1 Children Are Different
Pearls
• Children are not “little adults.” They are physically, physiologically, and emotionally immature. Critical care equipment, assessment techniques, and therapies must be appropriate for the child’s anatomy and physiology.
• The skilled critical care nurse is able to determine at a glance whether the child “looks good” or “looks bad.” This rapid evaluation includes visual and tactile assessment of the child’s color, perfusion, level of activity, and position. This assessment is similar to that described as the pediatric initial impression8a: level of consciousness, breathing, and color.
• Normal vital signs are not always appropriate vital signs in the seriously ill or injured patient. Tachycardia and tachypnea are usually appropriate when the child is in distress. Hypotension may be only a late sign of shock in children.
Psychosocial development
The child and parents or primary caretaker must be treated as a unit, and the parents should be allowed to remain with the child as much as possible. Visitation hours should be liberal, if not unlimited. Communication with the parents must be clear, frequent, and consistent. Joint nurse-physician rounds (involving all caregivers) that include the patient and family will help establish open and consistent communication within the healthcare team and with the family. Specific information about the child’s emotional and intellectual development and the response of the child and family to the child’s illness is included in Chapters 2 and 3.
General assessment
Initial Impression: “Looks Good” vs. “Looks Bad”
Every skilled critical care nurse and physician develops a systematic method for determining the severity of the patient’s condition, making both qualitative and quantitative assessments. Often, the initial, general impression of how the patient looks is more important than any single vital sign or clinical measurement.8a
The skilled critical care clinician can determine at a glance whether the patient “looks good” or “looks bad.” This determination requires a rapid visual evaluation of the child’s color, skin perfusion, level of consciousness (activity and responsiveness), breathing, and position of comfort (Box 1-1). Each portion of this assessment is reviewed in detail in this section.
Box 1-1 Assessment of General Appearance: “Looks Good” Versus “Looks Bad”
Level of consciousness (activity, responsiveness)
Evaluation of Vital Signs
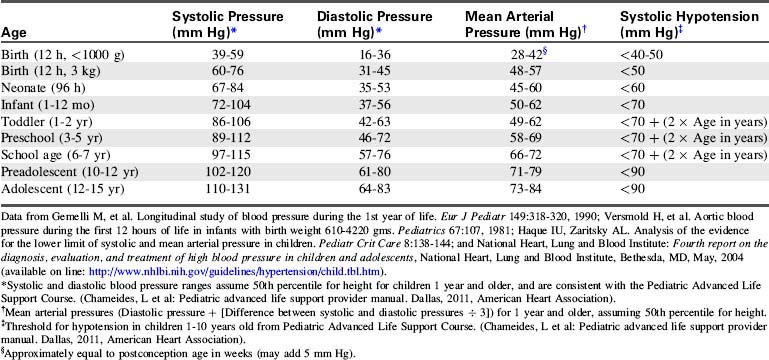
Normal vital signs ranges are provided in Tables 1-1 to 1-3. Evaluation of vital signs requires consideration of normal values for the child’s age,14a trends in the individual patient’s vital signs, and appropriate vital signs for the child’s condition. Remember that in children, shock can be present despite the observation of a normal blood pressure. Hypotension is often a late sign of shock in the pediatric patient.
Table 1-1 Normal Heart Rates in Children*
| Age | Awake Heart Rate (beats/min) | Sleeping Heart Rate (beats/min) |
| Neonate | 100-205 | 90-160 |
| Infant | 100-180 | 90-160 |
| Toddler | 98-140 | 80-120 |
| Preschooler | 80-120 | 65-100 |
| School-aged child | 75-118 | 58-90 |
| Adolescent | 60-100 | 50-90 |
* Always consider the patient’s normal range and clinical condition. Heart rate will normally increase with fever or stress.
Table 1-2 Normal Respiratory Rates in Children*14a
| Age | Rate (breaths/min) |
| Infant | 30-53 |
| Toddler | 22-37 |
| Preschool | 20-28 |
| School age | 18-25 |
| Adolescent | 12-20 |
* Consider the patient’s normal range. The child’s respiratory rate is expected to increase in the presence of fever or stress.
Assessment Format
An additional alphabetical format may be useful for pediatric critical care nurses. This format uses the first seven letters of the alphabet to help the nurse recall the steps in a seven-point check (Box 1-2). The seven essential assessment points include the child’s airway (and aeration), brain (neurologic function), circulation, drips or drugs administered, electrolyte balance, fluids (including fluid balance and fluid administration rate), genitourinary and gastrointestinal function, and growth and development.17a When caring for the critically ill neonate, this format can be modified to create a nine-point check, with the addition of the letter H for heat, or thermoregulation, and the letter I for immunologic immaturity.
General characteristics
Thermoregulation
The nurse can reduce cold stress by maintaining a neutral thermal environment for the neonate. A neutral thermal environment is the environmental temperature at which the infant maintains a rectal temperature of 37° C with the lowest oxygen consumption. This neutral temperature should be maintained during all aspects of the infant’s care, especially during transport and diagnostic tests. Over-bed radiant warmers can help maintain the infant’s temperature without interfering with observation and care. The beds are equipped with servo-control devices to adjust heat output in response to changes in the infant’s skin temperature. Adjustable alarms indicate when excessive warming is required to maintain the infant’s temperature or when the infant’s temperature varies from the selected range. (For further information regarding warming devices, see Chapter 21)
Fluid Requirements and Fluid Therapy
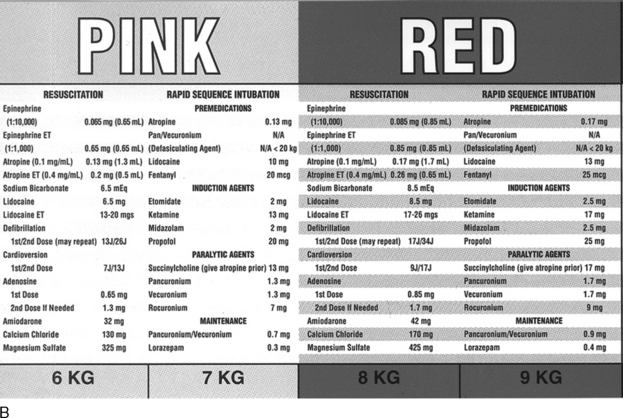
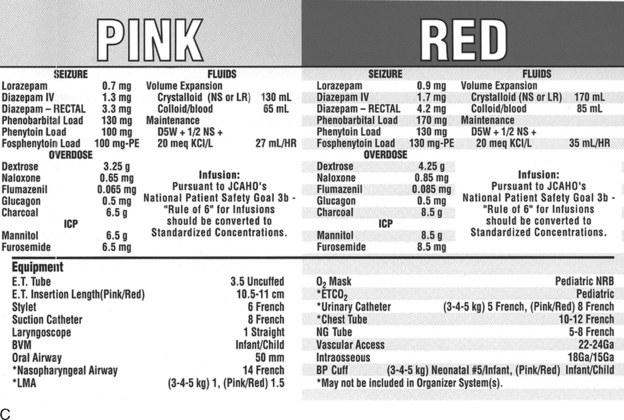
The weight can be estimated from body length using a length-based tape (see section, Cardiac Arrest and Resuscitation) such as the Broselow resuscitation tape (Fig. 1-1; see also Evolve Fig. 1-1 in the Chapter 1 Supplement on the Evolve Website.)
The estimate of maintenance fluid requirements (Table 1-4) provides a baseline for tailoring the fluid administration rate for each patient. Actual fluid administration is tailored to the child’s clinical condition. Normal insensible water losses average 300 to 400 mL/m2 BSA per day. Fever increases insensible water losses by approximately 0.42 mL/kg per hour per degree Celsius elevation in temperature above 37° C.40 Radiant warmers, phototherapy, and the presence of diaphoresis or large burns also will increase a child’s insensible water loss. Fluid retention can diminish fluid requirements postoperatively and fluid retention typically develops in the presence of congestive heart failure, respiratory failure, or renal failure.
Table 1-4 Formulas for Estimating Daily Maintenance Fluid and Electrolyte Requirements for Children
| Daily Requirements | Hourly Requirements | |
| Fluid Requirements Estimated from Weight* | ||
| Newborn (up to 72 hr after birth) | 60-100 mL/kg (newborns are born with excess body water) | – |
| Up to 10 kg | 100 mL/kg (can increase up to 150 mL/kg to provide caloric requirements if renal and cardiac function are adequate) | 4 mL/kg |
| 11-20 kg | 1000 mL for the first 10 kg + 50 mL/kg for each kg over 10 kg | 40 mL for first 10 kg + 2 mL/kg for each kg over 10 kg |
| 21-30 kg | 1500 mL for the first 20 kg + 25 mL/kg for each kg over 20 kg | 60 mL for first 20 kg + 1 mL/kg for each kg over 20 kg |
| Fluid Requirements Estimated from Body Surface Area (BSA) | ||
| Maintenance | 1500 mL/m2 BSA | – |
| Insensible losses | 300-400 mL/m2 BSA | – |
| Electrolytes | ||
| Sodium (Na) | 2-4 mEq/kg | – |
| Potassium (K) | 1-2 mEq/kg | – |
| Chloride (Cl) | 2-3 mEq/kg | – |
| Calcium (Ca) | 0.5-3 mEq/kg | – |
| Phosphorous (Phos) | 0.5-2 mmol/kg | – |
| Magnesium (Mg) | 0.4-0.9 mEq/kg | – |
* The “maintenance” fluids calculated by these formulas must only be used as a starting point to determine the fluid requirements of an individual patient. If intravascular volume is adequate, children with cardiac, pulmonary, or renal failure or increased intracranial pressure should generally receive less than these calculated “maintenance” fluids. The formula utilizing body weight generally results in a generous “maintenance” fluid total.
Consistent with values from Barakat AY, Ichikawa I: Laboratory data. In Ichikawa I, editor: Pediatric textbook of fluids and electrolytes, Baltimore, 1990, Williams and Wilkins; and Tan JM: Nephrology. In Custer JW, Rau RE, editors: The Johns Hopkins Hospital Harriet Lane Handbook, ed 18, Philadelphia, 2009, Mosby-Elsevier.
Children have proportionally more body water than do adults. Total body water constitutes approximately 75% to 80% of the full-term infant’s weight and 60% to 70% of the body weight of the adult. During the first weeks of life, most body water is located in the extracellular compartment, and much of this water is exchanged daily. For this reason and because the infant kidney is less able to concentrate urine (see section, Renal Function), dehydration can develop rapidly if the infant’s fluid intake is compromised or fluid losses are excessive.
Intravenous fluids are provided to flush monitoring lines, dilute medications, replace volume loss, or provide nutrition. In the past, hypotonic crystalloids (e.g., 5% dextrose with 0.2% sodium chloride) were routinely used for pediatric maintenance and replacement fluids, with the assumption that critically ill patients are likely to retain sodium and water. However, children are much more likely to develop hyponatremia if hypotonic rather than isotonic solutions are used, and isotonic fluids do not increase risk of hypernatremia.2,9 At this time there is insufficient evidence to identify a single optimal intravenous fluid for pediatric maintenance therapy, so practitioners will need to individualize intravenous fluid selection for each patient.
Electrolyte, Glucose, and Calcium Balance
Sodium is the major intravascular ion, and acute changes in serum sodium concentration will affect serum osmolality and free water movement. Hyponatremia in the critically ill child can result from antidiuretic hormone excess (i.e., the syndrome of inappropriate antidiuretic hormone secretion) and liberal water administration in excess of sodium, including administration of hypotonic fluids.4 Hyponatremia can also result from excess sodium losses, such as those occurring with adrenocortical insufficiency (see Chapter 12).
Hypernatremia can result from excessive sodium administration or free water loss, such as that occurring with diabetes insipidus or vomiting. Hypernatremia in infants and young children is most frequently observed as a complication of dehydration. Cerebral hemorrhage and cerebral dysfunction have been reported after abrupt correction of hyponatremia in adults (i.e., rapid rise in serum sodium concentration),18 and similar complications are thought to occur in children. Rapid correction of hypernatremia can produce an acute fall in serum osmolality, with resultant intracellular free water shift and cerebral edema. In general, when correcting hyponatremia or hypernatremia the child’s serum sodium concentration should be changed at a maximum rate of 10 to 12 mEq/24 h (or an average of 0.5 mEq/h).
The serum potassium should be expected to fall as the child’s pH rises, and it will rise as the pH falls because hydrogen ion moves intracellularly in exchange for potassium. A low serum potassium concentration in a patient with acidosis is problematic, because it will drop even lower as the acidosis is corrected (see Chapter 12).
Several case series in adult38 and pediatric patients suggested that uncontrolled hyperglycemia, whether it is endogenous or exogenous in origin, can be harmful to critically ill patients and can increase complication rates and decrease survival. Although this is a significant concern, other studies have found contradictory evidence, and additional studies are underway to clarify these issues. Use of insulin infusion to prevent hyperglycemia was associated with reduced critical care unit mortality in adult studies38 and one multicenter pediatric study,39 but was also associated with increased hypoglycemic episodes.
The serum ionized calcium concentration (normal value is approximately 4.8 to 5.2 mg/dL or 1.2 to 1.38 mmol/L) is the “working” calcium, involved in nerve and muscle function.12 Therefore, the healthcare team monitors ionized and total calcium concentration during critical illness and provides supplementary calcium for documented hypocalcemia.
A fall in total or ionized calcium is observed frequently in critically ill infants and children. Ionized hypocalcemia has been reported after cardiac arrest in children with septic shock or renal failure.41 The phosphate in citrate phosphate dextran-preserved blood will precipitate with ionized calcium, so some transfusions may produce ionized hypocalcemia.
Abnormalities in magnesium balance are observed frequently in critically ill patients. Magnesium affects parathyroid function and contributes to control of the intracellular potassium concentration. As a result, hypomagnesemia can contribute to refractory hypocalcemia or hypokalemia. In addition, it can be associated with increased neuromuscular excitability, gastrointestinal dysfunction, and arrhythmias.18
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Be sure to check out the supplementary content available at
Be sure to check out the supplementary content available at