Communicable Diseases
Frances A. Maurer
Focus Questions
What methods have been used historically to safeguard populations against communicable diseases?
What are the elements of a communicable disease, and how do they interact?
Key Terms
Agent
Artificial immunity
Bioterrorism
Host
Infective dose
Invasiveness
Natural immunity
Nosocomial infections
Pathogenicity
Reservoirs
Resistance
Sources of contamination
Vector
Virulence
Communicable diseases and control
Communicable diseases occur in every country, in every urban and rural area, and in every neighborhood, from the very rich to the very poor. Nurses who provide quality care in combating communicable diseases must have a basic understanding of epidemiology, infection control, microbiology, medicine, public health, and nursing. Furthermore, the community nurse must have knowledge of the legal system, which mandates prevention and control of communicable diseases locally, nationally, and worldwide. Nurses must also have knowledge of effective support systems that can be used by individuals, families, and communities.
The public health community faces new challenges. The resurgence of old diseases, such as measles and tuberculosis (TB); the appearance of drug-resistant bacteria such as methicillin-resistant Staphylococcus (MRSA) and Clostridium difficile (C. difficile); and the emergence of new diseases, such as severe acute respiratory syndrome (SARS) and Ebola virus disease, and the persistence of human immunodeficiency virus (HIV) infection and acquired immunodeficiency syndrome (AIDS), require health professionals to be alert, conscientious monitors of the public health. The potential for bioterrorism, the use of disease-producing agents as weapons, is also a growing concern of public health agencies.
Communicable disease control involves controlling environmental elements and personal behaviors that facilitate the spread of disease. The knowledge of how to control disease has been acquired through centuries of whimsical practice, lucky guesses, serendipitous observation, and strict scientific inquiry. The most dramatic controls have been achieved by establishing public hygiene measures. A brief historic review of attempts at disease control provides the community health nurse with an appreciation of the efforts needed to reach the level of disease control we have today.
Disease Control: Biblical Times to the Present
Communicable diseases such as smallpox and leprosy existed even before the birth of Christ. Plague raged intermittently throughout Europe and China during the thirteenth and fourteenth centuries, decimating the population. In the fourteenth century, physicians first formulated a theory to explain the communicable disease process. Although it was not completely accurate, this and subsequent trial-and-error efforts helped physicians develop sound principles for communicable disease control (Box 8-1). Today, quarantine, sanitary precautions, and travel restrictions remain methods of communicable disease control.
As the relationship between disease-producing microorganisms and factors that are beneficial to their growth became more apparent, control measures became more specific. Sanitary regulation of the environment and isolation of infected individuals became accepted strategies. These control measures were widely enforced. Streets were cleaned, the throwing of garbage into rivers and streets was discouraged, standing water was drained, and infected individuals were isolated. In America, quarantine laws became acceptable in the mid-1800s.
Early State and Federal Efforts at Disease Control
In 1869, the first state health department was established in Massachusetts; health departments in other states soon followed. By 1901 all but five states had some type of board of health. The Massachusetts health department controlled communicable diseases by regulating sanitary conditions and by building water and sewage systems. As boards of health developed, they began to realize the importance of accurate statistics for tracking and controlling communicable diseases. Statistics provided a way to identify trends, incidence, and effective treatment.
Communicable disease control at the federal level was almost nonexistent until the 1800s. In 1872, the Marine Hospital Service, the forerunner of the Public Health Service, was founded by an act of Congress. At approximately the same time, the American Public Health Association was established. The American Public Health Association provided a forum for physicians and other public health workers to set standards of care. In 1878 the Quarantine Act was passed, granting the federal government the power to impose quarantine. In 1912, the Marine Hospital Service officially became the Public Health Service (PHS), and states were held responsible for reporting statistics to the federal government via the PHS (Miller, 2002; Mullan, 1989).
Federal support for research assistance in communicable disease control led to several important actions. In 1930, the Ransdell Act established the National Institutes of Health (NIH), which continues to be the major source of research for the PHS. In 1946, the Communicable Disease Center, currently known as the Centers for Disease Control and Prevention (CDC), was established. The CDC’s original mandate was control of infectious diseases. Over the years, however, the scope of the CDC has expanded to include noninfectious diseases and environmental issues. The CDC is responsible for collecting morbidity and mortality statistics on reportable infectious diseases.
The 1970s were a decade of health reform and legislation. The needs of migrant workers were supported, and vaccines were made available to the poor. Funding for the NIH was increased, and a national effort began to decrease the incidence of cancer, heart attacks, and strokes. In the 1980s the important role of the PHS was underscored by the advent of HIV infection. The need for HIV infection prevention and education efforts, the issue of confidential or anonymous testing and counseling, the need for contact tracing and notification, and the care of infected individuals in hospitals and in the community have served to emphasize the need for a public health response to communicable diseases.
Today public health officials face many challenges, including the need for a quick response to a bioterrorism attack (see Chapter 22); the potential for rapid spread of infectious diseases due to the ease of travel between countries; and the rise of new and drug-resistant diseases. The public health community must meet these challenges in spite of limited funding for public health programs.
Successes in Communicable Disease Control
Public health practices have initiated community protection measures such as creating safer environmental conditions and providing treatments and vaccines as soon as they become available. Water quality regulations, sewage regulations, and food-handling regulations have decreased the incidence of enteric diseases. Currently, water is chlorinated, milk is pasteurized, preservatives are added to foods, and safe sewage plants are built. Antibiotics help reduce the spread of communicable diseases (e.g., rheumatic fever, TB, syphilis) by lessening the time during which infected persons are contagious.
Vaccine development and immunization programs eliminated smallpox and have dramatically decreased the incidence of childhood diseases such as measles, mumps, pertussis, polio, and rubella. In 1977 a national campaign, the Childhood Immunization Initiative, resulted in massive immunizations of young children. Unfortunately, a reduced emphasis on public health at the national level, with corresponding funding cuts, diminished the impact of this early immunization effort (Jekel et al., 2007). When the public becomes complacent, some diseases resurface or new ones emerge to affect the health of populations.
Contemporary issues in communicable disease
Despite significant success in communicable disease control since the 1940s, these diseases are still among the leading causes of death in the United States. Infectious diseases account for 25% of all doctor visits. When considered as a group, three infectious diseases—pneumonia, influenza, and HIV infection—constituted the ninth leading cause of death in the United States in 2007 (U.S. Department of Health and Human Services [USDHHS], 2010a). The public health community is especially concerned about a resurgence in the incidence of vaccine-preventable childhood illnesses (e.g., measles), TB, sexually transmitted diseases, and hepatitis and the emergence of new diseases, the most prominent of which are HIV infection, SARS, and West Nile virus infection (Table 8-1). The objectives of Healthy People 2020 (USDHHS, 2010b) have targeted all of these communicable diseases for special attention to significantly reduce their impact on the American people (refer to the Healthy People 2020 box on page 193).
Table 8-1
Frequency of Notifiable Diseases Over Time
| Disease | 1940 | 1950 | 1960 | 1970 | 1980 | 1990 | 2000 | 2010 |
| AIDS | 41,595* | 40,758** | ||||||
| Chlamydia (first report 1995) | 702, 093 | 1,244,180 | ||||||
| HIV | 36,870** | |||||||
| Legionellosis | 475* | 1,370 | 1,127 | 3,522 | ||||
| Lyme disease | 17,130 | 38,464 | ||||||
| Measles (rubeola) | 291,162 | 319,124 | 441,703 | 47,351 | 13,506 | 27,786 | 86 | 71++ |
| Mumps | NA | NA | NA | 104,953 | 8,576 | 5,292 | 338 | 1,991 |
| Pertussis | 183,866 | 120,718 | 14,809 | 4,249 | 1,730 | 4,570 | 7,867 | 16,858 |
| Poliomyelitis | 9,804 | 33,300 | 3,190 | 33 | 9 | 7 | 0 | 1 |
| Rabies, animal | 7,210 | 7,901 | 3,567 | 3,224 | 6,421 | 4,826 | 6,934 | 5,343 |
| Rabies, human | 41 | 18 | 2 | 3 | 0 | 1 | 0 | 4 |
| Rheumatic fever | NA | NA | 9,022 | 3,227 | 432 | 108 | ‡ | ‡ |
| Rubella (German measles) | NA | NA | NA | 56,552 | 3,904 | 1,125 | 185 | 5 |
| SARS | ¶ | |||||||
| Smallpox | 2,795 | Last Documented case in the United States was in 1949 | ||||||
| Syphilis | 472,900 | 217,558 | 122,538 | 91,382 | 68,382 | 134,255 | 32,221 | 44,828 |
| Tuberculosis | 102,984 | 217,742 | 122,538 | 91,382 | 68,832 | 134,255 | 16,377 | 11,545 |
| Typhoid fever | 9,809 | 2,484 | 816 | 346 | 510 | 552 | 377 | 397 |
| Varicella | 27,382 | 20,482*** | ||||||
| West Nile virus | 720¶ | |||||||
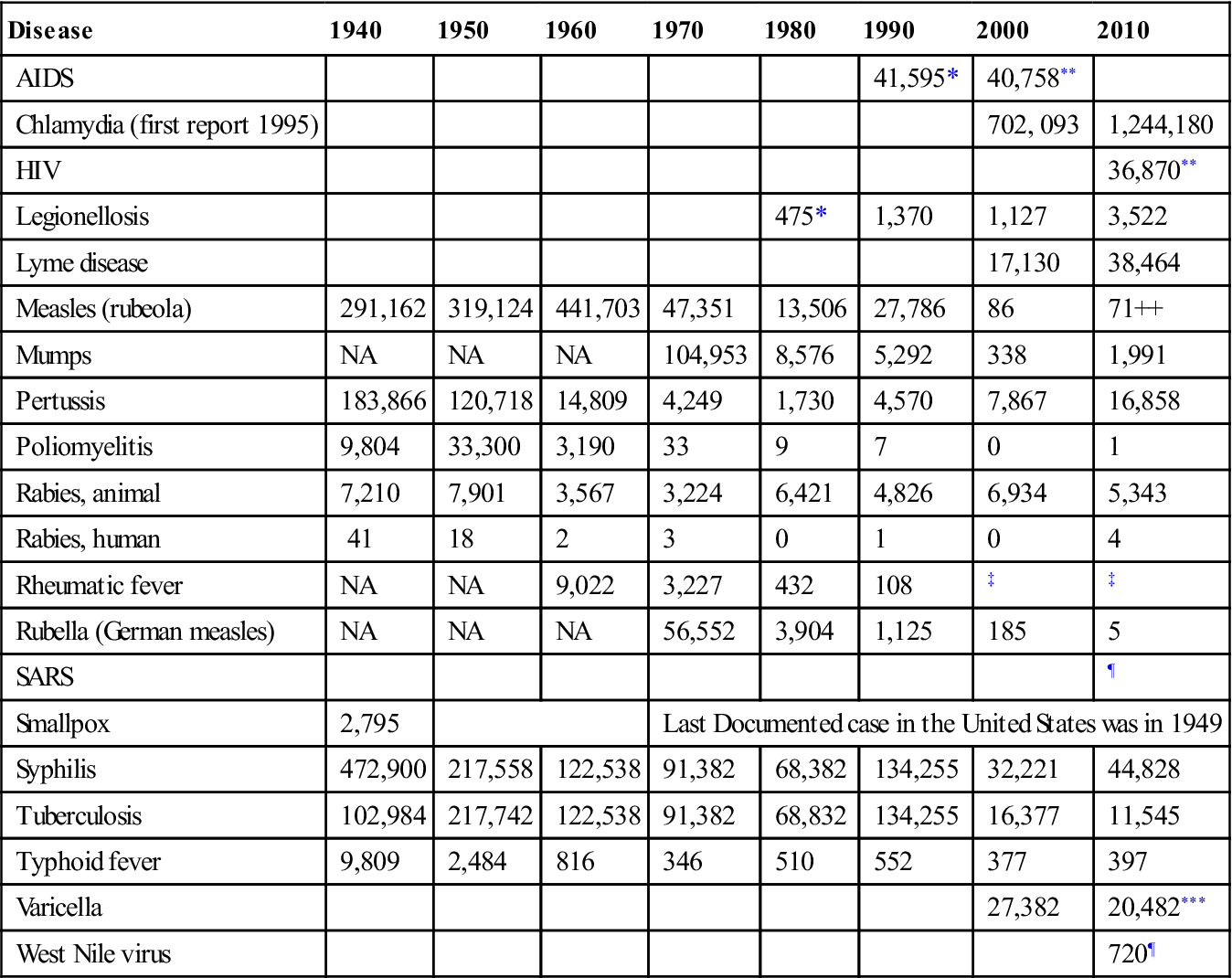
NA, Not available; SARS, severe acute respiratory syndrome.
*New emerging reportable disease.
**Combined HIV/AIDS reporting as of 2008.
***Added back to list in 2003.
‡No longer requires mandatory notification.
¶Not a reportable communicable disease at present; West Nile virus case reporting started in 2006; no current cases of SARS.
Data from Centers for Disease Control and Prevention. (1979). Annual summary and summary of notifiable diseases—1990, 2002, 2007, 2011. Atlanta: CDC.
Vaccine Failure and Lapsed Immunizations
The resurgence of certain communicable diseases has been the result of lapses in control measures and the diminished effect of vaccines over time.
Childhood Immunizations: Measles, Mumps, and Pertussis
Lapsed immunization efforts in the 1980s resulted in increased susceptibility to certain vaccine-preventable diseases. One proof of these lapsed immunization practices was the increase in measles cases in the late 1980s and early 1990s. Between 1989 and 1991, some 55,000 new cases were reported. Investigations of the resurgence of measles in high school and college populations revealed that the vaccine did not provide lifelong immunity. One to two booster doses are now recommended for continued protection against measles. Measles outbreaks continue to occur in unvaccinated children and adults. In the first third of 2011 there were 118 cases of measles, the highest rate since 1992 (CDC 2011a). Eighty-nine percent of those measles cases were among unvaccinated individuals and were associated with importation from other countries. In other words, the source cases were Americans traveling overseas and/or persons from other countries visiting this country.
As with measles, mumps outbreaks have occurred among highly vaccinated populations. The risk of mumps has shifted from young children to older children, adolescents, and young adults and is usually associated with vaccine failure over time. The two-dose schedule of measles, mumps, and rubella vaccine (MMR) adopted in 1989 led to a 95% decline in the incidence of mumps (CDC, 2001a). A resurgence of mumps among adolescents and young adults who had received the recommended two doses has led to the recommendation of a third dose for those at high risk (CDC, 2006a; 2010a)
Pertussis outbreaks have occurred in undervaccinated populations. In 2004 and 2005, 345 cases of pertussis were reported among Amish preschool-age children in Delaware (CDC, 2006a). Vaccination rates among the Amish are low, although vaccination is not prohibited by their religion. Pertussis rates continue to rise. In 2009 there were approximately 17,000 cases (CDC, 2011b). In 2005 the CDC recommended a reconditioned tetanus toxoid-reduced diphtheria toxoid-acellular pertussis vaccine (Tdap) for use among adolescents and adults. Adolescents who have had Tdap vaccine have fewer incidences of pertussis than those who have not (CDC, 2011b).
To evaluate the degree of immunization coverage, the National Immunization Program at the CDC established a population-based immunization registry. Registries at the state and local levels track each child’s immunization status. This information is necessary to ensure protection of the population from vaccine-preventable diseases and to identify children who are at risk when exposed to disease. A Healthy People 2020 objective is to have 95% of children under 6 years of age enrolled in the immunization registry. In 2008, 75% of children were enrolled (USDHHS, 2010b).
Significant progress has been made in inoculating young children. By 2007, 95% of school-aged children in kindergarten and first grade had had all the recommended vaccinations (USDHHS, 2010b). Ninety percent vaccination of susceptible groups provides substantial protection against a recurrent epidemic. Monitoring of vaccination status for entry into school and daycare identifies children at risk. In Washington, DC, for example, a review of immunization status by school nurses determined that 50% of children needed one or more vaccinations to meet the district’s school entry requirement (CDC, 2003a). Stringent surveillance has increased the complete immunization rate to 90% of all DC students (CDC, 2011c).
Failure to Implement Recommended Vaccinations: Pneumococcal Pneumonia and Influenza
Several episodes of pneumonia outbreaks in chronic care facilities in Massachusetts, Maryland, and Oklahoma in 1995 and 1996 were determined to be the result of failure to vaccinate at-risk populations with pneumococcal pneumonia vaccine. Investigation revealed that fewer than 5% of these institutions’ populations were immunized. The death rate at the three institutions ranged from 20% to 28% of infected seniors (CDC, 1997a)—a preventable tragedy.
Pneumococcal disease and influenza account for over 53,000 deaths each year (CDC, 2010b). The majority of these deaths occur in people over the age of 65. Influenza immunization rates are approximately 67% in this age group. Pneumococcal vaccination rates in older adults have improved but are still low (61%) (USDHHS, 2010a). Nurses should make an effort to ensure that both vaccinations are routinely administered in hospitals, nursing homes, congregate settings, and other community settings that serve the older adult population.
Drug-Resistant Diseases
One trend of special concern to public health practitioners is the increase in drug-resistant strains of organisms that cause communicable diseases. After years of successful treatment, cases of gonorrhea, TB, pneumonia, and syphilis are on the rise. These increases are the result of less success with standard antibiotic therapies. Examples of drug-resistant organisms are the following:
• Neisseria gonorrhoeae—resistant to fluoroquinolone; cases spread from Hawaii and Los Angeles to all regions of the country (CDC, 2011d)
• Neisseria gonorrhoeae—resistant to azithromycin in a small but growing number of cases in the United States (CDC 2011e)
• Staphylococcus aureus—commonly resistant to methicillin and now becoming resistant to vancomycin, the last currently known drug treatment choice (CDC, 2006b, 2006c, 2010c)
• Salmonella—a new strain, serotype Typhimurium, is resistant to ampicillin, chloramphenicol, streptomycin, sulfonamides, and tetracycline; strain is common in the United Kingdom and has now spread to the United States (CDC, 1997b: Wright et al., 2005)
• Shigella sonnei (gastroenteritis)—resistant to ampicillin and trimethoprim-sulfamethoxazole; cases found in daycare centers in Kansas, Kentucky, and Missouri (CDC, 2006d)
Drug-resistant communicable diseases are a special concern not only because they are more complicated to treat but also because the delay in control increases the risk of infection for every person, including health care workers. Community health nurses must be alert to screen high-risk groups (Box 8-2), be aware of current treatments, and be able to identify the signs of drug-resistant infection in clients. In addition, community health professionals must take an active role in educating practitioners and the public alike concerning the prudent use of antimicrobial drugs to reduce the emergence of drug-resistant strains.
Methicillin Resistant Staphylococcus Aureus (MRSA)
MRSA is a staph bacteria resistant to methicillin, oxacillin, penicillin, amoxicillin, and sometimes to vancomycin. MRSA infections that are community located (14%) usually present as a skin infection. Most community-acquired infections are mild, although some have become life threatening. More severe MRSA infections (85%) occur in hospital and other health care facilities and are very serious infections (CDC, 2010c). MRSA can present in surgical wounds, urinary tract infections, bloodstream infections, and pneumonia. Stringent universal precautions in intensive care units and other specialty units have reduced the incidence of hospital-acquired MRSA. Little progress has been made in the incidence of community-acquired MRSA (CA-MRSA) and in fact the number and virulence of CA-MRSA cases has alarmed public health officials (Milstone et al., 2010).
Fluoroquinolone Resistant Clostridium Difficile (C. Difficile)
C. difficile bacteria is indigenous to the intestinal tract. It proliferates after antibiotic use has reduced the number of healthy intestinal bacteria that served to keep C. difficile in check. Symptoms range from mild diarrhea to severe infections. C. difficile is the most common cause of bacterial diarrhea in hospitalized patients. Control includes modifying antibiotic therapies, stringent cleaning of equipment and rooms, and scrupulous personal hygiene (Hall, 2010).
Tuberculosis: Difficult to Control
Nearly one third of the world’s population is infected with TB. It is a leading infectious cause of death worldwide, causing more than 2 million deaths each year (CDC, 2011f). Persons infected with the TB organism but without overt disease are asymptomatic and are not contagious to others. If infection progresses to TB disease, individuals will have symptoms and become contagious. A person who has a compromised immune system, practices poor nutrition, lives in poverty, or has other diseases is at greater risk of progressing from TB infection to TB disease (see Chapter 21). People who live in or emigrate from countries in which TB is indigenous are at greater risk of having been infected (see Chapter 5). Without prophylactic treatment for the infection, individuals have a 5% to 10% chance of progressing to disease (CDC, 2008a). HIV-infected individuals are at special risk. The number of persons with the dual diagnosis of HIV and TB has increased dramatically, with approximately 10% of all TB cases also having HIV (CDC, 2008a).
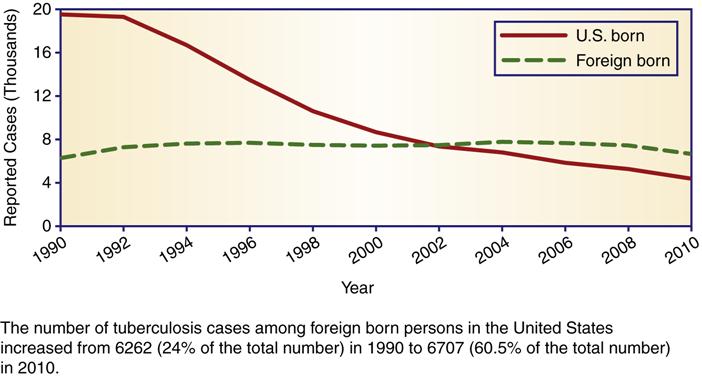
The risk of acquiring TB infection or disease is relatively low in the United States. Immigrants from countries in which TB is indigenous are at greater risk because they are more likely to have been exposed and infected in their country of origin (CDC, 2011f). Although the total number of TB cases has declined, the incidence among foreign-born persons as a percentage of total cases has increased (Figure 8-1). The TB case rate among foreign-born persons in the United States is eleven times greater than U.S.-born persons (CDC, 2010d). Today, public health agencies have renewed efforts to identify and treat foreign-born individuals. Closing the gap between TB rates among foreign-born and native-born Americans is a national health objective and a goal of the CDC.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


