Conception and Prenatal Development
Learning Objectives
After studying this chapter, you should be able to:
• Describe formation of the female and male gametes.
• Relate ovulation and ejaculation to the process of human conception.
• Explain implantation and nourishment of the embryo before development of the placenta.
• Describe normal prenatal development from conception through birth.
• Explain structure and function of the placenta, umbilical cord, and fetal membranes.
• Describe how common deviations from usual conception and prenatal development occur.
• Describe prenatal circulation and the circulatory changes after birth.
![]()
http://evolve.elsevier.com/McKinney/mat-ch/
A basic understanding of conception and prenatal development helps the nurse provide care to parents during normal childbearing and better understand problems such as infertility and birth defects. This chapter addresses formation of the gametes, the process of conception, prenatal development, and important auxiliary structures that support prenatal development. A short discussion of multifetal pregnancy is included.
Gametogenesis
To develop ova in females and spermatozoa in males, gametogenesis (creation of reproductive cells) requires a special reduction division called meiosis. Unlike mitosis, in which the diploid number of chromosomes (46) is retained in each new cell, meiosis halves the number of chromosomes (haploid number). Only one of each chromosome pair is directed to the gamete, 22 autosomes and 1 sex chromosome. When the sperm and ovum unite at conception, the “halves” form a new cell and restore the chromosome number to 46 (Table 12-1).
TABLE 12-1
COMPARISON OF FEMALE AND MALE GAMETOGENESIS
| OOGENESIS | SPERMATOGENESIS | |
| Time during which primary germ cells are produced | Fetal life. No others develop after about 30 weeks of gestation. | Continuously after puberty |
| Hormones that control process | GnRH FSH LH Estrogen | GnRH FSH LH Testosterone Estrogen (small amounts converted from testosterone) Growth hormone |
| Number of mature germ cells that develop from each primary cell | One | Four |
| Quantity | One during each reproductive cycle of about 28 days | 35-200 million are released with each ejaculation. |
| Size | Large. Visible to naked eye. Abundant cytoplasm to nourish embryo until implantation | Tiny compared with ovum. Little cytoplasm. Head is almost all nuclear material (chromosomes). |
| Motility | Relatively nonmotile. Carried along by action of cilia and currents within fallopian tubes | Independently motile by means of whiplike tail. Mitochondria in middle piece provide energy for motility. |
| Chromosome complement | 23 total: 22 autosomes plus one X sex chromosome | 23 total: 22 autosomes, plus either an X or a Y sex chromosome |
FSH, Follicle-stimulating hormone; GnRH, gonadotropin-releasing hormone; LH, luteinizing hormone.
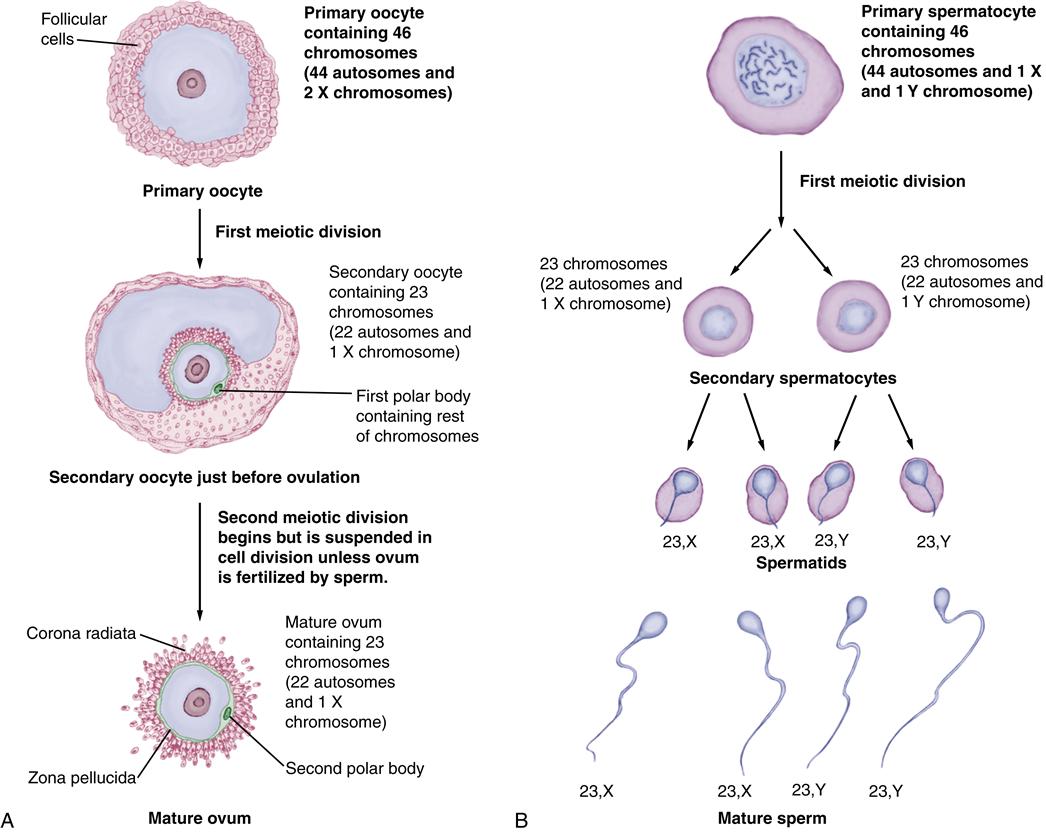
Oogenesis
Oogenesis (formation of ova or female gametes) begins during prenatal life, when primitive ova (oogonia) multiply by mitosis, like other somatic (body) cells throughout life. Each oogonium contains 46 chromosomes (22 pairs of autosomes, or non-sex chromosomes, and a pair of X chromosomes), as do other body cells. Before birth, the oogonia enlarge to form primary oocytes with a layer of follicular cells surrounding each one (Figure 12-1, A). These are called primary follicles. The primary oocyte begins its first meiotic division during fetal life but does not complete the process until puberty. The primary oocytes (still containing 46 chromosomes) remain dormant throughout childhood.
By the 30th week of gestation, the female fetus has all the ova she will ever have. Many of these ova regress during childhood (see Chapter 11, p. 207). When reproductive cycles begin at puberty, some of the primary follicles present at birth begin maturing. The cyclic process of gamete maturation continues throughout a woman’s reproductive years until the climacteric, or “change of life” (Blackburn, 2013; Carlson, 2009; Jones, 2009a; Moore & Persaud, 2008a, 2008b).
When the oocyte matures, two meiotic divisions reduce the chromosome number from 46 paired to 23 unpaired chromosomes: 22 autosomes and an X chromosome. Shortly before ovulation, the primary oocyte completes its first meiotic division, which began during fetal life. A secondary oocyte, now containing 23 unpaired chromosomes, results. The cytoplasm in the primary oocyte is divided unequally with this division, with most retained by the secondary oocyte. The remainder of cytoplasm, plus the other 23 chromosomes, goes into a tiny, nonfunctional polar body that soon degenerates.
At ovulation, the secondary oocyte begins dividing again (second meiotic division) to form a mature ovum. The 23 chromosomes duplicate themselves in the second meiotic division, but half of the duplicated chromosomes will be discarded if fertilization occurs. The second meiotic division is prolonged, and the mature ovum remains suspended in metaphase, the middle part of cell division. If fertilization occurs, the second meiotic division is completed, resulting in a mature ovum containing 23 chromosomes and a second tiny polar body containing the 23 discarded chromosomes that degenerates. If the ovum is not fertilized, it does not complete the second meiotic division and degenerates. In oogenesis, one primary oocyte results in a single mature ovum.
When released from the ovary, the mature ovum is surrounded by two layers—the zona pellucida and the cells of the corona radiata. These layers protect the ovum and prevent fertilization by more than one sperm. For fertilization to occur, the sperm must penetrate these two layers to reach the ovum’s cell nucleus.
Spermatogenesis
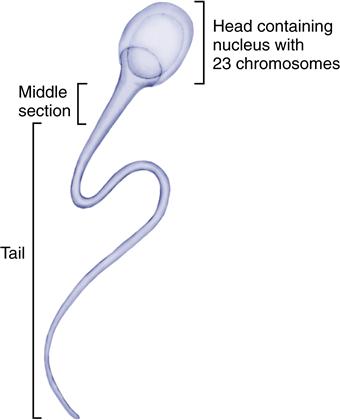
Spermatogenesis, or formation of sperm, begins during puberty in the male (Figure 12-1, B). Primitive sperm cells (spermatogonia) develop during fetal life and begin multiplying by mitosis during puberty. Unlike the female, the male produces new spermatogonia that can mature into sperm throughout his lifetime. Although male fertility gradually declines with age, men can father children in their 50s, 60s, and beyond.
Each spermatogonium contains 46 paired chromosomes, like other body cells. In the mature male, a spermatogonium enlarges to become a primary spermatocyte, still containing all 46 chromosomes. The first meiotic division forms two secondary spermatocytes and reduces the number to 23 unpaired chromosomes: 22 autosomes and 1 sex chromosome, either an X or a Y. Each secondary spermatocyte divides again in the second meiotic division to form two spermatids. Therefore half of the four spermatids that result from the two meiotic divisions of the spermatogonium carry an X chromosome and half carry a Y. The spermatids gradually mature into sperm.
The gamete from a male determines the sex of the new baby. If an X-bearing spermatozoon fertilizes the ovum, the baby is a girl. If a Y-bearing spermatozoon fertilizes the ovum, the baby is a boy.
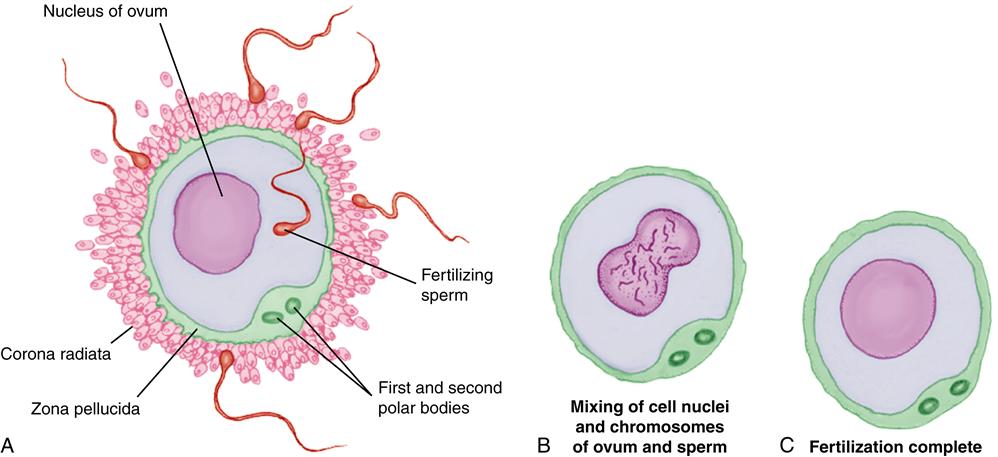
The mature sperm has three sections: a head, a middle portion, and a tail (Figure 12-2). The head is almost entirely the cell nucleus. The head contains the male chromosomes that join the chromosomes of the ovum. The middle portion supplies energy for the tail’s whiplike action. The movement of the tail propels the sperm toward the ovum.
Conception
Conception requires correct timing between release of a mature ovum at ovulation and ejaculation of enough healthy, mature, motile sperm into the vagina. The ovum may have the capacity to be fertilized no longer than 24 hours after ovulation, although the exact duration of its viability is unknown. Most sperm survive no more than 1 to 2 days although a few may remain fertile in the woman’s reproductive tract up to 80 hours (Blackburn, 2013; Carlson, 2009).
Preparation for Conception in the Female
Before ovulation, several oocytes begin to mature under the influence of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) from the woman’s anterior pituitary gland. Each maturing oocyte is contained in a sac within the ovary called the graafian follicle, which produces estrogen and progesterone to prepare the endometrium (uterine lining) for a possible pregnancy. Eventually one follicle outgrows the others. The less mature oocytes permanently regress.
Release of the Ovum
Ovulation, or release of the ovum, occurs about 14 days before a woman’s next menstrual period would begin. The follicle develops a thin spot on the surface of the ovary and ruptures, releasing the mature ovum with its surrounding cells on the surface of the ovary. There the collapsed follicle becomes the corpus luteum, which maintains the high estrogen and progesterone secretion necessary to make final preparation of the uterine lining for a fertilized ovum.
Ovum Transport
Released on the surface of the ovary, the mature ovum is picked up by the fimbriated (fringed) ends of the fallopian tube near the surface of the ovary. The ovum is transported through the tube by muscular action of the tube and movement of cilia within the tube. Fertilization normally occurs in the distal third of the fallopian tube, near the ovary. The ovum, fertilized or not, enters the uterus about 3 days after its release from the ovary.
Preparation for Conception in the Male
The male preparation for fertilizing the ovum consists of ejaculation, movement of the sperm in the female reproductive tract, and preparation of the sperm for actual fertilization.
Ejaculation
Expulsion of semen from the penis is ejaculation. When a male ejaculates during vaginal intercourse, 35 to 200 million sperm are deposited in the upper vagina and over the cervix (Blackburn, 2013; Hall, 2011; Jones, 2009b). The sperm are suspended in seminal fluid, which nourishes and protects them from the acidic vaginal environment. To hold the semen deeply in the vagina, the seminal fluid coagulates somewhat after ejaculation. The sperm are relatively immobile for about 15 to 30 minutes until other seminal enzymes dissolve the coagulated fluid and allow the sperm to begin moving upward through the cervix.
Transport of Sperm in the Female Reproductive Tract
Whiplike movement of the tails of spermatozoa propels them through the cervix, uterus, and fallopian tubes. Uterine contractions induced by prostaglandins in the seminal fluid enhance movement of the sperm toward the ovum. Only sperm cells enter the cervix. The seminal fluid remains in the vagina.
Many sperm are lost along the way. Some are digested by vaginal enzymes and phagocytes in the female reproductive tract, whereas others move into the wrong tube or past the ovum and out into the peritoneal cavity. Only a few hundred reach the fallopian tube where the ovum waits.
Preparation of Sperm for Fertilization
Sperm are not immediately ready to fertilize the ovum when they are ejaculated. While making the trip to the ovum, the sperm undergo changes (capacitation) that enable one to penetrate the protective layers surrounding the ovum. During capacitation, a glycoprotein coat and seminal proteins are removed from the acrosome (tip of the sperm head). After capacitation, the sperm look the same but are more active and can better penetrate the corona radiata and zona pellucida that surround the ovum.
The sperm that reach the ovum release an enzyme (hyaluronidase) to digest a pathway through the corona radiata and zona pellucida. Their tails beat harder to propel them toward the center of the ovum. Eventually, one spermatozoon penetrates the ovum.
Fertilization
Fertilization occurs when one spermatozoon enters the ovum and the two nuclei containing the parents’ chromosomes merge (Figure 12-3).
Entry of One Spermatozoon into the Ovum
Entry of a spermatozoon into the ovum has two results:
• Changes in the zona pellucida surrounding the ovum prevent other sperm from entering.
• The ovum, which has been suspended in the middle of its second meiotic division, completes meiosis.
The results are a nucleus with 23 chromosomes and expulsion of a second nonfunctional polar body. The mature ovum now contains 23 unpaired chromosomes, 22 autosomes, and 1 X chromosome in its nucleus.
Fusion of the Nuclei of Sperm and Ovum
Fusion of the nuclei of the sperm and ovum begins when the sperm enters the ovum. The sperm head enlarges, and the tail degenerates. The nuclei of the gametes move toward the center of the ovum, where the membranes surrounding their nuclei touch and dissolve. The 23 chromosomes from the sperm mingle with the 23 from the ovum, restoring the diploid number to 46. Fertilization is complete within 24 hours, and cell division of the zygote can begin when the nuclei of the sperm and ovum unite.
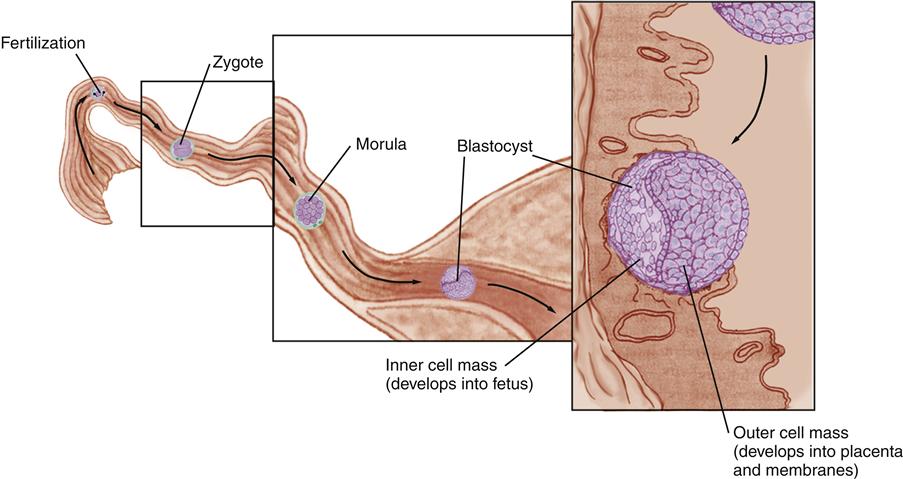
Pre-Embryonic Period
The pre-embryonic period is the first 2 weeks after conception. Figure 12-4 illustrates the period from fertilization through implantation.
Initiation of Cell Division
The zygote divides into two cells, then four, then eight cells while in the fallopian tube. Up to the 16-cell stage, the cells become smaller with each division, so they occupy about the same amount of space as the original ovum. When the conceptus (fertilized ovum) is a solid ball of 12 to 16 cells, it is called a morula because it resembles a mulberry.
The outer cells of the morula secrete fluid, creating a sac of cells (the blastocyst) that has an inner cell mass within the sac. The inner cell mass of the blastocyst develops into the fetus. Part of the outer layer of blastocyst cells develops into the placenta and fetal membranes.
Entry of the Zygote into the Uterus
The conceptus enters the uterus about 3 to 4 days after conception, when it contains about 100 cells. It lingers in the uterus another 2 to 4 days before beginning implantation. The endometrium, now called the decidua, is in the secretory phase of the reproductive cycle, 1½ weeks before the woman would begin her menstrual period. The endometrial glands are secreting at their maximum, providing rich fluids to nourish the conceptus before placental circulation is established. The endometrial spiral arteries are well developed in the secretory phase, providing easy access for developing the placental blood supply.
Implantation in the Decidua
The conceptus carries a small supply of nutrients for early cell division, but implantation (nidation) at the proper time and location in the uterus is crucial for continued development. Complete implantation is a gradual process that occurs between the 6th and 10th days. Embryonic structures continue developing during implantation.
Maintaining the Decidua
Implantation and survival of the conceptus are critically dependent on a continuing supply of estrogen and progesterone to maintain the decidua in the secretory phase. The zygote secretes human chorionic gonadotropin (hCG) to signal that a pregnancy has begun. With continued hCG production by the conceptus, the corpus luteum continues to secrete estrogen and progesterone rather than regressing.
Location of Implantation
The conceptus must be in the right place at the right time for normal implantation to occur. The site of implantation is important because that is the place that the placenta develops. Normal implantation occurs in the upper uterus (fundus). The upper uterus is the best area for implantation and placental development for three reasons:
Mechanism of Implantation
Enzymes produced by the conceptus erode the decidua, tapping maternal sources of nutrition. Primary chorionic villi are tiny projections on the surface of the conceptus. They extend into the decidua basalis that lies between the conceptus and the wall of the uterus. The chorionic villi eventually form the fetal side of the placenta; the decidua basalis forms the maternal side of the placenta (see Figure 16-14).
At this early stage, nutritive fluid passes to the embryo by diffusion (passive movement across a cell membrane from an area of higher concentration to one of lower concentration) because no circulatory system is yet established. By 10 days, the conceptus is fully embedded within the mother’s uterine decidua.
As the conceptus implants, usually near the time of the next expected menstrual period, a small amount of bleeding may occur at the site. The woman may think implantation bleeding is a normal menstrual period.
Embryonic Period
The embryonic period of development extends from the beginning of the 3rd week through the 8th week after conception. Basic structures of all major body organs are completed during the embryonic period. Table 12-2 presents major developments in body systems during prenatal life. Figure 12-5 (p. 222) illustrates the external appearance of the embryo from the 3rd through the 8th week after conception.
TABLE 12-2
TIMETABLE OF PRENATAL DEVELOPMENT BASED ON FERTILIZATION AGE∗
| NERVOUS/SENSORY SYSTEM | CARDIORESPIRATORY SYSTEM | DIGESTIVE SYSTEM | GENITOURINARY SYSTEM | MUSCULOSKELETAL SYSTEM | INTEGUMENTARY SYSTEM |
| 3 Weeks: 1.5 mm CRL | |||||
| Flat neural plate begins closing to form neural tube. Neural tube still open at each end. | Heart consists of two parallel tubes that fuse into a single tube. Contractions of heart tube begin. Chorionic villi of early placenta connect with heart. | Endoderm (inner germ layer) will become digestive tract. | Paired, cube-shaped swellings (somites) appear and will form most of the head and trunk skeleton. Muscle, bone, and cartilage develop from mesoderm. | Epidermis (outer skin layer) will develop from ectoderm (outer germ layer). Dermis (deep skin layer) and connective tissue will develop from mesoderm (middle germ layer). | |
| 4 Weeks: 4 mm CRL | |||||
| Neural tube closed at each end. Cranial end of neural tube will form brain; caudal end will form spinal cord. Eye development begins as an outgrowth of forebrain. Nose development begins as two pits. Inner ear begins developing from hindbrain. | Heart begins partitioning into four chambers and begins beating. Blood circulating through embryonic vessels and chorionic villi. Tracheal development begins as a bud on the upper gut and branches into two bronchial buds. | Development of primitive gut as embryo folds laterally. Stomach begins as a widening of the tube-shaped primitive gut. Liver, gallbladder, and biliary ducts begin as a bud from primitive gut. | Primordial germ (reproductive) cells are present on embryonic yolk sac. | Upper limb buds are present and look like flippers. Lower limb buds appear. | Mammary ridges that will develop into mammary glands appear. |
| 6 Weeks: 13 mm CRL | |||||
| Development of pituitary gland and cranial nerves. Head sharply flexed because of rapid brain growth. Eyelid development beginning. External ear development begins in neck region as six swellings. | Blood formation primarily in liver. Three right and two left lung lobes develop as outgrowths of the right and left bronchi. Partitioning of the heart into four chambers completed. | Most intestines are contained within the umbilical cord because the liver and kidneys occupy most of the abdominal cavity. Stomach nearing final form. Development of upper and lower jaws. | Kidneys are near bladder in the pelvis. Kidneys occupy much of the abdominal cavity. Primordial germ cells incorporated into developing gonads. Male and female gonads are identical in appearance. | Arms paddle shaped, fingers webbed. Feet and toes develop similarly, but a few days later than arms and hands. Bones cartilaginous, but ossification of skull begins. | Mammary glands begin development. Tooth buds for primary (deciduous) teeth begin developing. |
| 8 Weeks: 30 mm CRL | |||||
| Spinal cord stops at end of vertebral column. Taste buds begin developing. Eyelids fuse. Ears have final form but are low-set. | Heart partitioned into four chambers. Heartbeat detectable with ultrasound. Additional branching of bronchi. | Stomach has reached final form. Lips are fused. Intestines remain in umbilical cord. | Testes begin developing under influence of Y chromosome. Ovaries will develop if a Y chromosome is not present. External genitalia begin to differentiate but still appear quite similar. | Fingers and toes still webbed, but distinct by end of 8th week. Bones begin to ossify. Joints resemble those of adults. | Auricles of ear low-set but beginning to assume final shape. |
| 10 Weeks: 61 mm CRL; Weight: 14 g | |||||
| Head flexion still present, but straighter. Eyelids closed and fused. Top of external ear slightly below eye level. | May be possible to detect heartbeat with Doppler transducer. Blood produced in spleen and lymphatic tissue. | Intestines contained within abdominal cavity as growth of this cavity catches up with digestive system development. Digestive tract patent from mouth to anus. | Kidneys in their adult position. Male and female external genitalia have different appearance but are still easily confused. | Toes distinct; soles face each other. | Fingernails begin developing. Tooth buds for permanent teeth begin developing below those for primary teeth. |
| 12 Weeks: 87 mm CRL; Weight: 45 g | |||||
| Surface of brain is smooth, without sulci (grooves) or gyri (convolutions). Nasal septum and palate complete development. | Heartbeat should be detected with Doppler transducer. | Sucking reflex present. Bile formed by liver. | Kidneys begin producing urine. Male and female external genitalia can be distinguished by appearance. | Limbs are long and thin. Involuntary muscles of viscera develop. | Downy lanugo begins developing at end of this week. |
| 16 Weeks: 140 mm CRL; Weight: 200 g | |||||
| Face is human-looking because eyes face forward rather than to side. | Pulmonary vascular system developing rapidly. | Fetus swallows amniotic fluid and produces meconium (bowel contents). | Urine excreted into amniotic fluid. | Lower limbs reach final relative length, longer than upper limbs. A woman who has been pregnant before may begin to feel fetal movements. | External ears have enough cartilage to stand away from head somewhat. Blood vessels easily visible through the delicate skin. Fingerprints developing. |
| 20 Weeks: 160 mm CRL; Weight: 460 g | |||||
| Myelination of nerves begins and continues through first year of postnatal life. | Heartbeat should be detectable with regular fetoscope. | Peristalsis well developed. | More than 40% of nephrons are mature and functioning. Testes contained in abdomen but begin descent toward scrotum. Primordial follicles of ovary reach peak of 5-7 million and then gradually decline. | Fetal movements felt by mother and may be palpable by an experienced examiner. | Skin is thin and covered with vernix caseosa. Brown fat production complete. Nipples begin development. |
| 24 Weeks: 230 mm CRL; Weight: 820 g | |||||
| Spinal cord ends at level of first sacral vertebra because of more rapid growth of vertebral canal. | Primitive thin-walled alveoli (air sacs) have developed and are surrounded by capillary network. Surfactant production begins in lungs. Respiration possible, but most fetuses die if born at this time. | Testes descending toward inguinal rings. | Fetus is active. Fetal movements become progressively more noticeable to both mother and examiner. | Body appearance lean. Skin wrinkled and red. Fingerprints and footprints developed. Fingernails present. Eyebrows and lashes present. | |
| 28 Weeks: 270 mm CRL; Weight: 1300 g | |||||
| Major sulci and gyri are present. Eyelids no longer fused after 26 weeks. Responds to bitter substances on tongue. | Erythrocyte formation completely in bone marrow. Sufficient alveoli, surfactant, and capillary network to allow respiratory function, although respiratory distress syndrome is common. Many infants born at this time survive with intensive care. | Testes descended through inguinal canal into scrotum by end of 26th week. | Skin slightly wrinkled but smoothing out as subcutaneous fat is deposited under it. | ||
| 32 Weeks: 300 mm CRL; Weight: 2100 g | |||||
| Maturation of parasympathetic nears that of sympathetic nervous system, resulting in fetal heart rate variability on electronic fetal monitor tracing. | Surfactant production nears mature levels. Respiratory distress still possible if born at 32 weeks. Fetal heart rate variability gradually increases toward full term. | Skin smooth and pigmented. Large vessels visible beneath skin. Fingernails reach fingertips. Lanugo disappearing. | |||
| 38 Weeks: 360 mm CRL; Weight: 3400 g | |||||
| Sulci and gyri developed. Visual acuity about 20/600 at birth. | Newborn infant has about one eighth to one sixth the number of alveoli of an adult; well-developed ability to exchange gas. | Both testes usually palpable in scrotum at birth. The newborn girl’s ovaries contain about 1 million follicles. No new ones are formed after birth; their numbers continue to decline after birth. | Fetus plump, and skin smooth. Vernix caseosa present in major body creases. Lanugo present on shoulders and upper back only. Fingernails extend beyond the fingertips. Ear cartilage firm. | ||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree