plan and provides a record that has a nursing—rather than medical—focus.
The daily assessment flow sheet includes areas for documenting assessment of major categories, such as respiration or pain, along with routine
care and monitoring. It usually provides spaces to document times treatments were given as well as continued assessments of a specific area such as neurologic checks every hour. Progress notes are organized according to PIE:
care and monitoring. It usually provides spaces to document times treatments were given as well as continued assessments of a specific area such as neurologic checks every hour. Progress notes are organized according to PIE:
Problem
Use data collected from your initial assessment to identify pertinent nursing diagnoses. Use the list of nursing diagnoses accepted by your facility, which usually corresponds to the diagnoses approved by the North American Nursing Diagnosis Association (NANDA). Some facilities use a separate problem list such as in the POMR. When documenting a problem in the progress notes, label it as P and number it; for example, P#1. This way you can refer to it later by number without having to re-document the problem statement.
|
Intervention
Document the nursing actions you take for each nursing diagnosis. Label each entry as I followed by P and the problem number; for example, IP#1.
Evaluation
The patient’s response to treatment makes up your evaluation. Use the label E followed by P and the problem number; for example, EP#1.
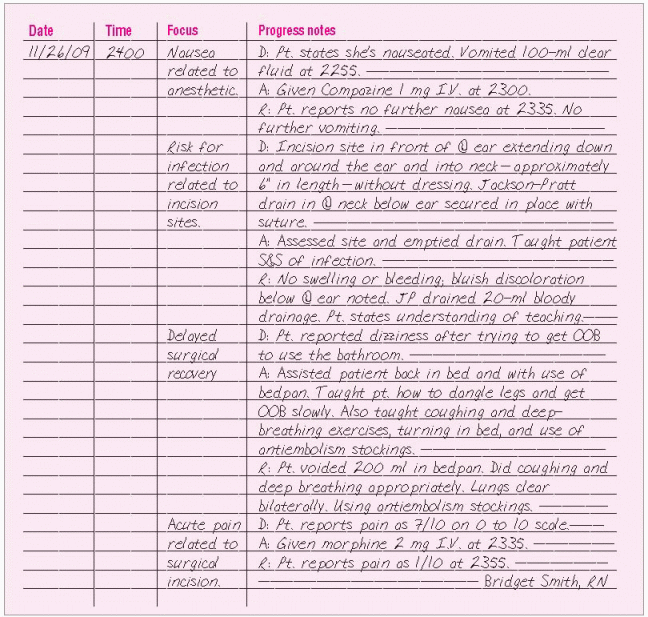
FOCUS charting
FOCUS charting is organized into patient-centered topics, or foci. It encourages you to use assessment data to evaluate these concerns.
Use a progress sheet with columns for the date, time, focus, and progress notes. In the focus column, write each focus as a nursing diagnosis, a sign or symptom, a patient behavior, a special need, an acute change in the patient’s condition, or a significant event. In the progress notes column, organize information using three categories: data (D), action (A), and response (R). In the data category, include subjective and objective information that describes the focus. In the action category, include immediate and future nursing actions based on your assessment of the patient’s condition and any changes to the care plan you deem necessary based on your evaluation. In the response category, describe the patient’s response to nursing or medical care. Using all three categories ensures concise documentation based on the nursing process. All other routine nursing tasks and assessment data can be documented on flow sheets and checklists.
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree