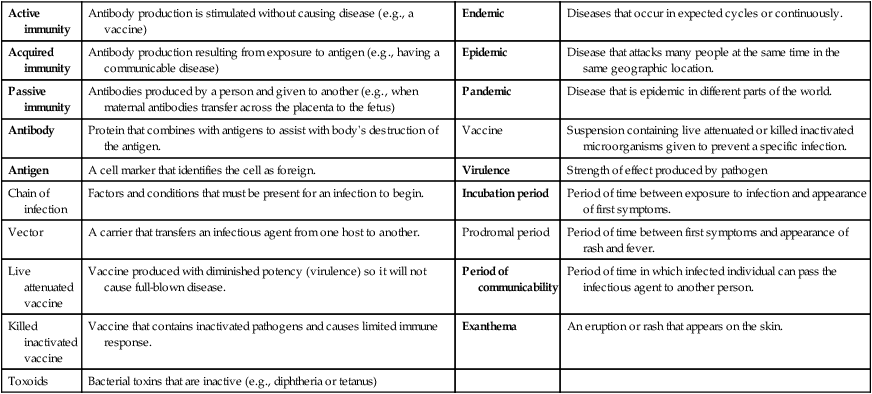
1. Define the vocabulary terms listed 2. Identify the components of chain of infections and specific interventions to break the chain 3. Discuss transmission modes for communicable diseases in children 4. Identify interventions to decrease transmission of a communicable disease 5. Identify the appropriate isolation precaution for each communicable disease 6. Develop a plan for home care for a child with a communicable disease 7. List the immunizations given during the first year, and include the approximate age for each 8. Discuss ways to educate parents about the importance of immunizations A communicable disease is an infection that has been transmitted by direct or indirect contact, vehicle or vector, or airborne route. Communicable diseases are also known as infectious diseases. Infectious and communicable diseases account for the major cause of illness for infants and children. There are several factors that make infants and children susceptible to these diseases. Their immune system is not fully developed until 6 years of age (see Chapter 19), and they have not developed antibodies against many of the organisms. Many children attend day care during the first year of life, which increases their risk of exposure. Developmentally, infants have hand-to-mouth behavior, which is a source of infection. While many toddlers are still in diapers and are learning to be toilet trained, they may not always wash their hands, and this increases the risk of transmission. They are also exploring their environment and coming in contact with animals. School-age children are exposed to many potential infections through their school. Many are lax with hand hygiene, and they share items among their peers. • Reservoir (environment in which the organism exists and multiplies) • Portal of exit (route by which the organism leaves the reservoir) • Transmission mode (airborne, contact, droplet) • Portal of entry to host (route by which the organism enters the host) When a communicable disease is suspected, a thorough history must be obtained. The nurse asks whether the child has recently been exposed to a communicable disease, has been immunized, or has already had the disease. The nurse may inquire whether the child has experienced any of the prodromal symptoms (symptoms indicating the onset of a disease). Table 18-1 lists common terms used with communicable diseases. Table 18-1 Common Terms Used with Communicable Diseases Table 18-2 summarizes the nursing care of several common communicable diseases. Smallpox is included to familiarize the student with information on a disease that might be used in an event of bioterrorism. Table 18-2
Communicable Diseases
![]() http://evolve.elsevier.com/Price/pediatric/
http://evolve.elsevier.com/Price/pediatric/
Communicable Diseases
Active immunity
Antibody production is stimulated without causing disease (e.g., a vaccine)
Endemic
Diseases that occur in expected cycles or continuously.
Acquired immunity
Antibody production resulting from exposure to antigen (e.g., having a communicable disease)
Epidemic
Disease that attacks many people at the same time in the same geographic location.
Passive immunity
Antibodies produced by a person and given to another (e.g., when maternal antibodies transfer across the placenta to the fetus)
Pandemic
Disease that is epidemic in different parts of the world.
Antibody
Protein that combines with antigens to assist with body’s destruction of the antigen.
Vaccine
Suspension containing live attenuated or killed inactivated microorganisms given to prevent a specific infection.
Antigen
A cell marker that identifies the cell as foreign.
Virulence
Strength of effect produced by pathogen
Chain of infection
Factors and conditions that must be present for an infection to begin.
Incubation period
Period of time between exposure to infection and appearance of first symptoms.
Vector
A carrier that transfers an infectious agent from one host to another.
Prodromal period
Period of time between first symptoms and appearance of rash and fever.
Live attenuated vaccine
Vaccine produced with diminished potency (virulence) so it will not cause full-blown disease.
Period of communicability
Period of time in which infected individual can pass the infectious agent to another person.
Killed inactivated vaccine
Vaccine that contains inactivated pathogens and causes limited immune response.
Exanthema
An eruption or rash that appears on the skin.
Toxoids
Bacterial toxins that are inactive (e.g., diphtheria or tetanus)
DISEASE
COMMUNICABILITY PERIOD AND ROUTE
CLINICAL MANIFESTATIONS
TREATMENT AND NURSING CARE
COMPLICATIONS
Chickenpox (Varicella)
5 days after onset of rash and until all lesions are crusted
Route: Airborne, droplet infection; direct or indirect contact
Dry scabs are not infectious
General malaise, slight fever, anorexia, headache. Successive crops of macules, papules, vesicles, crusts. These may all be present at the same time. Itching of the skin. Generalized lymphadenopathy.
Oral acyclovir should be considered for otherwise healthy people at increased risk (e.g., people older than 12 yr of age, individuals with pulmonary disorders). IV antiviral therapy is recommended for immunocompromised children.
Bacterial superinfection; thrombocytopenia, arthritis, encephalitis, nephritis, Reye syndrome (with aspirin use).
Incubation period: 10-21 days
Causative agent: Varicella-zoster virus
Symptomatic. Prevent child from scratching. Keep fingernails short and clean. Sedation may be necessary. Use soothing lotions to allay itching. If secondary infections occur, antimicrobials may be given. Do not give aspirin because of high risk for Reye syndrome. Salicylate therapy should be stopped in a child who is exposed to varicella.
Diphtheria
In untreated persons, organisms can be present in discharges from the nose and throat and from eye and skin lesions for 2-6 wk after infection
Route: Droplets from respiratory tract of infected person or carrier; contact with discharges from skin lesions
Local and systemic manifestations. Membrane over tissue in nose or throat at site of bacterial invasion. Hoarse, brassy cough with stridor. Toxin from organism produces malaise and fever. Toxin has affinity for renal, nervous, and cardiac tissue.
A single dose (IV preferred) of equine antitoxin should be administered on the basis of clinical diagnosis, even before culture results are available (test for sensitivity to horse serum).
Local infections: low-grade fever with gradual onset. Serious complications include severe neck swelling (bull neck), upper airway obstruction, myocarditis, and peripheral neuropathies.
Incubation period: 2-7 days or longer
Causative agent: Corynebacterium diphtheriae
Antimicrobial therapy with erythromycin or penicillin G procaine is given for 14 days in addition to antitoxin. Strict bed rest. Prevent exertion. Cleansing throat gargles may be ordered. Liquid or soft diet. Gavage or parenteral administration of fluids may become necessary. Observe for respiratory obstruction.
Equipment for suctioning should be available. Oxygen and emergency tracheostomy may be necessary. Isolate.
Epidemic Influenza
Route: Airborne, droplet infection; direct contact
Manifestations in respiratory tract. Sudden onset with chills, fever, muscle pains, cough. If infection is severe and spreads to lower respiratory tract, air hunger may develop.
Symptomatic. Provide bed rest and increased fluid intake. Antimicrobials and sulfonamides may prevent secondary infection. Acetaminophen (antipyretic), drugs to control cough, and analgesics for pain may be given. Do not give aspirin because of high risk for Reye syndrome.
In severe cases, pulmonary edema and cardiac failure. Secondary invaders may produce bacterial infections of respiratory tract.
Incubation period: 1-4 days
Causative agent: Influenza virus types A, B, and C
Amantadine, rimantadine, Zanamivir, and oseltamivir (antiviral medication) are approved for treatment in children 1 yr of age and older, but different strains have developed some resistance.
Erythema Infectiosum (fifth disease)
Uncertain
Route: Droplet; infected persons
Three-stage rash: Erythema on face, mostly on cheeks (disappears in 1-4 days). One day after face rash, maculopapular red spots appear on upper and lower extremities, progressing proximal to distal; lacy appearance. Rash subsides but reappears if skin is irritated (sun, heat, cold); may last 1-3 wk.
Child not contagious after rash appears.
Reinforce benign nature of the condition to parents. No treatment indicated.
Aplastic crisis in children with sickle cell anemia.
Incubation period: 4-14 days or longer
Causative agent: Parvovirus B19
Exposed pregnant women should notify their obstetrician.
Avoid exposing immunosuppressed children and children with sickle cell disease.
Exanthema Subitum (Roseola)
Unknown
Route: Droplet; primarily affects children younger than 2 yr of age
Persistent high fever for 3-4 days in child who appears well. Precipitous drop in fever to normal with appearance of rash. Rash: discrete rose-pink macules appearing first on trunk, then spreading to neck, face, and extremities. Nonpruritic, fades on pressure, lasts 1-2 days.
Antipyretics to control fever. Anticonvulsants for child who has history of febrile seizures.
Febrile seizures during febrile period. Bulging fontanel.
Incubation period: 9-10 days
Causative agent: Human herpesvirus type 6
Teach parents measures for combating high temperature. Reinforce benign nature of illness.
Hepatitis Type A
1-2 weeks before onset of jaundice or elevation of liver enzymes
Route: Oral contamination by intestinal excretions; contaminated food, milk, or water
Hepatitis A is a major potential health problem in daycare centers
Manifestations occur rapidly and vary from mild to severe, from mild fever, anorexia, generalized malaise, nausea, vomiting, unpleasant taste in mouth, abdominal discomfort, and nonexistent or mild jaundice to severe jaundice, coma, and death. Early leukopenia is seen. Bile may be detected in urine; bowel movements are clay-colored. Liver function tests are useful for diagnosis.
Symptomatic. No specific therapy for uncomplicated HAV infection. Enteric precautions are necessary for 1 wk after onset of jaundice. Persons caring for those who are not toilet-trained, have diarrhea, or are incontinent should use disposable gloves when carrying fecal waste.
Usually benign in children.
Liver damage, recurrence of symptoms.
May be a source of chromosomal damage.
Incubation period: 15-50 days (average 28 days)
Causative agent: Hepatitis A virus (HAV)
Prevention: In daycare centers, practice thorough hand hygiene after changing diapers and before preparing and serving food. Because HAV may survive on objects in the environment for weeks (e.g., infant changing tables), adequate environmental hygiene is essential.
Children should be immunized at 1 yr of age (12-23 mos).
Administer immunoglobulin to contacts of affected child younger than 1 yr of age in a daycare setting.
Hepatitis Type B
Few days before to 1 mo or more after onset
Route: Person-to-person by percutaneous introduction of blood; direct contact with secretions or blood contaminated with HBV.
Routine preexposure immunization recommended for all infants; appropriate immunoprophylaxis of infants born to HBsAg-positive women and of infants born to women with unknown HBsAg status; some risk in children on hemodialysis, children receiving blood or blood products (including those with hemophilia), and IV drug users
Manifestations occur slowly. See hepatitis A for clinical manifestations.
Symptomatic. Children should be allowed to regulate own activity. Diet should be high-protein, high-calorie, high-carbohydrate, and low-fat. Food should be served in small, attractive, frequent feedings. Chief reasons for hospitalization are persistent vomiting and toxicity. Fluids may be given parenterally.
Acute fulminating hepatitis characterized by rapidly rising bilirubin, encephalopathy, edema, ascites, and hepatic coma.
Chronic HBV-infected persons are at risk for serious liver disease including primary hepatocellular carcinoma (HCC) with advancing age.
Incubation period: 45-160 days (average 90 days)
Causative agent: Hepatitis B virus (HBV)
Prevention: Universal immunization of infants and preteen children not immunized during infancy. Careful handling of blood and secretions; universal precautions.
No specific therapy for acute
HBV vaccine is available.
HBIG and corticosteroids are not effective.
Lyme Disease
Not communicable from person to person; persons with active disease should not donate blood
Begins with a skin lesion at the site of a recent tick bite. The painless red macule expands to form a large papule with a raised border and a clear center. Systemic manifestations include malaise, lethargy, fever, headache, arthralgias, stiff neck, myalgias, and lymphadenopathy. Late manifestations involve the joints and the cardiac and neurologic systems. Often first appears as single joint redness, swelling, and limitation.
Early treatment is doxycycline for children 8 yr of age and older. All ages: amoxicillin or cefuroxime. Later-stage disease is treated with high-dose IV ceftriaxone or penicillin. Prevention by teaching parents to observe for signs of disease during tick season. Protective clothing should be worn in areas where tick exposure is likely. Ticks should be removed.
Neurologic complications, carditis, and chronic arthritis may develop.
Incubation period: 1-32 days but up to months or years
Causative agent: Borrelia burgdorferi
Route: Spread by ticks; most common hosts are white-tailed deer and white-footed mice
Transplacental infection has resulted in fetal death, prematurity, and congenital anomalies.
Measles (Rubeola)
From 4 days before to 5 days after rash appears
Route: Direct contact; airborne by droplets and contaminated dust
Coryza, conjunctivitis, and photophobia are present before rash. Koplik spots in mouth, hacking cough, high fever, rash, and enlarged lymph nodes. Rash consists of small reddish brown or pink macules changing to papules; fades on pressure. Rash begins behind ears, on forehead or cheeks, progresses to extremities, and lasts about 5 days.
Symptomatic. Keep child in bed until fever and cough subside. Light in room should be dimmed. Keep hands from eyes. Irrigate eyes with physiologic saline solution to relieve itching. Tepid baths and soothing lotion relieve itching of skin. Encourage fluids during fever. Humidify the child’s room. Antimicrobial therapy given for complications.
Vary with severity of disease: otitis media, pneumonia, tracheobronchitis, nephritis. Encephalitis with permanent brain damage may occur. Death from respiratory and neurologic complications.
Incubation period: 8-12 days
Causative agent: RNA virus
Vitamin A supplementation is recommended once daily for 2 days to reduce mortality. Immunoglobulin (IG) can help prevent or modify measles within 6 days of exposure.
Subacute sclerosing panencephalitis (SSPE), a rare degenerative central nervous syndrome (CNS) disease, may occur. The mean incubation period is 7 yr after measles illness.
Measles, German (Rubella)
During prodromal period and for 5 days after appearance of rash
Route: Direct contact with secretions of nose and throat of infected person; airborne by contaminated dust particles
Fetus may contract rubella in utero if mother has the disease; slight fever, mild coryza. Rash consists of small pink or pale red macules closely grouped to appear as scarlet blush that fades on pressure. Rash fades in 3 days. Swelling of posterior cervical and occipital lymph nodes. No Koplik spots or photophobia as in measles.
Symptomatic. Bed rest until fever subsides. Children should be excluded from school or daycare for 7 days after onset of rash.
Infants with congenital rubella should be considered contagious until 1 yr of age unless cultures are repeatedly negative.
Chief danger of disease is damage to fetus if mother contracts infection during first trimester of pregnancy. Neonate may have congenital rubella syndrome with permanent defects (e.g., cataracts, cardiovascular anomalies, deafness, microcephaly, mental retardation). Virus can be isolated from blood, urine, throat, cerebrospinal fluid, lens, and other involved organs.
Incubation period: 14-23 days
Causative agent: Virus
Infants may shed virus for 12-18 mo.
Severe complications are rare. Encephalitis may occur.
Mumps (Infectious Parotitis)
1-2 days before swelling to 5 days after onset of swelling
Route: Direct or indirect contact with salivary secretions of infected person. Droplet
Salivary glands are chiefly affected. Parotid, sublingual, and submaxillary glands may be involved. Swelling and pain occur in these glands either unilaterally or bilaterally. Child may have difficulty swallowing, headache, fever, and malaise.
Local application of heat or cold to salivary glands to reduce discomfort. Liquids or soft foods are given. Foods containing acid may increase pain. Bed rest until swelling subsides. Children are excluded from school or daycare for 9 days from onset of parotid gland swelling. Mumps vaccine should be given at least 2 wk before or 3 mos after administration of IG or blood transfusion.
Complications are less frequent in children than in adults.
Incubation period: 16-18 days
Causative agent: Rubulavirus in the Paramyxoviridae family
Meningoencephalitis, inflammation of ovaries or testes, or deafness may occur.
Pertussis (Whooping Cough)
4-6 wk from onset
Route: Direct contact; airborne by droplet spread from infected person
Begins with symptoms of upper respiratory tract infection. Coryza, dry cough, which is worse at night. Cough occurs in paroxysms of several sharp coughs in one expiration, then a rapid deep inspiration, followed by a whoop. Dyspnea and fever may be present. Vomiting may occur after coughing. Lymphocytosis occurs.
Duration of illness is 6-10 wk.
Symptomatic. Azithromycin is the drug of choice for treatment or prophylaxis of pertussis in infants younger than 1 mo of age. Erythromycin may limit communicability. Protect child from secondary infection. Erythromycin for household and daycare contacts. Primary or booster vaccination of exposed children younger than 7 yr of age. Provide mental and physical rest to prevent paroxysms of coughing. Provide warm, humid air. Oxygen may be necessary. Avoid chilling. Offer small, frequent feedings to maintain nutritional status. Refeed if child vomits. Small amounts of sedatives may be given to quiet the child. Most infants younger than 6 mos of age are hospitalized; intensive care may be required.
Very serious disease during infancy because of complication of bronchopneumonia.
Otitis media, marasmus, bronchiectasis, and atelectasis may occur.
Hemorrhage may occur during paroxysms of coughing. Encephalitis may occur.
Incubation period: 7-10 days
Causative agent: Bordetella pertussis
Poliovirus Infection (Poliomyelitis)
During period of infection, latter part of incubation period, and first week of acute illness
Route: Oral contamination by pharyngeal and intestinal excretions, respiratory route
Acute illness. Initial symptoms of upper respiratory tract infection, headache, fever, vomiting.
Both parents and child need support and reassurance, for they are fearful of the term polio. Treatment and nursing care are symptomatic. Because oral polio vaccine is no longer available in the United States, the chance for exposure to vaccine-type polio is remote.
Emotional disturbances, gastric dilation, melena, hypertension, or transitory paralysis of bladder may occur.
Incubation period: 3-6 days
Causative agent: Enteroviruses
Nonparalytic: Previous symptoms plus sore or stiff muscles of neck, trunk, and extremities. Nuchal rigidity.
Severe complications of paralytic polio include respiratory failure and permanent muscle deficits.
Paralytic: Includes muscular paralysis. Clinical manifestations may vary from mild to very severe following symptomless period after initial symptoms.
Rotavirus
Route: Fecal-oral
Acute onset of fever and vomiting followed 24-48 hr later by watery diarrhea.
Oral or parenteral fluids and electrolytes are given to prevent and correct dehydration.
No antiviral therapy is available.
Contact precautions are used when diapering or cleaning incontinent children during illness.
Dehydration, electrolyte abnormalities, and acidosis.
Incubation period: 1-3 days
Causative agent: Rotovirus
Smallpox (Variola)
Persons are not infectious during the incubation period or febrile prodrome but become infectious with the onset of mucosal lesions, which occur within hours of the rash; the first week of rash illness is the most infectious period, although individuals remain infectious until all scabs have separated
Route: Droplets (from the oropharynx of infected individuals); may be transmitted from aerosol and direct contact with infected lesions, clothing, or bedding
Severe prodromal illness with high fever (generally 102° F-104° F [38.9° C-40° C]), malaise, severe headache, backache, abdominal pain, and prostration (exhaustion), lasting for 2-5 days. May include vomiting and seizures. Prodromal period is followed by lesions on the mucosa of the mouth or pharynx that last less than 24 hr before the onset of rash. The child is considered infectious once the lesions appear. The rash begins on the face and spreads rapidly to the forearms, trunk, and legs in a centrifugal distribution. Many have lesions on the palms and soles After 8-10 days, lesions begin to crust. Once all lesions have separated (3-4 wk), the child is no longer infectious.
Treatment is supportive. Vaccinia immune globulin (VIG) is used for certain complications of immunizations and has no role in treatment of smallpox. The vaccination may provide some protection against the disease if administered within 3-4 days of exposure. Children are isolated in a private, airborne infection isolation room with negative pressure ventilation. Anyone entering the room must wear an N95 or higher-quality respirator, gloves, and gown even if there is a history of recent successful immunization. If thechild leaves the room, he or she should wear a mask and be covered with sheets or gowns to decrease the risk for possible transmission.
Fatality rates reached 30% in the past; death occurred during the second week of illness from overwhelming viremia. The potential for modern supportive therapy in improving outcome is not known.
Incubation period: 7-17 days
Causative agent: Virus (variola)
Note: A smallpox vaccination plan has been implemented in the United States; however, the plan does not currently include immunization of children.
Cidofovir has been suggested as having a role in smallpox therapy, but no data are available.
Streptococcal Infection, Group A Beta Hemolytic (Streptococcal Sore Throat, Scarlet Fever, Scarlatina)
Onset to recovery
Initial symptoms of streptococcal sore throat are seen in the pharynx. The source of this organism may also be in a burn or wound. Toxin from site of infection is absorbed into bloodstream. Typical symptoms of scarlet fever are headache, fever, rapid pulse, rash, thirst, vomiting, lymphadenitis, and delirium. Throat is injected, and cellulitis of throat occurs. White tongue coating desquamates, and red strawberry tongue results. Other manifestations may include otitis media, mastoiditis, and meningitis.
Penicillin G is the drug of choice. Erythromycin is used for penicillin-sensitive individuals. Adequate fluid intake, bed rest, pain-relieving drugs, and mouth care are important. Diet should be given as the child wishes: liquid, soft, or regular. Warm saline throat irrigations may be given to the older child. Increased humidity for severe infection of upper respiratory tract. Cold or hot applications to painful cervical lymph nodes.
Complications are caused by toxins, the streptococci, or secondary infection. Complications of pneumonia, glomerulonephritis, or rheumatic fever may occur.
Route: Droplet infection; direct and indirect transmission may occur
Incubation period:2-5 days
Causative agent:Betahemolyticstreptococci,Group A strains
Tetanus
Route: Wound contaminant; umbilical stump contamination in neonates
Early signs are headache, restlessness, followed by spasm of masticatory muscles (chewing), difficulty opening the mouth, dysphagia. Progresses to opisthotonos (severe arching of back and head bending to back), seizures.
Human tetanus immune globulin is given to neutralize neurotoxins to stop the infectious process.
Surgical wound debridement
Quiet environment as muscle spasms are aggravated by external stimuli.
Metronidazole is the drug of choice for 10-14 days; an alternative is Penicillin G, IV.
Diazepam (Valium) to alleviate muscle spasms
Respiratory failure requiring support. Seizures.
Incubation period: 3-21 days (average 8 days)
Causative agent:Clostridium tetani![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Communicable Diseases
Get Clinical Tree app for offline access
