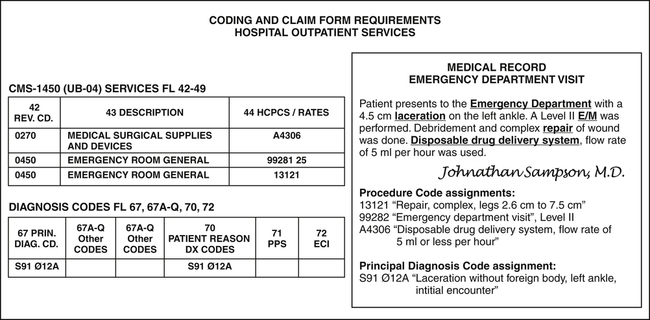
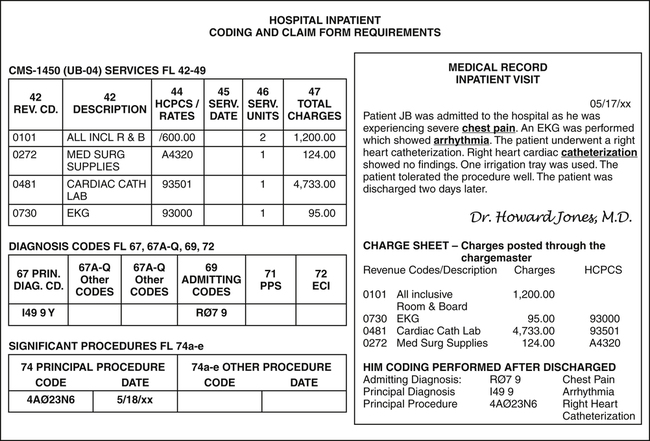
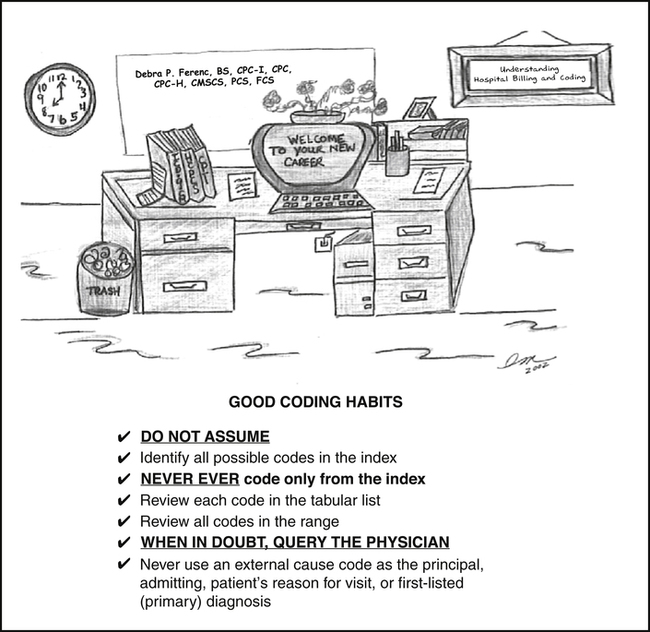
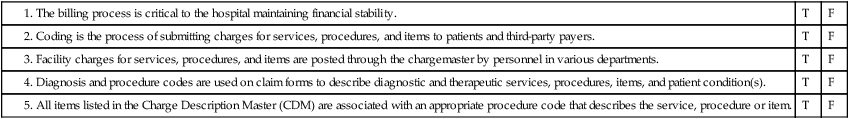
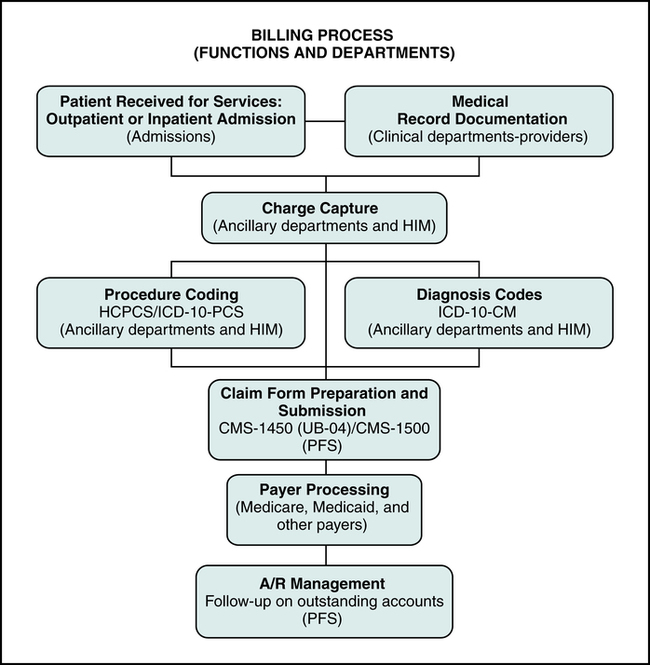
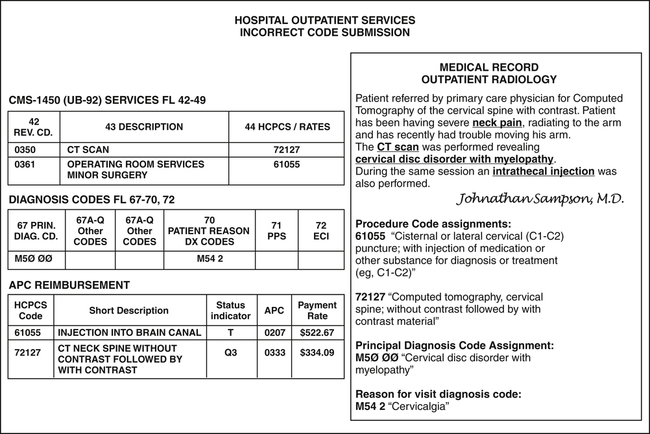
Chapter 9 1. Define terms, phrases, abbreviations, and acronyms. 2. Explain the relationship between billing and coding. 3. Discuss variations in coding systems used for outpatient and inpatient services. 4. Identify standard code sets required under HIPAA regulations. 5. Demonstrate an understanding of HCPCS and ICD-10 coding principles and guidelines. 6. Provide an outline of the basic steps to coding from the medical record. 7. Demonstrate the ability to apply coding guidelines for outpatient and inpatient cases. American Health Information Management Association Ambulatory Payment Classifications Centers for Disease Control and Prevention Charge Description Master or chargemaster Current Procedural Terminology Centers for Medicare and Medicaid Services Emergency Medical Treatment and Labor Act Healthcare Common Procedure Coding System International Classification of Diseases, 10th Revision, Clinical Modification International Classification of Diseases, 10th Revision, Procedure Coding System Inpatient Prospective Payment System Medicare Severity-Diagnosis Related Groups National Correct Coding Initiative National Center for Health Statistics Medicare Outpatient Code Editor Outpatient Prospective Payment System Resource-Based Relative Value Scale Coding principles and guidelines vary by provider, category of service, and payer type. The challenge for hospital coding and billing professionals is to understand those variations and effectively apply guidelines applicable to coding hospital services. Hospital coding and billing professionals must also understand the relationship between billing and coding. This relationship is significant because coding describes diagnostic and therapeutic services provided and medical conditions that explain why services were provided. Concepts on documentation, coding, claim forms, and the billing process were covered in previous chapters. This chapter will provide a brief review of those concepts, demonstrating the relationship between coding and billing. The chapter will then explore diagnosis and procedure coding guidelines and their appropriate application. The basic steps to coding conditions and procedures using ICD-10-CM, HCPCS and ICD-10-PCS will be revisited to assist with the application of coding guidelines using case scenarios. Each function in the process can be thought of as an individual step contributing to the completion of patient statements and claim forms. The function of coding is integral to the billing process. The relationship between coding and billing is simply that coding is required to bill for services rendered. Codes are used on claim forms to describe diagnostic and therapeutic services, procedures, items, and medical conditions documented in the patient’s medical record. A diagnosis code(s) should explain the medical necessity for the service or procedure. The relationship between coding and billing is illustrated in Figure 9-1, which highlights functions of the billing process and the departments responsible for performing those functions. Third-party payer claim processing includes a detailed review of claim form data to identify issues with the claim. Payment determination is performed after the claim is reviewed and an explanation of the determination is sent to the provider. The claim may be paid, denied, or the claim may be placed in “pending” status until additional information is obtained. It is essential for hospital billing and coding professionals to understand phases of payer processing and payer edits to ensure accurate coding and billing of hospital services. Figure 9-2 illustrates phases of third-party payer claim processing. The Medicare Outpatient Code Editor (OCE) is a computerized program designed to check outpatient claim data to identify problems related to services billed, such as coding errors or issues involving medical necessity. OCE incorporates the National Correct Coding Initiative (NCCI) and other Medicare edits. All