Chapter 4 Cultural Aspects of Health and Illness
Health Promotion and Maintenance
1. Explain the purpose of Healthy People 2020 as related to culture.
2. Incorporate cultural practices and beliefs into the patient’s plan of care.
3. Define culture, cultural diversity, cultural competence, and cultural sensitivity.
4. Discuss specific cultural practices, such as family roles and nutrition, which should be part of a cultural assessment.
5. Describe the best approach for caring for patients who are homeless.
6. Identify two major health issues related to the lesbian, gay, bisexual, and transgender (LGBT) population.
7. Identify two influences of culture on drug therapy.
8. Collaborate with the professional chaplain to manage a patient’s spiritual distress.
9. Describe two examples of generic and folk medicine that are used in the United States today.
10. Explain ways that nurses can communicate sensitively with patients from various cultural groups.
http://evolve.elsevier.com/Iggy/
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Review Questions for the NCLEX® Examination
Culture and Cultural Competence
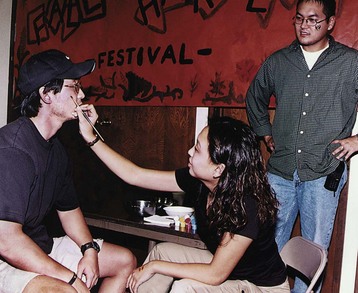
When considering cultural aspects of health, nurses and other health care staff need to understand the differences in commonly used terms: culture, cultural diversity, cultural competency, and cultural sensitivity. Culture is not restricted to race or ethnicity. Instead, culture is a broad term that refers to integrated patterns of behavior acquired over time, including beliefs, values, customs, norms, habits, language, thoughts, and ways of life. It is learned and transmitted primarily within the family unit, generation, and/or other social organizations and is shared by most of the members of the group. A person’s culture provides his or her worldview, which helps guide decision making and enhances self-worth (Fig. 4-1). Be sure to respect the clinical decisions made by all patients and their families, even if they differ from what you think the decisions should be.
Becoming culturally competent first requires you to examine your feelings and experiences regarding diversity, starting with an understanding of your own heritage. Then you will need to learn more about specific cultural differences so you can develop an appreciation for the values and beliefs of both patients and staff co-workers. Campinha-Bacote’s (2003) ASKED Model of Cultural Competence provides a beginning, basic self-assessment tool. Ask yourself the questions listed in Table 4-1.
TABLE 4-1 CAMPINHA-BACOTE’S ASKED MODEL OF CULTURAL COMPETENCE
Data from Dr. Josie Campinha-Bacote, expert in cultural nursing.
Purnell’s Domains of Culture
No one is expected to know the specific traits of every type of culture, including racial and ethnic groups. But you will need to continue learning as you interact with more and more diverse groups to develop cultural competence. Purnell & Paulanka (2008) have suggested 12 essential areas, or domains, to assess and understand any culture (Table 4-2). The most relevant of these cultural practices for nursing care are briefly reviewed here.
TABLE 4-2 PURNELL’S DOMAINS FOR ASSESSING CULTURAL GROUPS OR PERSONS
Data from Purnell, L. (2000). A description of the Purnell model for cultural competence. Journal of Transcultural Nursing, 11(1), 40-46.
Culture Overview and Communication
Overview and Localities
The ancestors of a large portion of the U.S. population left their native countries many decades or centuries ago. One of the biggest movements of newcomers was in the early 1940s. Many of these people were European, fleeing persecution or war-torn countries. More recent immigrants come to the United States for better opportunities for education, jobs, religious freedom, and democracy (Purnell & Paulanka, 2008).
Although ethnic minorities can be found anywhere throughout the United States, some have chosen to live in specific geographic areas with members of their culture for support and practice of traditional customs. For example, Asian Americans are concentrated in New York City and California. Hispanics, especially Mexicans and Latinos, tend to reside in the Southwestern United States, Texas, Florida, and California (Purnell & Paulanka, 2008). New York City also has a high percentage of people of Hispanic descent.
Homelessness
Homelessness can be either absolute or relative. Absolute homelessness is defined as having no physical home; those who are relatively homeless have some sort of shelter, although it may not be safe or sanitary (Badiaga et al., 2008). The severity of health care needs of this population is increasing while available resources are shrinking (Drury, 2008). Most patients use the emergency department for primary care and seek health care only because of complications of chronic disease. In many cases, these complications could be prevented with consistent treatment and follow-up. Major reasons that explain why the homeless avoid the health care community include (Jones et al., 2009):
The homeless are particularly prone to cardiovascular disease (CVD) because of poor nutrition, stress, and lack of preventive and follow-up care. The stress of being homeless, coupled with lack of ongoing health care, leads to hypertension, diabetes mellitus, and high cholesterol (Jones et al., 2009). To add to these risks, the typical diet of a homeless person includes high intake of saturated fats, sodium, and cholesterol. Stress-coping behaviors such as smoking, excessive alcohol, and illicit drug use also increase the risk for CVD.
• Staying in overcrowded shelters
• Having limited access to bathing and clean clothing
• Sharing bedding and clothing with others
• Having sex with multiple partners, especially without condoms
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree