Chapter 3 Common Health Problems of Older Adults
Safe and Effective Care Environment
1. Recognize the benefits of interdisciplinary health care team collaboration in the care of older adults.
2. Identify risk factors for falls and driving ability in older adults who live in the community or are hospitalized.
3. Explain falls risk and prevention interventions for older adults in the hospital and community.
4. Describe best practices to promote patient safety when using restraints.
Health Promotion and Maintenance
5. Teach selected evidence-based lifestyle practices to promote healthy activities in older adults.
6. Conduct a medication assessment for potential risks for adverse drug events in older adults.
8. Assess the older patient’s risk for and signs of neglect and abuse.
9. Use valid and reliable tools to assess for mental/behavioral health problems in the older adult.
10. Compare characteristics of depression, delirium, and dementia.
11. Develop a plan of care to assist the older adult to cope with relocation stress syndrome.
12. Identify four subgroups of older adults.
13. Explain factors that contribute to nutrition-related problems among older adults in the community and inpatient facilities.
14. Describe the effects of drugs on the older adult.
15. Assess for adverse drug effects of psychoactive drugs when taken by older adults.
http://evolve.elsevier.com/Iggy/
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Review Questions for the NCLEX® Examination
Overview
Late adulthood can be divided into four subgroups:
• 65 to 74 years of age: the young old
• 75 to 84 years of age: the middle old
• 85 to 99 years of age: the old old
The fastest growing subgroup is the old old, sometimes referred to as the advanced older adult population. Members of this subgroup are sometimes referred to as the “frail elderly,” although a number of 85 to 95 year olds are very healthy and do not meet the criteria for being frail. Frailty is a clinical syndrome in which the older adult has unintentional weight loss, weakness and exhaustion, and slowed physical activity, including walking. Frail older adults are also at high risk for adverse outcomes (Rocchiccioli & Sanford, 2009).
The number of homeless people older than 60 years is also growing. The inability to pay for housing and family/partner relationship problems are primary factors that contribute to this trend. Most homeless adults have one or more chronic health problems, including mental/behavioral health disorders. Chapter 4 discusses issues related to the homeless population in more detail.
Health Issues for Older Adults in Community-Based Settings
Like younger and middle-aged adults, older adults need to practice health promotion and illness prevention to maintain or achieve a high level of wellness. Teach them the importance of promoting wellness and strategies for meeting this outcome (Chart 3-1).
Chart 3-1 Patient and Family Education
Preparing for Self-Management: Lifestyles and Practices to Promote Wellness
Health-Protecting Behaviors
• Have yearly influenza vaccinations (after October 1).
• Obtain a pneumococcal vaccination. (A routine revaccination may be necessary.)
• Have a tetanus immunization, and get a booster every 10 years.
• Wear seat belts when you are in an automobile.
• Use alcohol in moderation or not at all.
• Avoid smoking; if you do smoke, do not smoke in bed.
• Install and maintain working smoke detectors and/or sprinklers.
• Create a hazard-free environment to prevent falls; eliminate hazards such as scatter rugs and waxed floors.
• Use medications, herbs, and nutritional supplements according to your health care provider’s prescription.
• Avoid over-the-counter medications unless your physician directs you to use them.
Health-Enhancing Behaviors
• Have a yearly physical examination; see your health care provider more often if health problems occur.
• Reduce dietary fat to not more than 30% of calories; saturated fat should provide less than 10% of your calories.
• Increase your dietary intake of complex carbohydrate and fiber-containing food to five or more servings of fruits and vegetables and six or more servings of grain products daily.
• Increase calcium intake to between 1000 and 1500 mg daily; take a vitamin D supplement every day if not exposed daily to sunlight.
• Allow at least 10 to 15 minutes of sun exposure two or three times weekly for vitamin D intake; avoid prolonged sun exposure.
• Exercise regularly three to five times a week.
• Manage stress through coping mechanisms that have been successful in the past.
• Get together with people in different settings to socialize.
• Reminisce about your life through reflective discussions or journaling.
Common health issues and problems that often affect older adults in the community include:
• Decreased nutrition and hydration
• Mental health/behavioral health problems (including substance abuse)
Decreased Nutrition and Hydration
Inadequate nutrition may also be related to loneliness. Older adults may respond to loneliness, depression, and boredom by not eating, which can lead to under-nutrition. Many who live alone lose the incentive to prepare or eat balanced diets, especially if they do not “feel well.” Men who live at home alone are especially at risk for not eating enough calories to maintain their weight. Other factors associated with under-eating include being hospitalized before starting home health care, having a primary care provider who is not a female family member, and having a low level of education (Volkert et al., 2010).
Action Alert
Perform nutritional screening for older adults in the community who are at risk for inadequate nutrition—either under-nutrition or obesity. Ask the individual about unintentional weight loss or gain, eating habits, appetite, prescribed and over-the-counter drugs, and current health problems. Determine contributing factors for older adults who have or are at risk for poor nutrition, such as transportation issues or loneliness. Based on these data, develop and implement a plan of care in collaboration with appropriate members of the health care team. Chapter 63 describes nutritional assessment and management of nutrition problems in detail.
Some older adults are at risk for geriatric failure to thrive (GFTT)—a complex syndrome including under-nutrition, impaired physical functioning, depression, and cognitive impairment (Rocchiccioli & Sanford, 2009). However, drug therapy, chronic diseases, major losses, and poor socioeconomic status can cause these same health problems. Be sure to consider these factors when screening for GFTT. For those at risk for or who have GFTT, collaborate with the older adult and family to plan referral to his or her primary care provider for extensive evaluation. Early supportive intervention can help prevent advanced levels of deterioration.
Action Alert
Incontinence may actually increase because the urine becomes more concentrated and irritating to the bladder and urinary sphincter. Teach older adults the importance of drinking 6 to 8 glasses of water a day plus other fluids as desired. Remind them to avoid excessive caffeine and alcohol because they can cause dehydration. Chapter 13 discusses fluid and electrolyte imbalances in detail.
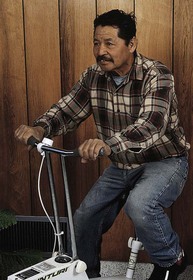
Decreased Mobility
Exercise and activity are important for older adults as a means of promoting and maintaining health (Fig. 3-1). Physical activity can help keep the body in shape and maintain an optimal level of functioning. Regular exercise has many benefits for older adults in community-based settings. The advantages of maintaining appropriate levels of physical activity include:
• Increased muscle strength and balance
• Reduced or maintained weight
• Improved sense of well-being and self-esteem
• Decreased depression symptoms
• Reduced risks for diabetes, coronary artery disease, and dementia
A study by Weeks et al. (2008) found that past life experience, life transitions, and future health concerns affect the participation of older adults in physical activity. For example, women who worked outside the home and/or reared multiple children stated that they did not have the time or energy to exercise when they were young. Others thought that their current health status prevented them from engaging in exercise. Some older adults worried that increasing their activity level might increase their risk for hip fracture or arthritis.
Weeks et al. (2008) also found that when compared with seniors living independently, nursing home residents had a very low level of physical activity. The researchers suggested that nursing home staff members need to be trained in how to promote resident exercise at least twice a week. Nurses who work in nursing homes must collaborate with physical and occupational therapists to plan this training and implement a regular exercise program.
Swimming is also recommended but does not offer the weight-bearing advantage of walking. Weight bearing helps build bone, an especially important advantage for older women to prevent osteoporosis (see Chapter 53). Teach older adults who have been sedentary to start their exercise programs slowly and gradually increase the frequency and duration of activity over time, under the direction of their health care provider.
Health Promotion and Maintenance
Stress and Loss
• Rapid environmental changes that require immediate reaction
• Changes in lifestyle resulting from retirement or physical incapacity
Fortunately, most older adults are relatively healthy and live in and own their own homes. Physical and/or mental health problems may force some to relocate to a retirement center or an assisted-living facility, although these facilities can be very expensive. Others move in with family members or apartment buildings funded and designated for seniors. Older adults usually have more difficulty adjusting to major change when compared with younger and middle-aged adults. Being admitted to a hospital or nursing home is a particularly traumatic experience. Older adults often suffer from relocation stress syndrome, also known as relocation trauma. Relocation stress syndrome is the physical and emotional distress that occurs after the person moves from one setting to another. Examples of physiologic behaviors are sleep disturbance and increased physical symptoms, such as GI distress. Examples of emotional manifestations are withdrawal, anxiety, anger, and depression. Chart 3-2 lists nursing interventions that may help decrease the effects of relocation.
Chart 3-2 Best Practice for Patient Safety & Quality Care
Minimizing the Effects of Relocation Stress in Older Adults
• Provide opportunities for the patient to assist in decision making.
• Carefully explain all procedures and routines to the patient before they occur.
• Ask the family or significant other to provide familiar or special keepsakes to keep at the patient’s bedside (e.g., family picture, favorite hairbrush).
• Reorient the patient frequently to his or her location.
• Ask the patient about his or her expectations during hospitalization or assisted-living or nursing home stay.
• Encourage the patient’s family and friends to visit often.
• Establish a trusting relationship with the patient as early as possible.
• Assess the patient’s usual lifestyle and daily activities, including food likes and dislikes and preferred time for bathing.
• Avoid unnecessary room changes.
• If possible, have a family member, significant other, staff member, or volunteer accompany the patient when leaving the unit for special procedures or therapies.
Accidents
Fall Prevention
Once an older person has been identified as being at high risk for falls, choose interventions that help prevent falls and possible serious injury. For those in the community, tai chi exercise is very helpful to improve balance and functional mobility, as well as to decrease the fear of falling, especially among older women (Wooten, 2010). Tai chi is described in Chapter 2.
Driving Safety
Physicians and other health care professionals play a major role in identifying driver safety issues. Yet, many are reluctant to intervene because older patients feel they will lose their independence if they cannot drive. They may also be angry and resistant to the idea of giving up perhaps their only means of transportation. As an alternative, health care professionals can recommend driving refresher courses and suggest that high-risk driving conditions, like wet roads, be avoided. Newer vehicles have some safety features to help older adults, such as large-print digital readouts for speed and other data. Chart 3-3 lists additional ways to improve older adult driver safety.
Chart 3-3 Best Practice for Patient Safety & Quality Care
Recommendations for Improving Older Driver Safety
• Discuss driving ability with the patient to assess his or her perception.
• Assess physical and mental deficits that could affect driving ability.
• Consult with appropriate health care providers to treat health problems that could interfere with driving.
• Suggest community-based transportation options, if available, instead of driving.
• Discuss driving concerns with patients and their families.
• Remind the patient to wear glasses and hearing aids, if prescribed.
• Encourage driver refresher classes, often offered by AARP (formerly the American Association of Retired Persons).
• Consult a certified driving specialist for an on-road driving assessment.
• Encourage avoiding high-risk driving locations or conditions, such as busy urban interstates and wet or icy weather conditions.
• Report unsafe drivers to the state department of motor vehicles if they continue to drive.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree