23 Clinical Informatics
Pearls
• Clinical information technology (IT) involves a dynamic set of interactions that all have to be managed effectively. The categories of people, process, and technology each introduce different challenges and factors that must be addressed for successful IT implementation and adoption.
• To achieve maximal beneficial effects, clinical IT must provide clinicians with the right amount of data in the appropriate context to help them make good clinical decisions.
• The use of IT to enforce compliance and adherence to policies and regulations must be balanced with clinical utility and minimal distractions.
• Effective use of clinical IT tools can markedly improve patient safety and clinical workflow.
• Clinical, administrative, and IT leaders need to develop a shared vision and governance model to deploy and maintain clinical IT systems.
Introduction
In the past decade, many examples of error, waste, and inefficiency in healthcare have been identified. In 1999, the Institute of Medicine (IOM) estimated that nearly 100,000 hospitalized patients die each year from medical errors.12 The IOM report led to increased scrutiny of the safety and efficiency of the healthcare system. In 2003, the analysis by McGlynn and others9 documented a significant gap between the care that patients need and the care that is provided. In a sample of more than 6700 adult patients in 12 metropolitan cities, only 54.9% of patients received the recommended care.9
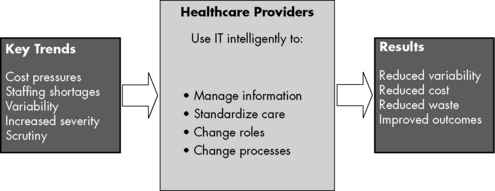
IT is a potential tool to reduce errors. A reduction in errors can result from the role of IT in managing information, its utility in standardizing care, and through its role as a vehicle to change roles and processes in an effort to reduce cost, variability, and waste. These efforts can result in improved outcomes (Fig. 23-1)
Implemention of clinical information systems
In another case, in the first 5 months following implementation of a commercially purchased CPOE system in a pediatric critical care unit at a leading children’s hospital in the northeast, mortality during interfacility patient transfer more than doubled (from 2.8% to 6.6%) when compared with the mortality in the 13 months preceding CPOE implementation.3 Several factors may have contributed to this rise. First, the system was rapidly deployed. Second, the clinical care team was not allowed to enter orders until the patient physically entered the hospital. Third, order sets were not developed to help clinicians rapidly enter common orders. Fourth, simultaneous with the CPOE implementation, the hospital dispensing process for medications was changed. All of these factors directly affected patient care.
A second children’s hospital in the northwest installed the same commercial CPOE system. When the effects of the implementation system on the northwest children’s hospital was studied by Del Beccaro and others,2 they found no difference in mortality in the preimplementation and postimplementation periods.
The Agency for Healthcare Research and Quality (AHRQ) calls for careful and thoughtful implementation of CPOE systems. Koppel’s study of CPOE systems, funded by the AHRQ,7 found two key problem areas in implementation:
• Fragmentation of data among each hospital’s various information systems
• Interface problems between people and machines, particularly when the computer forced people to work in a way that differed from clinical work routines
People, Process, and Technology
Different units in the same hospital will have drastically different acceptance of the same technology as the result of differences in staff perceptions regarding the ease of technology use and also the result of differences in staff attitudes about changes in their practice. Gender and age play important roles in determining these perceptions and attitudes. Karsh4 found that male users valued the usefulness of a tool, whereas female users felt that ease of use was more valuable. Older users focused more on social and process issues, whereas younger users focused more on the effects of the tool on task performance. Therefore before implementing any new technology, planners should evaluate characteristics of potential users and of the potential technology itself.