outpatient claims are processed through the OCE as required by the Centers for Medicare and Medicaid Services (CMS). The OCE includes edits related to HCPCS Level I and Level II Codes. The OCE contains edits used to identify coding, coverage, clinical, and other claim issues as illustrated in Figure 9-3. The Medicare Code Editor (MCE) is a computerized program that incorporates various Medicare edits designed to check inpatient claim data to identify problems related to services billed, such as coding errors or issues involving medical necessity. All inpatient claims are processed through the MCE as required by the Centers for Medicare and Medicaid Services (CMS). The MCE includes inpatient coding edits, coverage edits, and clinical edits. National Correct Coding Initiative (NCCI) and Medically Unlikely Edits (MUE) are also incorporated into the MCE. Examples of edits included in the MCE are illustrated in Figure 9-3. The National Correct Coding Initiative (NCCI) includes edits that provide explanation of coding situations that may be inappropriate and they are built into many billing software programs. NCCI edits are published quarterly and applied based on the date of service. They can be obtained in manual format or they can be incorporated into some billing programs to ensure appropriate usage of codes and guidelines. Examples of NCCI edits are outlined in Figure 9-4. Medically Unlikely Edits (MUE) were developed by CMS and implemented in 2007 to identify maximum units of service that can be reported for a particular HCPCS Level I CPT or Level II Medicare National code on the same date of service, by the same provider, for the same patient. Medically Unlikely Edits (MUE) were not made public initially. However, CMS later announced that the majority of existing MUE would be made public. CMS publishes MUE on the Medicare Web site at http://www.cms.hhs.gov/NationalCorrectCodInitEd/08_MUE.asp#TopOfPage. Medicare further states that due to concerns regarding fraud and abuse, MUE with values of 4 or more will not be made public. Examples of MUE are illustrated in Figure 9-4. Submission of procedure or diagnosis codes that are incorrect will result in incorrect reimbursement, as illustrated in Figure 9-5. The APC payment rate for the injection procedure code 61055, is $522.67. The APC payment rate for the CT scan, without contrast followed by with contrast, procedure code 72127 is $334.09. The total reimbursement for this case is $856.76. If the claim was submitted with procedure code 72125, CT scan without contrast, the APC payment rate is $192.06, and the total reimbursement would be drastically reduced to $714.73. The first step to accurate coding is to understand what coding system is required for submission of charges to various payers. Coding system requirements and guidelines vary by payer and by category of service: outpatient, non-patient and inpatient, as illustrated in Figure 9-6. This section will explore examples of coding system variations for outpatient and inpatient services to provide a basic understanding of the reporting requirements for each service category. Coding system requirements for outpatient and non-patient services are outlined in Figure 9-6. Hospital outpatient facility charges are submitted for services provided by various departments within the hospital. Outpatient services include ambulatory surgery, emergency room, observation, radiology, and pathology/laboratory. These facility charges are generally reported on the CMS-1450 (UB-04). The coding systems used are HCPCS Level I CPT and Level II Medicare National Procedure Codes. ICD-10-CM diagnosis codes are used to report patient conditions in FL 67, 67A-Q, 70, and 72. An example of outpatient coding and claim form reporting is illustrated in Figure 9-7. Coding and claim form requirements for hospital inpatient services are outlined in Figure 9-6. Hospitals submit facility charges for inpatient services on the CMS-1450 (UB-04). The services are posted through the chargemaster by various hospital departments including the Health Information Management (HIM) Department. Each item in the chargemaster is associated with an HCPCS code. HCPCS codes are not always required in FL 44 for inpatient claims; however, they are printed on the detailed itemized statement. ICD-10-CM diagnosis codes are used to report the principal diagnosis, other diagnoses, admitting diagnosis, and external cause of injury in FL 67, 67A-Q, 69, and 72. Significant procedures performed during the visit are reported using ICD-10-PCS codes and they are reported in FL 74a-e. An example of coding systems and claim form requirements for hospital inpatient services is illustrated in Figure 9-8. To ensure accurate and effective coding, coders should develop good coding habits such as “NEVER code from the index” and “IF IT IS NOT DOCUMENTED, DO NOT CODE.” A coder must be consistent in the process he or she follows to assign a code, and a coder must follow those good coding habits in every coding situation (Figure 9-9). • Section I: ICD-10-CM Conventions, General Coding Guidelines, and Chapter-Specific Guidelines • Section II: Selection of Principal Diagnosis • Section III: Reporting Additional Diagnoses • Section IV: Diagnostic Coding and Reporting Guidelines for Outpatient Services
Coding Guidelines and Applications (HCPCS, ICD-10-PCS, and ICD-10-CM)
Relationship Between Billing and Coding
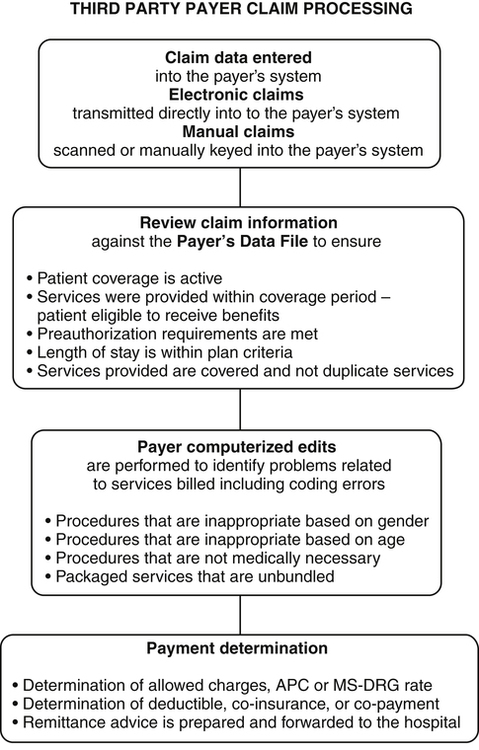
Payer Processing
Payer Edits
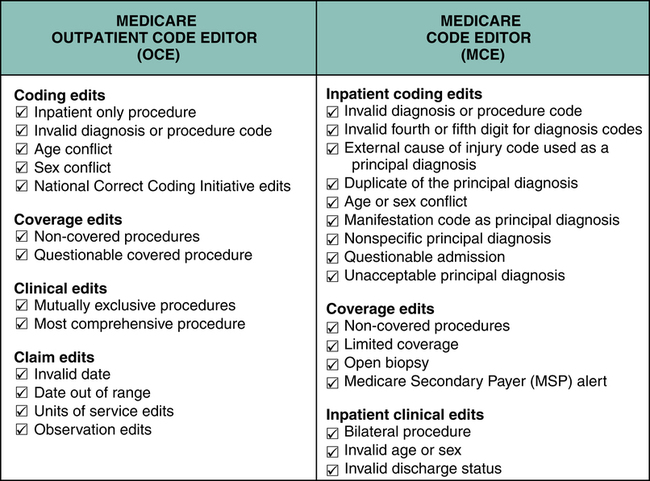
Outpatient Code Editor (OCE)
Medicare Code Editor (MCE)
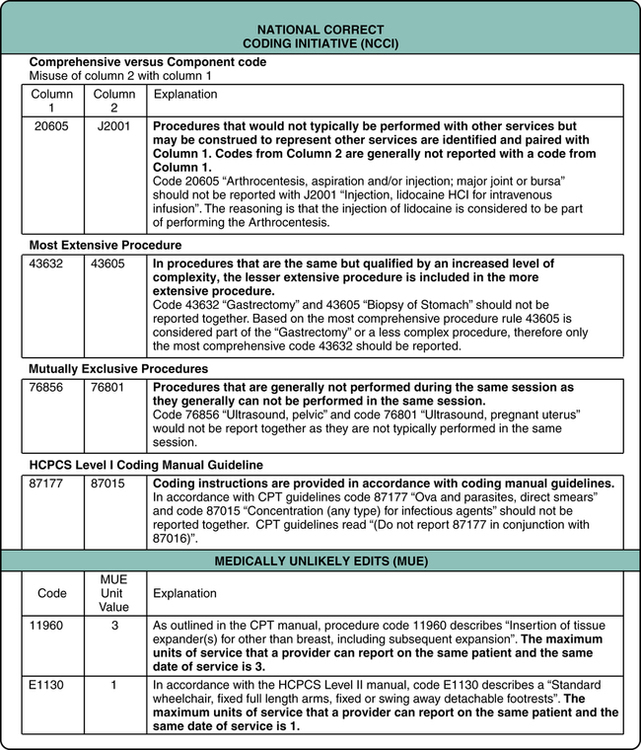
National Correct Coding Initiative (NCCI)
Medically Unlikely Edits (MUE)
Payment Determination
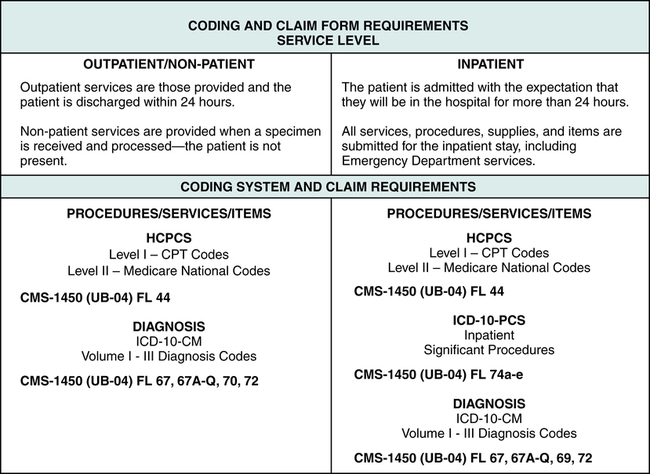
Coding System Variations
Outpatient and Non-patient Services
Inpatient Services
ICD-10-CM Official Diagnosis Coding Guidelines
ICD-10-CM General Diagnosis Coding Guidelines
Level of Detail in ICD-10-CM Coding
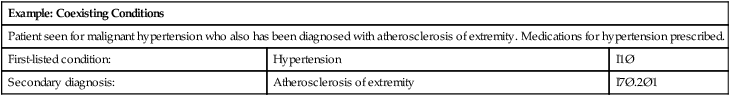
ICD-10-CM CHAPTER 9: DISEASES OF THE CIRCULATORY SYSTEM
I1Ø
Essential (primary) hypertension
I7Ø
Atherosclerosis
I7Ø.Ø
Atherosclerosis of aorta
I7Ø.1
Atherosclerosis of renal artery
I7Ø.2
Atherosclerosis of native arteries of the extremities
17Ø.2Ø
Unspecified atherosclerosis of native arteries of extremities
I7Ø.2Ø1
Unspecified atherosclerosis of native arteries of extremities, right leg
I7Ø.2Ø2
Unspecified atherosclerosis of native arteries of extremities, left leg
I7Ø.2Ø3
Unspecified atherosclerosis of native arteries of extremities, bilateral legs
I7Ø.2Ø8
Unspecified atherosclerosis of native arteries of extremities, other extremity
I7Ø.2Ø9
Unspecified atherosclerosis of native arteries of extremities, unspecified extremity
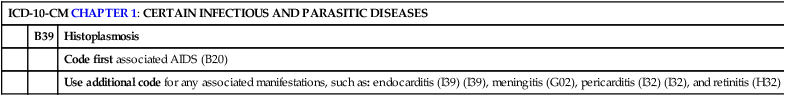
Multiple Coding for a Single Condition
ICD-10-CM CHAPTER 1: CERTAIN INFECTIOUS AND PARASITIC DISEASES
B39
Histoplasmosis
Code first associated AIDS (B20)
Use additional code for any associated manifestations, such as: endocarditis (I39) (I39), meningitis (G02), pericarditis (I32) (I32), and retinitis (H32)
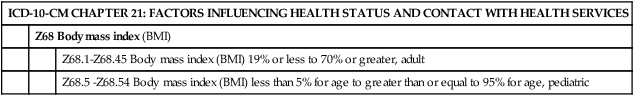
Documentation for Body Mass Index (BMI)
ICD-10-CM CHAPTER 21: FACTORS INFLUENCING HEALTH STATUS AND CONTACT WITH HEALTH SERVICES
Z68 Body mass index (BMI)
Z68.1-Z68.45 Body mass index (BMI) 19% or less to 70% or greater, adult
Z68.5 -Z68.54 Body mass index (BMI) less than 5% for age to greater than or equal to 95% for age, pediatric
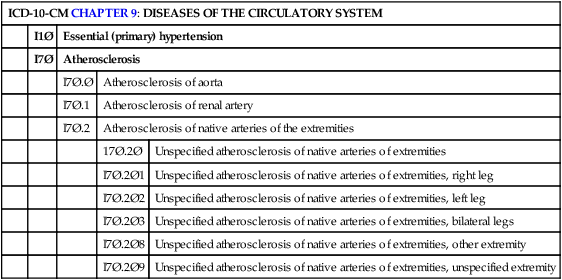
ICD-10-CM Outpatient Diagnosis Coding Guidelines
Identify and Code the First-Listed Condition
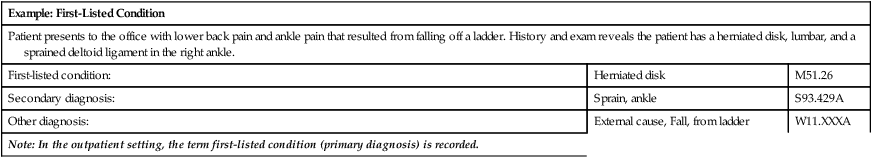
Example: First-Listed Condition
Patient presents to the office with lower back pain and ankle pain that resulted from falling off a ladder. History and exam reveals the patient has a herniated disk, lumbar, and a sprained deltoid ligament in the right ankle.
First-listed condition:
Herniated disk
M51.26
Secondary diagnosis:
Sprain, ankle
S93.429A
Other diagnosis:
External cause, Fall, from ladder
W11.XXXA
Note: In the outpatient setting, the term first-listed condition (primary diagnosis) is recorded.
Uncertain Diagnoses
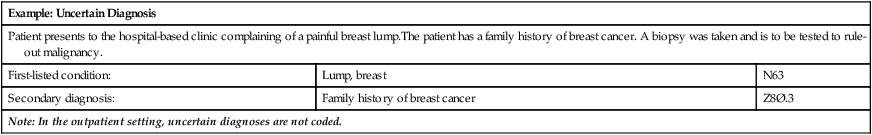
Example: Uncertain Diagnosis
Patient presents to the hospital-based clinic complaining of a painful breast lump.The patient has a family history of breast cancer. A biopsy was taken and is to be tested to rule-out malignancy.
First-listed condition:
Lump, breast
N63
Secondary diagnosis:
Family history of breast cancer
Z8Ø.3
Note: In the outpatient setting, uncertain diagnoses are not coded.
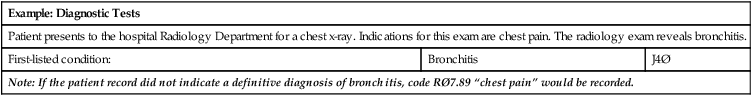
Diagnostic Tests
Example: Diagnostic Tests
Patient presents to the hospital Radiology Department for a chest x-ray. Indications for this exam are chest pain. The radiology exam reveals bronchitis.
First-listed condition:
Bronchitis
J4Ø
Note: If the patient record did not indicate a definitive diagnosis of bronchitis, code RØ7.89 “chest pain” would be recorded.
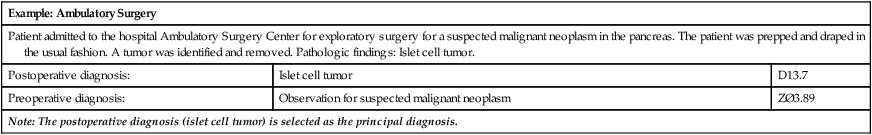
Ambulatory Surgery
Example: Ambulatory Surgery
Patient admitted to the hospital Ambulatory Surgery Center for exploratory surgery for a suspected malignant neoplasm in the pancreas. The patient was prepped and draped in the usual fashion. A tumor was identified and removed. Pathologic findings: Islet cell tumor.
Postoperative diagnosis:
Islet cell tumor
D13.7
Preoperative diagnosis:
Observation for suspected malignant neoplasm
ZØ3.89
Note: The postoperative diagnosis (islet cell tumor) is selected as the principal diagnosis.
Selection of the Principal Diagnosis
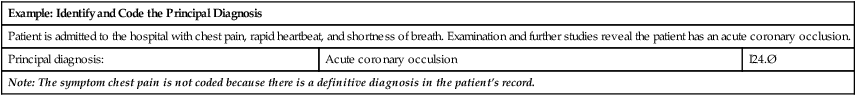
Identify and Code the Principal Diagnosis
Example: Identify and Code the Principal Diagnosis
Patient is admitted to the hospital with chest pain, rapid heartbeat, and shortness of breath. Examination and further studies reveal the patient has an acute coronary occlusion.
Principal diagnosis:
Acute coronary occulsion
I24.Ø
Note: The symptom chest pain is not coded because there is a definitive diagnosis in the patient’s record.
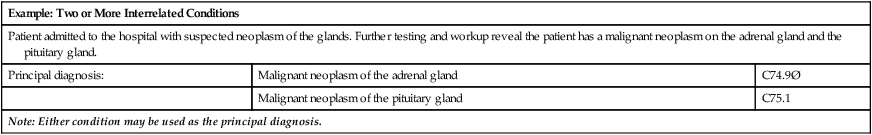
Two or More Interrelated Conditions
Example: Two or More Interrelated Conditions
Patient admitted to the hospital with suspected neoplasm of the glands. Further testing and workup reveal the patient has a malignant neoplasm on the adrenal gland and the pituitary gland.
Principal diagnosis:
Malignant neoplasm of the adrenal gland
C74.9Ø
Malignant neoplasm of the pituitary gland
C75.1
Note: Either condition may be used as the principal diagnosis.
Two or More Comparative or Contrasting Conditions
Example: Two or More Comparative or Contrasting Conditions
Patient is admitted with nausea, vomiting, and recurrent abdominal pain. Patient has a history of diverticula. The admitting physician documented the patient’s diagnosis as cholecystitis or diverticulitis of the small intestine. Patient scheduled for abdominal series and a gallbladder scan tomorrow.
Principal diagnosis:
Cholecystitis
K81.Ø
Diverticulitis
K57.12
Note: Either condition may be used as the principal diagnosis because the physician stated “cholecystitis or diverticulitis.” ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree