Critical Thinking in Nursing Practice
Objectives
• Describe characteristics of a critical thinker.
• Discuss the nurse’s responsibility in making clinical decisions.
• Discuss how reflection improves clinical decision making.
• Describe the components of a critical thinking model for clinical decision making.
• Discuss critical thinking skills used in nursing practice.
• Explain the relationship between clinical experience and critical thinking.
• Discuss the critical thinking attitudes used in clinical decision making.
• Explain how professional standards influence a nurse’s clinical decisions.
• Discuss the relationship of the nursing process to critical thinking.
Key Terms
Clinical decision making, p. 196
Concept map, p. 202
Critical thinking, p. 193
Decision making, p. 195
Diagnostic reasoning, p. 196
Evidence-based knowledge, p. 193
Inference, p. 196
Nursing process, p. 197
Problem solving, p. 195
Reflection, p. 202
Scientific method, p. 195
![]()
Every day you think critically without realizing it. If it’s hot outside, you take off a sweater. If your DVD doesn’t start, you reposition the disc. If you decide to walk the dogs, you change to a pair of walking shoes. These examples involve critical thinking as you face each day and prepare for all possibilities. As a nurse, you will face many clinical situations involving patients, family members, health care staff, and peers. In each situation it is important to try to see the big picture and think smart. To think smart you have to develop critical thinking skills to face each new experience and problem involving a patient’s care with open-mindedness, creativity, confidence, and continual inquiry. When a patient develops a new set of symptoms, asks you to offer comfort, or requires a procedure, it is important to think critically and make sensible judgments so the patient receives the best nursing care possible. Critical thinking is not a simple step-by-step, linear process that you learn overnight. It is a process acquired only through experience, commitment, and an active curiosity toward learning.
Clinical Decisions in Nursing Practice
Nurses are responsible for making accurate and appropriate clinical decisions. Clinical decision making separates professional nurses from technical personnel. For example, a professional nurse observes for changes in patients, recognizes potential problems, identifies new problems as they arise, and takes immediate action when a patient’s clinical condition worsens. Technical personnel simply follow direction in completing aspects of care that the professional nurse has identified as necessary. A professional nurse relies on knowledge and experience when deciding if a patient is having complications that call for notification of a health care provider or decides if a teaching plan for a patient is ineffective and needs revision. Benner (1984) describes clinical decision making as judgment that includes critical and reflective thinking and action and application of scientific and practical logic. Most patients have health care problems for which there are no clear textbook solutions. Each patient’s problems are unique, a product of the patient’s physical health, lifestyle, culture, relationship with family and friends, living environment, and experiences. Thus as a nurse you do not always have a clear picture of a patient’s needs and the appropriate actions to take when first meeting a patient. Instead you must learn to question, wonder, and explore different perspectives and interpretations to find a solution that benefits the patient.
Because no two patients’ health problems are the same, you always apply critical thinking differently. Observe patients closely, gather information about them, examine ideas and inferences about patient problems, recognize the problems, consider scientific principles relating to the problems, and develop an approach to nursing care. With experience you learn to creatively seek new knowledge, act quickly when events change, and make quality decisions for patients’ well-being. You will find nursing to be rewarding and fulfilling through the clinical decisions you make.
Critical Thinking Defined
Mr. Jacobs is a 58-year-old patient who had a radical prostatectomy for prostate cancer yesterday. His nurse, Tonya, finds the patient lying supine in bed with arms extended along his sides but tensed. When Tonya checks the patient’s surgical wound and drainage device, she notes that the patient winces when she gently places her hands to palpate around the surgical incision. She asks Mr. Jacobs when he last turned onto his side, and he responds, “Not since last night some time.” Tonya asks Mr. Jacobs if he is having incisional pain, and he nods yes, saying, “It hurts too much to move.” Tonya considers the information she has observed and learned from the patient to determine that he is in pain and has reduced mobility because of it. She decides that she needs to take action to relieve Mr. Jacobs’ pain so she can turn him more frequently and begin to get him out of bed for his recovery.
In the case example the nurse observes the clinical situation, asks questions, considers what she knows about postoperative pain and risk for immobility, and takes action. The nurse applies critical thinking, a continuous process characterized by open-mindedness, continual inquiry, and perseverance, combined with a willingness to look at each unique patient situation and determine which identified assumptions are true and relevant (Heffner and Rudy, 2008). Critical thinking involves recognizing that an issue (e.g., patient problem) exists, analyzing information about the issue (e.g., clinical data about a patient), evaluating information (reviewing assumptions and evidence) and making conclusions (Settersten and Lauver, 2004). A critical thinker considers what is important in each clinical situation, imagines and explores alternatives, considers ethical principles, and makes informed decisions about the care of patients.
Critical thinking is a way of thinking about a situation that always asks “Why?”, “What am I missing?”, “What do I really know about this patient’s situation?”, and “What are my options?” (Heffner and Rudy, 2008; Paul and Heaslip, 1995). Tonya knew that pain was likely going to be a problem because the patient had extensive surgery. Her review of her observations and the patient’s report of pain confirmed her knowledge that pain was a problem. Her options include giving Mr. Jacobs an analgesic and waiting until it takes effect so she is able to reposition and make him more comfortable. Once he has less acute pain, Tonya offers to teach Mr. Jacobs some relaxation exercises.
You begin to learn critical thinking early in your practice. For example, as you learn about administering baths and other hygiene measures, take time to read your textbook and the nursing literature about the concept of comfort. What are the criteria for comfort? How do patients from other cultures perceive comfort? What are the many factors that promote comfort? The use of evidence-based knowledge, or knowledge based on research or clinical expertise, makes you an informed critical thinker. Thinking critically and learning about the concept of comfort prepares you to better anticipate your patients’ needs, identify comfort problems more quickly, and offer appropriate care. Critical thinking requires cognitive skills and the habit of asking questions, remaining well informed, being honest in facing personal biases, and always being willing to reconsider and think clearly about issues (Facione, 1990). When core critical thinking skills are applied to nursing, they show the complex nature of clinical decision making (Table 15-1). Being able to apply all of these skills takes practice. You also need to have a sound knowledge base and thoughtfully consider what you learn when caring for patients.
TABLE 15-1
| SKILL | NURSING PRACTICE APPLICATIONS |
| Interpretation | Be orderly in data collection. Look for patterns to categorize data (e.g., nursing diagnoses [see Chapter 17]). Clarify any data you are uncertain about. |
| Analysis | Be open-minded as you look at information about a patient. Do not make careless assumptions. Do the data reveal what you believe is true, or are there other options? |
| Inference | Look at the meaning and significance of findings. Are there relationships between findings? Do the data about the patient help you see that a problem exists? |
| Evaluation | Look at all situations objectively. Use criteria (e.g., expected outcomes, pain characteristics, learning objectives) to determine results of nursing actions. Reflect on your own behavior. |
| Explanation | Support your findings and conclusions. Use knowledge and experience to choose strategies to use in the care of patients. |
| Self-regulation | Reflect on your experiences. Identify the ways you can improve your own performance. What will make you believe that you have been successful? |
Modified from Facione P: Critical thinking: a statement of expert consensus for purposes of educational assessment and instruction. The Delphi report: research findings and recommendations prepared for the American Philosophical Association, ERIC Doc No. ED 315, Washington, DC, 1990, ERIC.
Nurses who apply critical thinking in their work are able to see the big picture from all possible perspectives. They focus clearly on options for solving problems and making decisions rather than quickly and carelessly forming quick solutions (Kataoka-Yahiro and Saylor, 1994). Nurses who work in crisis situations such as the emergency department often act quickly when patient problems develop. However, even these nurses exercise discipline in decision making to avoid premature and inappropriate decisions. Learning to think critically helps you care for patients as their advocate, or supporter, and make better-informed choices about their care. Facione and Facione (1996) identified concepts for thinking critically (Table 15-2). Critical thinking is more than just problem solving. It is a continuous attempt to improve how to apply yourself when faced with problems in patient care.
TABLE 15-2
Concepts for a Critical Thinker
| CONCEPT | CRITICAL THINKING BEHAVIOR |
| Truth seeking | Seek the true meaning of a situation. Be courageous, honest, and objective about asking questions. |
| Open-mindedness | Be tolerant of different views; be sensitive to the possibility of your own prejudices; respect the right of others to have different opinions. |
| Analyticity | Analyze potentially problematic situations; anticipate possible results or consequences; value reason; use evidence-based knowledge. |
| Systematicity | Be organized, focused; work hard in any inquiry. |
| Self-confidence | Trust in your own reasoning processes. |
| Inquisitiveness | Be eager to acquire knowledge and learn explanations even when applications of the knowledge are not immediately clear. Value learning for learning’s sake. |
| Maturity | Multiple solutions are acceptable. Reflect on your own judgments; have cognitive maturity. |
Modified from Facione N, Facione P: Externalizing the critical thinking in knowledge development and clinical judgment, Nurs Outlook 44(3):129, 1996.
Thinking and Learning
Learning is a lifelong process. Your intellectual and emotional growth involves learning new knowledge and refining your ability to think, problem solve, and make judgments. To learn, you have to be flexible and always open to new information. The science of nursing is growing rapidly, and there will always be new information for you to apply in practice. As you have more clinical experiences and apply the knowledge you learn, you will become better at forming assumptions, presenting ideas, and making valid conclusions.
When you care for a patient, always think ahead and ask these questions: What is the patient’s status now? How might it change and why? Which physiological and emotional responses do I anticipate? What do I know to improve the patient’s condition? In which way will specific therapies affect the patient? What should be my first action? Do not let your thinking become routine or standardized. Instead, learn to look beyond the obvious in any clinical situation, explore the patient’s unique responses to health alterations, and recognize which actions are needed to benefit the patient. With experience you are able to recognize patterns of behavior, see commonalities in signs and symptoms, and anticipate reactions to therapies. Thinking about these experiences allows you to better anticipate each new patient’s needs and recognize problems when they develop.
Levels of Critical Thinking in Nursing
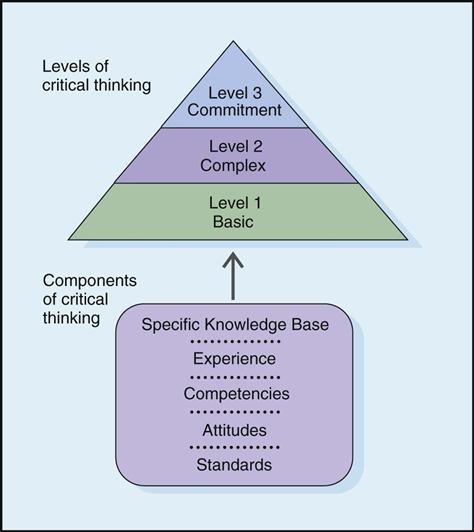
Your ability to think critically grows as you gain new knowledge in nursing practice. Kataoka-Yahiro and Saylor (1994) developed a critical thinking model (Fig. 15-1) that includes three levels: basic, complex, and commitment. An expert nurse thinks critically almost automatically. As a beginning student you make a more conscious effort to apply critical thinking because initially you are more task oriented and trying to learn how to organize nursing care activities. At first you apply the critical thinking model at the basic level. As you advance in practice, you adopt complex critical thinking and commitment.
Basic Critical Thinking
At the basic level of critical thinking a learner trusts that experts have the right answers for every problem. Thinking is concrete and based on a set of rules or principles. For example, as a nursing student you use a hospital procedure manual to confirm how to insert a Foley catheter. You likely follow the procedure step by step without adjusting it to meet a patient’s unique needs (e.g., positioning to minimize the patient’s pain or mobility restrictions). You do not have enough experience to anticipate how to individualize the procedure. At this level answers to complex problems are either right or wrong (e.g., when no urine drains from the catheter, the catheter tip must not be in the bladder), and one right answer usually exists for each problem. Basic critical thinking is an early step in developing reasoning (Kataoka-Yahiro and Saylor, 1994). A basic critical thinker learns to accept the diverse opinions and values of experts (e.g., instructors and staff nurse role models). However, inexperience, weak competencies, and inflexible attitudes can restrict a person’s ability to move to the next level of critical thinking.
Complex Critical Thinking
Complex critical thinkers begin to separate themselves from experts. They analyze and examine choices more independently. The person’s thinking abilities and initiative to look beyond expert opinion begin to change. A nurse learns that alternative and perhaps conflicting solutions exist.
Consider the case of Mr. Rosen, a 36-year-old man who had hip surgery. The patient is having pain but is refusing his ordered analgesic. His health care provider is concerned that the patient will not progress as planned, delaying rehabilitation. While discussing the importance of rehabilitation with Mr. Rosen, the nurse, Edwin, realizes the patient’s reason for not taking pain medication. Edwin learns that the patient practices meditation at home. As a complex critical thinker, Edwin recognizes that Mr. Rosen has options for pain relief. Edwin decides to discuss meditation and other nonpharmacological interventions with the patient as pain control options and how, when combined with analgesics, these interventions can potentially enhance pain relief.
In complex critical thinking each solution has benefits and risks that you weigh before making a final decision. There are options. Thinking becomes more creative and innovative. The complex critical thinker is willing to consider different options from routine procedures when complex situations develop. You learn a variety of different approaches for the same therapy.
Commitment
The third level of critical thinking is commitment (Kataoka-Yahiro and Saylor, 1994). At this level a person anticipates when to make choices without assistance from others and accepts accountability for decisions made. As a nurse you do more than just consider the complex alternatives that a problem poses. At the commitment level you choose an action or belief based on the available alternatives and support it. Sometimes an action is to not act or to delay an action until a later time. You choose to delay as a result of your experience and knowledge. Because you take accountability for the decision, you consider the results of the decision and determine whether it was appropriate.
Critical Thinking Competencies
Kataoka-Yahiro and Saylor (1994) describe critical thinking competencies as the cognitive processes a nurse uses to make judgments about the clinical care of patients. These include general critical thinking, specific critical thinking in clinical situations, and specific critical thinking in nursing. General critical thinking processes are not unique to nursing. They include the scientific method, problem solving, and decision making. Specific critical thinking competencies in clinical health care situations include diagnostic reasoning, clinical inference, and clinical decision making. The specific critical thinking competency in nursing involves use of the nursing process. Each of the competencies is discussed in the following paragraphs.
General Critical Thinking
Scientific Method
The scientific method is a way to solve problems using reasoning. It is a systematic, ordered approach to gathering data and solving problems used by nurses, physicians, and a variety of other health care professionals. This approach looks for the truth or verifies that a set of facts agrees with reality. Nurse researchers use the scientific method when testing research questions in nursing practice situations (see Chapter 5). The scientific method has five steps:
Consider the following example of the scientific method in nursing practice.
A nurse caring for patients who receive large doses of chemotherapy for ovarian cancer sees a pattern of patients developing severe inflammation in the mouth (mucositis) (identifies problem). The nurse reads research articles (collects data) about mucositis and learns that there is evidence to show that having patients keep ice in their mouths (cryotherapy) during the chemotherapy infusion reduces severity of mucositis after treatment. He or she asks (forms question), “Do patients with ovarian cancer who receive chemotherapy have less severe mucositis when given cryotherapy versus standard mouth rinse in the oral cavity?” The nurse then collaborates with colleagues to develop a nursing protocol for using ice with certain chemotherapy infusions. The nurses on the oncology unit collect information that allows them to compare the incidence and severity of mucositis for a group of patients who use cryotherapy versus those who use standard-practice mouth rinse (tests the question). They analyze the results of their project and find that the use of cryotherapy reduced the frequency and severity of mucositis in their patients (evaluating the results). They decide to continue the protocol for all patients with ovarian cancer.
Problem Solving
You face problems every day such as a computer program that doesn’t function properly or a close friend who has lost a favorite pet. When a problem arises, you obtain information and use it, plus what you already know, to find a solution. Patients routinely present problems in practice. For example, a home care nurse learns that a patient has difficulty taking her medications regularly. The patient is unable to describe what medications she has taken for the last 3 days. The medication bottles are labeled and filled. The nurse has to solve the problem of why the patient is not adhering to or following her medication schedule. The nurse knows that the patient was discharged from the hospital and had five medications ordered. The patient tells the nurse that she also takes two over-the-counter medications regularly. When the nurse asks her to show the medications that she takes in the morning, the nurse notices that she has difficulty reading the medication labels. The patient is able to describe the medications that she is to take but is uncertain about the times of administration. The nurse recommends having the patient’s pharmacy relabel the medications in larger lettering. In addition, the nurse shows the patient examples of pill organizers that will help her sort her medications by time of day for a period of 7 days.
Effective problem solving also involves evaluating the solution over time to make sure that it is effective. It becomes necessary to try different options if a problem recurs. From the previous example, during a follow-up visit the nurse finds that the patient has organized her medications correctly and is able to read the labels without difficulty. The nurse obtained information that correctly clarified the cause of the patient’s problem and tested a solution that proved successful. Having solved a problem in one situation adds to a nurse’s experience in practice, and this allows the nurse to apply that knowledge in future patient situations.
Decision Making
When you face a problem or situation and need to choose a course of action from several options, you are making a decision. Decision making is a product of critical thinking that focuses on problem resolution. Following a set of criteria helps to make a thorough and thoughtful decision. The criteria may be personal; based on an organizational policy; or, frequently in the case of nursing, a professional standard. For example, decision making occurs when a person decides on the choice of a health care provider. To make a decision, an individual has to recognize and define the problem or situation (need for a certain type of health care provider to provide medical care) and assess all options (consider recommended health care providers or choose one whose office is close to home). The person has to weigh each option against a set of personal criteria (experience, friendliness, and reputation), test possible options (talk directly with the different health care providers), consider the consequences of the decision (examine pros and cons of selecting one health care provider over another), and make a final decision. Although the set of criteria follows a sequence of steps, decision making involves moving back and forth when considering all criteria. It leads to informed conclusions that are supported by evidence and reason. Examples of decision making in the clinical area include determining which patient care priority requires the first response, choosing a type of dressing for a patient with a surgical wound, or selecting the best teaching approach for a family caregiver who will assist a patient who is returning home after a stroke.
Specific Critical Thinking
Diagnostic Reasoning and Inference
Once you receive information about a patient in a clinical situation, diagnostic reasoning begins. It is the analytical process for determining a patient’s health problems (Harjai and Tiwari, 2009). Accurate recognition of a patient’s problems is necessary before you decide on solutions and implement action. It requires you to assign meaning to the behaviors and physical signs and symptoms presented by a patient. Diagnostic reasoning begins when you interact with a patient or make physical or behavioral observations. An expert nurse sees the context of a patient situation (e.g., a patient who is feeling light-headed with blurred vision and who has a history of diabetes is possibly experiencing a problem with blood glucose levels), observes patterns and themes (e.g., symptoms that include weakness, hunger, and visual disturbances suggest hypoglycemia), and makes decisions quickly (e.g., offers a food source containing glucose). The information a nurse collects and analyzes leads to a diagnosis of a patient’s condition. Nurses do not make medical diagnoses, but they do assess and monitor patients closely and compare the patients’ signs and symptoms with those that are common to a medical diagnosis. This type of diagnostic reasoning helps health care providers pinpoint the nature of a problem more quickly and select proper therapies.
Part of diagnostic reasoning is clinical inference, the process of drawing conclusions from related pieces of evidence and previous experience with the evidence. An inference involves forming patterns of information from data before making a diagnosis. Seeing that a patient has lost appetite and experienced weight loss over the last month, the nurse infers that there is a nutritional problem. An example of diagnostic reasoning is forming a nursing diagnosis such as imbalanced nutrition: less than body requirements (see Chapter 17).
In diagnostic reasoning use patient data that you gather or collect to logically recognize the problem. For example, after turning a patient you see an area of redness on the right hip. You palpate the area and note that it is warm to the touch and the patient complains of tenderness. You press over the area with your finger; after you release pressure, the area does not blanch or turn white. After thinking about what you know about normal skin integrity and the effects of pressure, you form the diagnostic conclusion that the patient has a pressure ulcer. As a student, confirm your judgments with experienced nurses. At times you possibly will be wrong, but consulting with nurse experts gives you feedback to build on future clinical situations.
Often you cannot make a precise diagnosis during your first meeting with a patient. Sometimes you sense that a problem exists but do not have enough data to make a specific diagnosis. Some patients’ physical conditions limit their ability to tell you about symptoms. Some choose to not share sensitive and important information during your initial assessment. Some patients’ behaviors and physical responses become observable only under conditions not present during your initial assessment. When uncertain of a diagnosis, continue data collection. You have to critically analyze changing clinical situations until you are able to determine the patient’s unique situation. Diagnostic reasoning is a continuous behavior in nursing practice. Any diagnostic conclusions that you make will help the health care provider identify the nature of a problem more quickly and select appropriate medical therapies.
Clinical Decision Making
As in the case of general decision making, clinical decision making is a problem-solving activity that focuses on defining a problem and selecting an appropriate action. In clinical decision making a nurse identifies a patient’s problem and selects a nursing intervention. When you approach a clinical problem such as a patient who is less mobile and develops an area of redness over the hip, you make a decision that identifies the problem (impaired skin integrity in the form of a pressure ulcer) and choose the best nursing interventions (skin care and a turning schedule). Nurses make clinical decisions all the time to improve a patient’s health or maintain wellness. This means reducing the severity of the problem or resolving the problem completely. Clinical decision making requires careful reasoning (i.e., choosing the options for the best patient outcomes on the basis of the patient’s condition and the priority of the problem).
Improve your clinical decision making by knowing your patients. Nurse researchers found that expert nurses develop a level of knowing that leads to pattern recognition of patient symptoms and responses (White, 2003). For example, an expert nurse who has worked on a general surgery unit for many years is more likely able to detect signs of internal hemorrhage (e.g., fall in blood pressure, rapid pulse, change in consciousness) than a new nurse. Over time a combination of experience, time spent in a specific clinical area, and the quality of relationships formed with patients allow expert nurses to know clinical situations and quickly anticipate and select the right course of action. Spending more time during initial patient assessments to observe patient behavior and measure physical findings is a way to improve knowledge of your patients. In addition, consistently assessing and monitoring patients as problems occur help you to see how clinical changes develop over time. The selection of nursing therapies is built on both clinical knowledge and specific patient data, including:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree