Complications of Labor and Birth
Objectives
2. Discuss four factors associated with preterm labor.
3. Describe two major nursing assessments of a woman in preterm labor.
4. Explain why tocolytic agents are used in preterm labor.
5. Interpret the term premature rupture of membranes.
6. Identify two complications of premature rupture of membranes.
7. Differentiate between hypotonic and hypertonic uterine dysfunction.
8. Name and describe the three different types of breech presentation.
9. List two potential complications of a breech birth.
10. Explain the term cephalopelvic disproportion (CPD), and discuss the nursing management of CPD.
11. Define and identify three common methods used to induce labor.
12. Explain why an episiotomy is performed, and name two basic types of episiotomies.
13. Describe three types of lacerations that can occur during the birth process.
14. List two indications for using forceps to deliver the fetus.
15. Describe vacuum extraction.
17. Review the most common cause of rupture of the uterus during labor.
18. Describe umbilical cord prolapse, and state two associated potential complications.
19. List three potential complications of multifetal pregnancy.
20. Discuss five indications for a cesarean birth.
21. Describe the preoperative and postoperative care of a woman who is undergoing a cesarean birth.
22. Discuss the rationale for vaginal birth after a prior cesarean birth.
Key Terms
amnioinfusion (ăm-nē-ō-ĭn-FŪ-zhăn, p. 294)
amniotomy (ăm-nē-ŎT-ŏ-mē, p. 290)
augmentation of labor (ăwg-mĕn-TĀ-shŭn, p. 289)
Bishop score (p. 290)
caput chignon (kap´ət´shën´yän, p. 293)
cephalopelvic disproportion (CPD) (sĕf-ă-lō-PĔL-vĭc dĭs-prō-PŎR-shŭn, p. 286)
cesarean birth (sĕ-ZĀR-ē-ăn, p. 295)
chorioamnionitis (kō-rē-ō-ăm-nē-ō-NĪ-tĭs, p. 284)
dysfunctional labor (p. 285)
dystocia (dĭs-TŌ-sē-ă, p. 284)
episiotomy (ĕ-pēz-ē-ŎT-ō-mē, p. 291)
external version (p. 287)
fern test (p. 284)
forceps (p. 292)
hydramnios (hī-DRĂM-nē-ŏs, p. 293)
hypertonic uterine dysfunction (hī-pĕr-TŎN-ĭk Ū-tĕr-ĭn, p. 285)
hypotonic uterine dysfunction (hī-pō-TŎN-ĭk, p. 285)
induction of labor (p. 289)
multifetal pregnancy (mŭl-tē-FĒ-tăl, p. 294)
Nitrazine paper test (NĪ-tră-zēn, p. 284)
oligohydramnios (p. 294)
oxytocin (ŏks-ē-TŌ-sĭn, p. 290)
precipitate labor (prē-SĬP-ĭ-tāt, p. 293)
preterm labor (p. 280)
prolapsed umbilical cord (PRŌ-lăpst ŭm-BĬL-ĭ-kăl, p. 294)
prostaglandin (PGE2) gel (p. 290)
tocolytic agents (tō-kō-LĬT-ĭk, p. 283)
trial of labor after cesarean (TOLAC) (p. 300)
uterine rupture (p. 293)
vaginal birth after cesarean (VBAC) (p. 300)
 http://evolve.elsevier.com/Leifer/maternity
http://evolve.elsevier.com/Leifer/maternity
Labor and birth usually progress with few problems. However, when complications occur during labor, they can have devastating effects on the maternal-fetal outcome. Health care providers must quickly and accurately identify the nature of the problems and intervene to reduce or limit detrimental effects on the mother and newborn. This chapter discusses high-risk intrapartum care. Nursing care is incorporated throughout the chapter.
Preterm Labor
Preterm labor is defined as the onset of labor between 20 and 37 weeks’ gestation. It occurs in approximately 12% of pregnancies and accounts for most perinatal deaths not resulting from congenital anomalies. Preterm labor and premature rupture of membranes are the two most common factors that lead to preterm birth. Preterm birth has great significance for society because of the high rate of perinatal deaths and the excessive financial cost of caring for the preterm newborns. One of the Healthy People 2020 (U.S. Department of Health and Human Services, 2010) goals is for 90% of all pregnant women to have prenatal care starting in the first trimester and to reduce preterm labor and delivery. Early prenatal care makes it possible for the woman to reduce or eliminate some risk factors that contribute to preterm labor.
The criteria for diagnosing preterm labor include:
• Gestation between 20 and 37 weeks is considered preterm
• Late preterm is between 34 and 36 completed weeks of gestation
Associated Factors
The exact cause of preterm labor is unclear; however, several risk factors are known. Because epidemiologic data have shown some risk factors to be avoidable, there are some promising avenues for both prevention and treatment. Increased risk factors include poor prenatal care; infections, including periodontal (dental) infections; nutritional status; and sociodemographics (socioeconomic status, race, and lifestyle). Preterm labor, followed by preterm birth, has been associated with maternal anemia; urinary tract infection; cigarette smoking; and use of alcohol, cocaine, and other substances, all of which are potentially avoidable risk factors. In addition, alterations in maternal vaginal flora by pathogenic organisms (e.g., Chlamydia or Trichomonas organisms, bacterial vaginosis) are associated with preterm labor. The risk of spontaneous preterm birth increases as the length of the cervix decreases. The length of the cervix can be measured by transvaginal ultrasound.
Signs and Symptoms
Clinical manifestations of preterm labor are more subtle than for term labor. Health care providers and pregnant women need to know the warning signs of preterm labor. The health care provider should be notified of the following signs or symptoms:
Assessment and Management
Early prenatal care and education about prevention and the warning signs of preterm labor are extremely important to prevent preterm birth. The nurse should review the signs and symptoms that place a woman at risk for preterm labor and emphasize the importance of reporting the signs for prompt care in order to delay the newborn’s birth until the fetal lungs are mature enough for extrauterine life. Open communication between the woman, nurse, and other health team members is essential for collaborative care and successful prevention of preterm births. Once the woman has been identified as at high risk for preterm labor, the use of various strategies and more intense surveillance allows earlier identification and intervention for preterm labor.
When amniotic membrane integrity is lost, a protein in the amniotic fluid, called fibronectin, will be found in vaginal secretions. A vaginal swab for fetal fibronectin can help the physician decide which women should be treated most aggressively to stop preterm labor (Gabbe, Niebyl, & Simpson, 2007).
Infection is associated with preterm births. Identification and eradication of offending microorganisms that cause inflammation in the lower reproductive tract lessen the inflammatory response and provide a healthier cervix, thereby decreasing the incidence of preterm labor. Antibiotics may be prescribed prophylactically for women at risk for preterm labor, with premature rupture of the membranes, or with group B streptococcal cervical cultures.
The physician may order uterine activity monitoring at home for women at risk for preterm labor. The monitor assesses contractions only; it does not assess fetal heart rate. In the delivery unit, the pediatrician should be present to assist in assessment and resuscitation of the preterm newborn, and equipment and a working incubator for transportation to the neonatal intensive care unit (NICU) should also be available.
Stopping Preterm Labor
Once the woman is admitted to the hospital and the diagnosis of preterm labor is made, management focuses on stopping the uterine activity (contractions) before the cervix dilates beyond 3 cm, or “the point of no return.” The initial measures to stop preterm labor include identifying and treating any infection, restricting activity, ensuring hydration, and using tocolytic drugs (Table 14-1). The woman is placed on modified bed rest with bathroom privileges and is encouraged to maintain a lateral position. Assessment of uterine activity by palpation provides valuable information. The nurse communicates with the woman to help reduce her anxiety and concerns about fetal well-being and birth. Anxiety produces high levels of circulating catecholamines, which may induce further uterine activity. Explaining the planned care and procedures can reduce the patient’s fear of the unknown. Some drugs used as tocolytics may have an effect on carbohydrate metabolism and are used with caution in the diabetic patient.
Table 14-1
Drugs Used to Stop Preterm Labor (Tocolytics)
| Tocolytic Drug | Adverse Effects | Comments |
| Ritodrine (Yutopar) (β-adrenergic agonist) | Cardiovascular: maternal and fetal tachycardia Pulmonary: shortness of breath, chest pain, pulmonary edema, tachypnea Gastrointestinal: nausea, vomiting, diarrhea, ileus Central nervous system: tremors, jitteriness, restlessness, apprehension Metabolic alterations: hyperglycemia, hypokalemia, hypocalcemia | Approved by FDA but not in popular use. Side effects are dose related and more prominent during increases in the infusion rate than during maintenance therapy. ECG clearance suggested; hypertension and uncontrolled diabetes mellitus are contraindications. |
| Magnesium sulfate | Depression of deep tendon reflexes, respiratory depression, cardiac arrest (usually at serum magnesium levels >12 mg/dL) Less serious side effects: lethargy, weakness, visual blurring, headache, sensation of heat, nausea, vomiting, constipation, oliguria Fetal-neonatal effects: reduced heart rate variability, hypotonia | Adverse effects are dose related, occurring at higher serum levels. FHR and maternal vital signs must be monitored during labor and postpartum. |
| Indomethacin (prostaglandin synthesis inhibitor) | Epigastric pain, gastrointestinal bleeding; increased risk for bleeding; dizziness. Fetal effects: may have constriction of ductus arteriosus and decreased urinary output; decreased urinary output is associated with oligohydramnios, which may result in cord compression Respiratory distress syndrome | Not used after 32 weeks’ gestation or for more than 48-72 hours. Observe for maternal bleeding and adverse FHR patterns. |
| Nifedipine (Procardia) (calcium channel blocker) | Maternal flushing, transient tachycardia, hypotension; use with magnesium sulfate can cause serious hypotension and low calcium levels | Monitor for hypotension and increased serum glucose levels in those with diabetes. |
| Terbutaline (Brethine) (β-adrenergic agonist) | Tachycardia; monitor vital signs Shortness of breath; may cause hyperglycemia | Approved for investigational use and is widely used. Must not be used longer than 48 to 72 hours (FDA 2011) |
| Corticosteroids | Increased blood sugar | Given to accelerate production of surfactant, increase fetal lung maturity, and prevent neonatal intracranial hemorrhage |
| Betamethasone, dexamethasone | Monitor mother and newborn closely: mother for pulmonary edema and hyperglycemia, and newborn for heart rate changes | Given to mother 24-48 hours before birth of preterm newborn (<34 weeks of gestation) because it can hasten lung maturity |
Data from Clayton, B.D., Stock, Y.N., & Cooper, S.E. (2010). Basic pharmacology for nurses (15th ed.). St. Louis: Mosby; Creasy, R., Resnik, R., Iams, J., Lockwood, C., & Moore, T. (2008). Creasy & Resnik’s maternal-fetal medicine (6th ed.). Philadelphia: Saunders; London, M., Ladewig, P., Ball, J., & Bindler, R. (2006). Maternal & child nursing (2nd ed.). Upper Saddle River, NJ: Prentice Hall; American Congress of Obstetricians and Gynecologists. (2003). Management of preterm labor. International Journal of Gynecology & Obstetrics, 101, 1039–1047.
Tocolytics should not be used in women who are hemorrhaging because vasodilation may increase bleeding. If signs of fetal distress are noted, tocolytics may not be used if adequate survival therapy is available in the NICU. Tocolytics are usually not effective in a cervical dilation of 5 cm or more.
The woman should be asked to report any vaginal discharge (color, consistency, and odor). Baseline maternal vital signs are important and may provide clues of infection. Tachycardia and elevation of temperature can be early signs of amniotic fluid infection.
Fetal surveillance includes external fetal monitoring; fetal tachycardia of more than 160 beats/minute may indicate infection or distress. Fetal movement and biophysical profile assessment with the nonstress test (NST) provide information about fetal well-being. Special fetal assessment tests can be performed, such as measuring lecithin/sphingomyelin (L/S) ratio to determine fetal lung maturity.
Resting in the lateral position increases blood flow to the uterus and may decrease uterine activity. Strict bed rest may have some adverse side effects, which include muscle atrophy, bone loss, changes in cardiac output, decreased gastric motility, and gastric reflux. In addition, bed rest may result in depression and anxiety in the woman.
Hydration is encouraged, and intravenous fluids are often administered to increase vascular volume and prevent dehydration. The pituitary gland responds to dehydration by secreting antidiuretic hormone and oxytocin. Therefore, preventing dehydration will prevent oxytocin from being released. A baseline admission complete blood count is useful for determining whether there has been a decrease in the hemoglobin and hematocrit levels.
Use of tocolytic agents is an additional measure undertaken to stop uterine activity. The goal of tocolytic therapy is to delay delivery until steroids can hasten lung maturity of the fetus. Several drugs can be used, but none is without side effects. The nurse must know the adverse effects of the drug given and monitor the woman for their possible appearance. β-Adrenergic-agonist drugs such as terbutaline (Brethine) are often used as tocolytics. Terbutaline should not be used for longer than 48-72 hours and should not be used for home or maintenance therapy to prevent preterm labor. Terbutaline therapy may result in adverse effects to both the mother and fetus (FDA, 2011). Propranolol should be available to reverse adverse effects. Magnesium sulfate is also an effective tocolytic, and calcium gluconate 10% should be available to aid in reversing any toxic effects. Nursing responsibilities with this drug include hourly monitoring of maternal vital signs and oxygen saturation. Indocin (indomethacin) is a prostaglandin synthesis inhibitor that can be used as a tocolytic drug. Indocin can prolong maternal bleeding time, and the woman should be observed for unusual bruising. Fetal monitoring is essential when Indocin is used because it may have adverse effects on the fetus if used for more than 48 hours. Calcium antagonists, such as nifedipine (Procardia), reduce smooth muscle contractions of the uterus, and the woman must be monitored for hypotension (Iams, Romero, & Creasy, 2009).
Chapter 13 discusses the nurse’s role regarding assessment for magnesium sulfate toxicity. Intervention for magnesium sulfate administration is the same as when given to prevent seizures in gestational hypertension.
Promotion of Fetal Lung Maturity
Promotion of fetal lung maturity is a goal in management because respiratory distress syndrome (RDS) is a common problem in preterm newborns. Respiratory distress can be reduced if steroids, such as betamethasone or dexamethasone, are given to the mother at least 24 to 48 hours before the birth of a newborn who is less than 34 weeks’ gestation. After birth, preterm newborns are commonly treated prophylactically with surfactant therapy to reduce the risk of RDS.
Nursing Care Related to Pharmacologic Therapy
All tocolytic therapies have maternal risks; therefore, continuous assessment for effects of the drugs is indicated during administration. Intravenous tocolytics are given according to the institution’s protocol. Accurate intake and output, bilateral breath sounds, changes in vital signs, and mental status are closely monitored to identify early signs of fluid overload and pulmonary edema. If the woman is receiving β-adrenergic-agonist drugs such as Terbutaline, a heart rate of 120 beats/minute or greater, or a decrease in blood pressure to less than 90/40 mm Hg, should be immediately reported to the health care provider. These findings may indicate profound hemodynamic changes, including decreased ventricular filling time, decreased cardiac output, and myocardial infarction may occur if the drug is not discontinued. A pulse oximeter and arterial blood gas results may be used to determine maternal oxygenation and acid-base balance. The woman may be placed in the Fowler’s position and given oxygen as needed. Tocolytic therapy is discontinued if the woman has chest pain or shortness of breath. When corticosteroids are given, the nurse must observe for fluid retention and pulmonary edema. Indomethacin can constrict the ductus arteriosus in the fetus and reduces amniotic fluid by reducing fetal kidney function. Careful fetal monitoring is essential. Side effects of magnesium sulfate include a feeling of warmth, headache, nausea, and lethargy. Nifedipine and magnesium sulfate cannot be used together because low maternal calcium levels may occur. Progesterone therapy is under study for use as a tocolytic (ACOG, 2003).
Home Care Management
If the woman meets appropriate criteria, the primary health care provider may consider home care (see Chapter 18). There is evidence that using the home uterine activity monitor (HUAM) is effective in decreasing preterm births in a select group of women. Detecting contractions or contraction frequency before cervical changes occur makes HUAM worthwhile.
Premature Rupture of Membranes
Spontaneous rupture of the amniotic sac more than 1 hour before onset of true labor is referred to as premature rupture of membranes (PROMs). Rupture of the membranes before 37 weeks’ gestation is known as preterm premature rupture of the membranes (PPROMs). The exact cause is unknown, but there are several risk factors.
Infection for both the mother and the fetus is the major risk; when membranes are ruptured, microorganisms from the vagina can ascend into the amniotic sac. Compression of the umbilical cord can occur as a result of the loss of amniotic fluid. Prolapse of the cord can also occur, which results in fetal distress. Because amniotic fluid is slightly alkaline, confirmation that the vaginal fluid is amniotic fluid can be obtained by a Nitrazine paper test, which it will turn blue-green on contact with amniotic fluid (Skill 14-1). Examination of the fluid under a microscope (fern test) will also show a ferning pattern as the fluid dries.
Management
Treatment depends on the duration of gestation and whether evidence of infection or fetal or maternal compromise is present. For many women near term, PROM signifies the imminent onset of true labor. If pregnancy is at or near term and the cervix is soft and with some dilation and effacement, then augmentation of labor may be started a few hours after rupture. If the woman is not at term, the risk of infection or preterm birth is weighed against the risks of an induction by oxytocin or a cesarean birth (Nursing Care Plan 14-1 on p. 300).
Infection of the amniotic sac, called chorioamnionitis, may be caused by prematurely ruptured membranes because the barrier to the uterine cavity is broken. The risk of infection increases if the membranes have been ruptured for more than 18 hours.
Management will likely consist of bed rest with bathroom privileges and observation for infection, NST, and daily assessment for fetal compromise. Antibiotics are given to reduce infection and steroids to hasten fetal lung development (Table 14-2).
Table 14-2
Management of Women with Premature Rupture of the Membranes (PROM)
| Women with PROM | Preterm Fetus | Term Fetus |
| Bed rest Hydration Sedation Antibiotics, if needed Reassurance | Determination of PROM Assessment for prolapsed cord Observation for infection Administration of corticosteroids, with or without delivery in 24-48 hours Delivery when the infant has the best chance for survival (i.e., avoid fetal distress) Have emergency resuscitation equipment available | Induction of labor if spontaneous labor has not begun by approximately 12 hours after PROM Potential for cesarean birth Expectant management of maternal-fetal infection Increased chance of asphyxia and respiratory distress in newborn after birth |
The woman may remain in the hospital until birth; however, if there is no sign of infection or fetal compromise, she may return home and self-monitor. Preparation for nursing management includes:
• Documenting vital signs daily and reporting any temperature greater than 38° C (100.4° F)
• Providing sterile equipment for vaginal examinations
• Reporting uterine contractions
• Reporting any vaginal discharge or bleeding
• Having the woman remain on bed rest in a lateral position (with bathroom privileges)
• Explaining activity restrictions
• Explaining the need to abstain from sexual intercourse and orgasm
Dystocia
Dystocia, also known as dysfunctional labor, is a difficult or abnormal labor. It primarily results from one of the following problems (Table 14-3):
Powers: abnormal uterine activity (ineffective uterine contractions)
Passenger: abnormal fetal size or presentation (excessive size or less than optimum position)
Psyche: past experiences, culture, preparation, and support system
Table 14-3
Causes of Dystocia (Dysfunctional Labor)
| Cause | Examples |
| Difficulty with powers | Uterine dysfunction or abnormalities |
| Difficulty with passageway | Pelvic size and shape, tumors |
| Difficulty with passenger | Fetal abnormality Excessive size Malpresentation Malposition |
| Psyche | Maternal anxiety, fatigue |
Dystocia is suspected when the rate of cervical dilation or fetal descent is not progressing normally or uterine contractions are ineffective. A prolonged labor, with potential injury to the fetus, may result. Electronic fetal monitoring (EFM) is used to assess uterine contractions and fetal well-being. Nursing assessment of the intensity, frequency, and duration of contractions is important.
Dystocia can be associated with problems such as maternal dehydration, exhaustion, increased risk of infection, and fetal distress. Change in maternal vital signs, such as elevation of temperature or rise in pulse rate, should be reported. Comfort measures should be implemented by nursing personnel, and the woman and significant other should be kept informed about the progress of labor.
Powers
Abnormal Uterine Contractions
Dysfunctional labor can result from abnormal uterine contractions that prevent normal progress of cervical dilation, effacement, and descent of the presenting part. It can be further described as being primary (hypertonic dysfunction) or secondary (hypotonic dysfunction).
Hypotonic Dysfunction
Hypotonic uterine dysfunction (secondary uterine inertia) occurs with abnormally slow progress after the labor has been established (Table 14-4). The uterine contractions become weak and inefficient and may even stop. The contractions are fewer than two or three in a 10-minute period and usually are not strong enough to cause the cervix to dilate beyond 4 cm, and the fundus does not feel firm at the height (or acme) of the contraction. Consequently, labor fails to progress. A prolonged labor can occur, which can increase the risk of intrauterine infection, placing both the mother and newborn at risk.
Table 14-4
Comparison of Hypotonic and Hypertonic Labor
| When Occurs | Contractions | Implications | Management |
| Hypotonic Labor | |||
| Active phase; may occur in latent phase | Infrequent; poor intensity; low resting tone between contractions | Maternal: seldom painful; prolonged labor; PROM; risk of infection; anxiety Fetal: risk of subsequent sepsis | Rule out cephalopelvic disproportion; use intravenous oxytocin to stimulate contractions; perform cesarean birth for abnormal fetal position or large newborn. Nursing interventions: assess contraction pattern; provide support; monitor vital signs; frequently assess fetal status; if considering cesarean birth, instruct mother about procedure. |
| Hypertonic Labor | |||
| Prolonged latent phase; may occur in active phase | Become more frequent; ineffective; painful; uterus does not relax between contractions | Maternal: exhaustion, discouragement, fatigue, anxiety Fetal: possible distress with decreased placental perfusion | Analgesia for rest; hydration; oxytocin is not administered (discontinue intravenous oxytocin if infusing). Nursing interventions: assess uterine contraction pattern; provide rest (analgesia); provide comfort measures; monitor maternal vital signs; frequently monitor fetal status. Lateral position; administer oxygen by mask. |
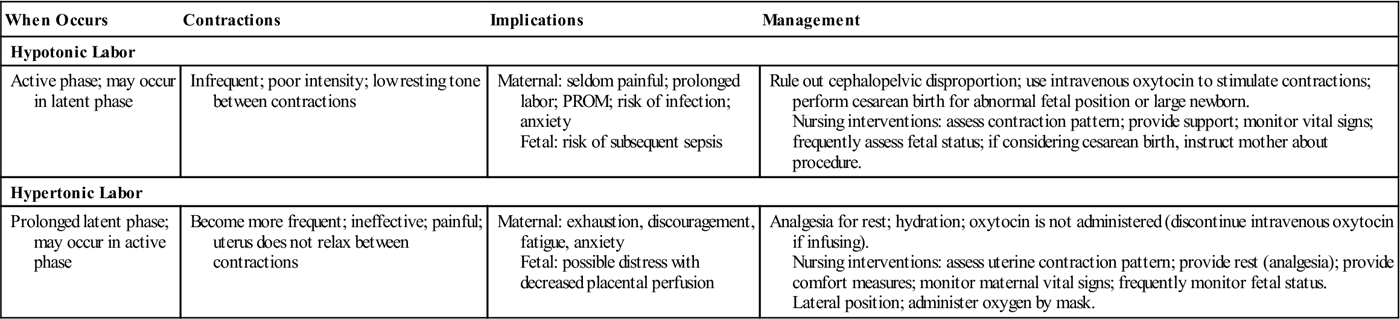
Hypotonic contractions occur as a result of fetopelvic disproportion, fetal malposition, overstretching of the uterus caused by a large newborn, multifetal gestation, or excessive maternal anxiety. The woman with hypotonic contractions can become exhausted and dehydrated. Medical management includes ruling out cephalopelvic disproportion (CPD) by ultrasound. If CPD is not the problem, augmentation by oxytocin is often started. The use of epidural analgesia and other regional anesthesia may reduce the effectiveness of the woman’s voluntary pushing efforts. Encouraging position changes and coaching can be helpful.
Hypertonic Uterine Dysfunction
Hypertonic uterine dysfunction refers to a labor with uterine contractions of poor quality that are painful, are out of proportion to their intensity, do not cause cervical dilation or effacement, and are usually uncoordinated and frequent (see Table 14-4). This is more common with a first pregnancy or an anxious woman who has intense pain and lack of labor progression. The latent period of labor is prolonged, which increases her exhaustion and anxiety. Often there is not adequate relaxation of muscle tone between contractions, which causes the woman to complain of constant cramps and results in ischemia or reduced blood flow to the fetus.
Management of hypertonic uterine dysfunction is rest, which is achieved by analgesia to reduce pain and encourage sleep. An intravenous infusion is frequently administered to maintain hydration and electrolyte balance. Often women awaken with normal contractions.
Passageway
Abnormal Pelvis Size or Shape
Contractures of the pelvic diameters reduce the capacity of the bony pelvis, including the inlet, midpelvis, outlet, or any combination of these planes. Pelvic contractures may be caused by congenital malformations, rickets, maternal malnutrition, tumors, and previous pelvic fractures.
Inlet contractures occur when the diagonal conjugate is shortened (less than 11.5 cm [4.5 inches]). Abnormal presentations, such as face and shoulder presentations, increase this problem. Midplane contractures are the most common cause of pelvic dystocia. Fetal descent is arrested (stops), and a cesarean birth is commonly done. Outlet contracture exists when the pubic arch is narrow. If uterine contractions continue when the passageway is obstructed, uterine rupture can occur, placing both the mother and fetus at risk. A common minor obstruction of the passageway is a distended bladder. Catheterization may be needed if the woman cannot void.
Scar tissue on the cervix from previous infections or surgery may not readily yield to labor forces to efface and dilate. A cesarean birth may be indicated when an abnormality of the passageway prolongs or impedes the progress of labor.
Passenger
Cephalopelvic Disproportion
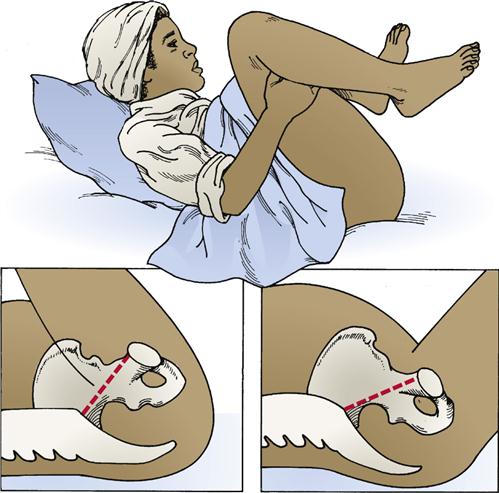
Cephalopelvic disproportion (CPD) is a condition in which the presenting part of the fetus (usually the head) is too large to pass through the woman’s pelvis. Because of the disproportion, it becomes physically impossible for the fetus to be delivered vaginally, and cesarean birth is necessary. CPD is suspected when the newborn’s head does not continue to descend even though the woman is having strong uterine contractions. Excessive fetal size may be associated with diabetes mellitus, multiparity, and genetics (one or both parents of large size). A large newborn (macrosomia) can cause difficulty in birth of the shoulders (shoulder dystocia). A modified position can aid in delivery  (Figure 14-1). Maternal complications that can occur are exhaustion, hemorrhage, and infection. Birth trauma and anoxia are complications for the fetus.
(Figure 14-1). Maternal complications that can occur are exhaustion, hemorrhage, and infection. Birth trauma and anoxia are complications for the fetus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



 Skill 14-1
Skill 14-1