Chapter 26 Clinical Anatomy
3 Which historical features in this patient increase the likelihood of a peripheral vascular disease diagnosis?
6 Outline the borders of the femoral triangle
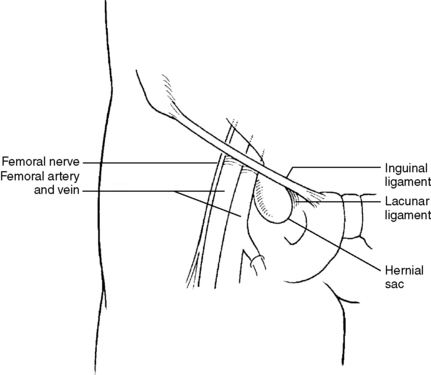
The femoral triangle is bordered by the inguinal ligament (superiorly), the sartorius (laterally), and the adductor longus (medially). From lateral to medial, it contains the femoral Nerve, common femoral Artery, femoral Vein, femoral canal (Empty space containing lymph nodes that is the site of femoral hernias), and the Lacunar ligament. The classic mnemonic is NAVEL (Fig. 26-1).
7 Describe the path of arterial blood from the femoral sheath to the feet
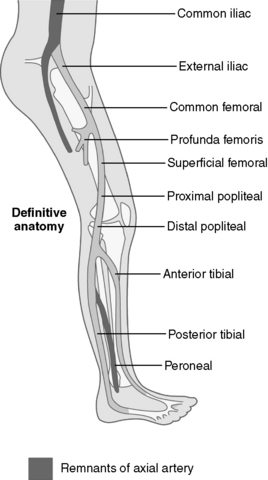
The common femoral artery quickly bifurcates at the level of the femoral trochanters into the profunda femoris (supplying primarily the thigh) and the superficial femoral artery, which runs through the adductor canal to the popliteal fossa (via the adductor hiatus) to become the popliteal artery. In the posterior compartment of the leg, the popliteal artery bifurcates into the tibiofibular trunk and the anterior tibial artery, which perforates the superior most portion of the interosseous membrane and descends in the anterior compartment until it crosses the ankle joint to become the dorsalis pedis artery, which can be palpated on the dorsum of the foot lateral to the tendon of the extensor hallucus longus. The tibiofibular trunk bifurcates to become the fibular artery, which runs downward in the deep posterior compartment of the leg, and the posterior tibial artery, which can be palpated between the medial malleolus and the calcaneus before bifurcating to form the lateral and medial plantar arteries, which supply the plantar aspect of the foot (Fig. 26-2).
9 In Table 26-1, cover the two columns on the right and attempt to list the drug class and mechanism of action for each of the drugs commonly used in treatment of peripheral vascular disease
Table 26-1 Selected Drugs Used to Treat Peripheral Vascular Disease
| Drug | Class | Mechanism of Action |
|---|---|---|
| Aspirin | Nonselective cyclooxygenase inhibitor | Irreversibly inhibits COX-1, decreasing platelet production of thromboxane A2, a vasoconstrictor and promoter of platelet aggregation |
| Clopidogrel | P2Y12 antagonist | Irreversibly inhibits P2Y12, a platelet ADP receptor necessary for activation of the glycoprotein IIb/IIIa pathway of platelet aggregation |
| Statins (e.g., atorvastatin, rosuvastatin, fluvastatin, lovastatin, pravastatin, simvastatin) | HMG-CoA reductase inhibitors | Inhibit HMG-CoA reductase, the rate-limiting step in endogenous production of cholesterol, to reduce the buildup of cholesterol in atherosclerotic plaques |
| Cilostazol | Phosphodiesterase III inhibitor | Inhibits cAMP phosphodiesterase III to reduce cAMP degradation, vasodilating peripheral arteries and inhibiting platelet aggregation |
| Pentoxifylline | Phosphodiesterase inhibitor | Inhibits cAMP phosphodiesterase; increases platelet flexibility and decreases blood viscosity |
ADP, adenosine diphosphate; cAMP, cyclic adenosine monophosphate; CoA, coenzyme A; COX-1, cyclooxygenase-1; HMG, hydroxymethylglutarate.
Summary Box: Peripheral Vascular Disease
 Peripheral vascular disease (PVD) is caused by atherosclerotic narrowing of peripheral arteries, usually of the lower extremities (LEs).
Peripheral vascular disease (PVD) is caused by atherosclerotic narrowing of peripheral arteries, usually of the lower extremities (LEs).
 Atherosclerotic lesions form preferentially at branch points and sites of tethering, as a result of turbulent blood flow and endothelial shear stress.
Atherosclerotic lesions form preferentially at branch points and sites of tethering, as a result of turbulent blood flow and endothelial shear stress.
 Blood flow to the LE: aorta → common iliac → external iliac → common femoral → profunda femoris (ends in thigh) and superficial femoral → popliteal → anterior tibial (supplies anterior compartment and ends as dorsalis pedis in the dorsum of the foot) and tibiofibular trunk → fibular (supplies lateral compartment) and posterior tibial (supplies posterior compartment) → lateral and medial plantar arteries.
Blood flow to the LE: aorta → common iliac → external iliac → common femoral → profunda femoris (ends in thigh) and superficial femoral → popliteal → anterior tibial (supplies anterior compartment and ends as dorsalis pedis in the dorsum of the foot) and tibiofibular trunk → fibular (supplies lateral compartment) and posterior tibial (supplies posterior compartment) → lateral and medial plantar arteries.
 From lateral to medial, the femoral triangle contains the femoral Nerve, Artery, Vein, canal (Empty space), and the Lacunar ligament. Remember the acronym NAVEL.
From lateral to medial, the femoral triangle contains the femoral Nerve, Artery, Vein, canal (Empty space), and the Lacunar ligament. Remember the acronym NAVEL.
2 If Oscar had forced his upper extremity above his head by grabbing the handlebars of the motorcycle to prevent his fall, he may have presented with a loss of sensation and impaired flexion in digits 4 and 5, impaired wrist flexion, hyperextension of the metacarpophalangeal joints, and an inability to abduct and adduct digits 2 to 5. What would be the diagnosis in this situation?
This pattern of injury is characteristic of a tear of nerve roots C8 and T1 (or a lower trunk tear) of the brachial plexus, a condition known as Klumpke’s paralysis. The ulnar nerve is exclusively supplied by C8 and T1 and is responsible for sensory innervation to the fifth digit, the medial half of the fourth digit, and the corresponding palmar surface of the hand. It controls the majority of medial digit flexion (via the medial heads of the flexor digitorum profundus and the flexor digiti minimi muscles) as well as abduction (via the dorsal interossei) and adduction (via the palmar interossei) of digits 2 to 5. It is partially responsible for metacarpophalangeal joint flexion (via the lumbricals of digits 4 and 5) and wrist flexion (via the flexor carpi ulnaris) (Fig. 26-3).
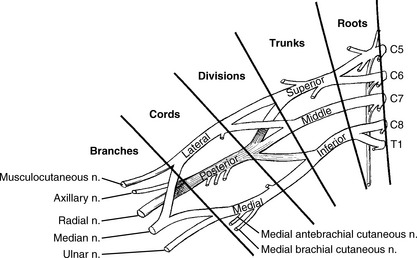
Figure 26-3 Roots, trunks, divisions, cords, and branches of the brachial plexus.
(From Miller RD: Miller’s Anesthesia, 6th ed. Philadelphia, Churchill Livingstone, 2005.)
3 What structure has Oscar injured this time and how has it led to his upper extremity position?
5 Outline the contents of the carpal tunnel
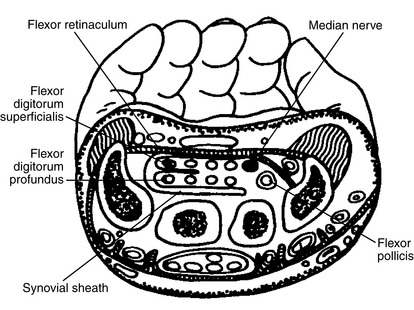
The carpal tunnel is formed by the eight wrist (carpal) bones and the transverse carpal ligament (flexor retinaculum), which spans from the tubercles of the scaphoid and trapezium to the pisiform and the hook of the hamate. The contents include the four flexor digitorum profundus tendons, the four flexor digitorum superficialis tendons, the flexor pollicis longus tendon, and the median nerve (Fig. 26-4).
6 Name the muscles of the thenar and hypothenar eminences and describe their function
 Thenar eminence (located proximal to the thumb): opponens pollicis, abductor pollicis brevis, and flexor pollicis brevis (all innervated by the median nerve after it passes through the carpal tunnel).
Thenar eminence (located proximal to the thumb): opponens pollicis, abductor pollicis brevis, and flexor pollicis brevis (all innervated by the median nerve after it passes through the carpal tunnel).
 Hypothenar eminence (located proximal to the fifth digit): opponens digiti minimi, abductor digiti minimi, and flexor digiti minimi (all innervated by the ulnar nerve).
Hypothenar eminence (located proximal to the fifth digit): opponens digiti minimi, abductor digiti minimi, and flexor digiti minimi (all innervated by the ulnar nerve).
 Function: These two groups have symmetrical function. As their names suggest, each group has a muscle that performs opposition, abduction, and flexion.
Function: These two groups have symmetrical function. As their names suggest, each group has a muscle that performs opposition, abduction, and flexion.
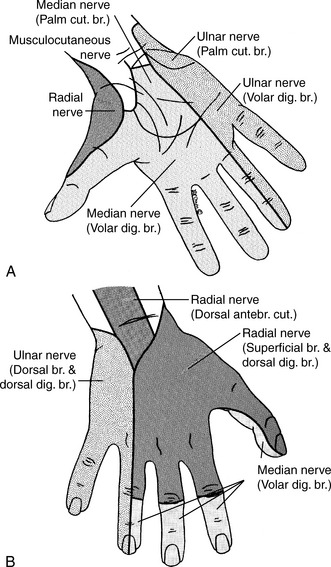
7 Describe the pattern of sensory innervation of the hand
 Median nerve: lateral palm, thumb, digits 2 and 3, and lateral half of digit 4.
Median nerve: lateral palm, thumb, digits 2 and 3, and lateral half of digit 4.
 Ulnar nerve: medial palm, medial dorsal hand, digit 5, and medial half of digit 4.
Ulnar nerve: medial palm, medial dorsal hand, digit 5, and medial half of digit 4.
 Radial nerve: lateral dorsal hand, extending distally to the proximal interphalangeal (PIP) joint of digits 1 to 3 and the lateral half of digit 4 (Fig. 26-5).
Radial nerve: lateral dorsal hand, extending distally to the proximal interphalangeal (PIP) joint of digits 1 to 3 and the lateral half of digit 4 (Fig. 26-5).
9 What are the three most common sites of humerus fracture, and which nerve and artery are at risk at each of these sites?
Table 26-2 Three Most Common Sites of Humerus Fracture
| Humerus Fracture Site | Nerve | Artery |
|---|---|---|
| Surgical neck | Axillary | Anterior and posterior circumflex humeral (branches of the axillary artery) |
| Midshaft | Radial | Profunda brachii (branch of the brachial artery) |
| Supracondylar | Median | Brachial |
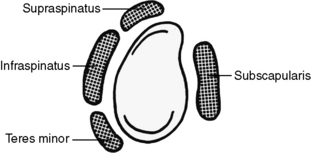
10 On reviewing Jake’s past medical history, you note that his baseball career was marred by a partially torn rotator cuff. Describe why the rotator cuff makes the glenohumeral joint different from other joints, and name its four components
Most joints are stabilized primarily by a ligamentous capsule, but the glenohumeral joint is stabilized primarily by the rotator cuff, which consists of the tendons of four muscles—supraspinatus, infraspinatus, teres minor, and subscapularis (Fig. 26-6). This design allows the glenohumeral joint to have the widest range of motion of all joints in the body, at the expense of stability and resistance to injury. The rotator cuff stabilizes the glenohumeral joint by pulling the head of the humerus toward the glenoid fossa of the scapula as other muscles flex, extend, abduct, or adduct the arm. Rapid, forceful, or repetitive movements (such as repeatedly throwing a baseball) can tear the tendons of the rotator cuff, leading to a lack of joint stability, restricted movement, and pain.
Summary Box: Upper Extremity Injuries
 From proximal to distal, the brachial plexus consists of:
From proximal to distal, the brachial plexus consists of:
 The musculocutaneous nerve innervates the flexors of the elbow.
The musculocutaneous nerve innervates the flexors of the elbow.
 The axillary nerve innervates the deltoid and teres minor muscles as well as the long head of the triceps brachii.
The axillary nerve innervates the deltoid and teres minor muscles as well as the long head of the triceps brachii.
 The radial nerve innervates the extensors in the arm and forearm.
The radial nerve innervates the extensors in the arm and forearm.
 The ulnar nerve innervates the medial heads of the flexor digitorum profundus, the flexor carpi ulnaris, medial lumbricals, interossei, and hypothenar muscles.
The ulnar nerve innervates the medial heads of the flexor digitorum profundus, the flexor carpi ulnaris, medial lumbricals, interossei, and hypothenar muscles.
 The median nerve innervates the anterior forearm muscles not innervated by the ulnar nerve, the lateral lumbricals, and the thenar muscles.
The median nerve innervates the anterior forearm muscles not innervated by the ulnar nerve, the lateral lumbricals, and the thenar muscles.
 The blood supply to the upper extremity (UE) is from the brachial artery, the continuation of the axillary artery after it crosses the teres major.
The blood supply to the upper extremity (UE) is from the brachial artery, the continuation of the axillary artery after it crosses the teres major.
 The carpal tunnel consists of the eight carpal bones and the transverse carpal ligament. It contains the median nerve and the tendons of the long flexors of the digits.
The carpal tunnel consists of the eight carpal bones and the transverse carpal ligament. It contains the median nerve and the tendons of the long flexors of the digits.
 The rotator cuff consists of the tendons of four muscles: supraspinatus, infraspinatus, teres minor, and subscapularis.
The rotator cuff consists of the tendons of four muscles: supraspinatus, infraspinatus, teres minor, and subscapularis.
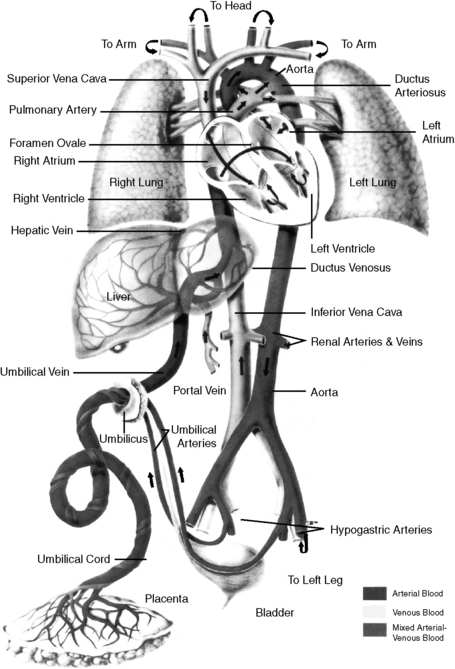
2 What is the utility of the ductus arteriosus?
In utero, this connection between the aorta and the pulmonary artery acts as a right-to-left shunt. It allows the majority of oxygenated blood (which has entered the right side of the heart through the route of placenta → umbilical vein → ductus venosus → inferior vena cava) to bypass the developing (nonfunctioning) lungs and enter the systemic circulation. Just after birth, the ductus arteriosus normally closes and undergoes fibrotic degeneration to become the ligamentum arteriosum (Fig. 26-7).
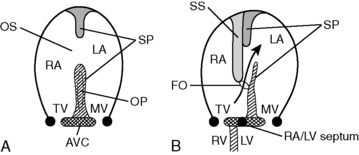
6 What are the three most common types of atrial septal defect?
Normally, the atrial septum develops completely to the left of the sinus venosus, the structure that is to become the superior and inferior venae cavae and part of the right atrium. In this rare defect, the septum develops anterior to the sinus venosus, allowing interatrial flow via the sinus venosus (Fig. 26-8).
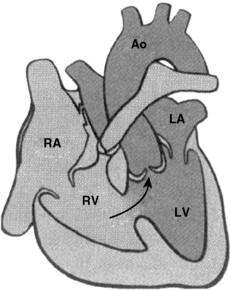
11 How does tetralogy of Fallot cause cyanosis?
Pulmonary stenosis causes a high resistance to flow through the pulmonary trunk. Coupled with concentric right ventricular hypertrophy, this leads to high right-sided heart pressures, causing right-to-left flow through the VSD (Fig. 26-9). When a critical proportion of deoxygenated blood is shunted through the VSD and mixed with oxygenated blood, cyanosis appears. It is classically seen first in the fingers and lips.
12 What is the cause of tetralogy of Fallot?
Summary Box: Congenital Heart Defects
 The ductus arteriosus connects the pulmonary artery to the aorta and allows blood to bypass the developing lungs during fetal life.
The ductus arteriosus connects the pulmonary artery to the aorta and allows blood to bypass the developing lungs during fetal life.
 The patency of the ductus arteriosus is maintained by low PO2 and prostaglandin E2. It can be pharmacologically closed with indomethacin or kept open with alprostadil.
The patency of the ductus arteriosus is maintained by low PO2 and prostaglandin E2. It can be pharmacologically closed with indomethacin or kept open with alprostadil.
 During fetal life, blood also bypasses the developing lungs via the foramen ovale, which is appropriately patent at this time.
During fetal life, blood also bypasses the developing lungs via the foramen ovale, which is appropriately patent at this time.
 Atrial septal defect (ASD) can be recognized on cardiac auscultation by a mild systolic ejection murmur and wide, fixed splitting of S2.
Atrial septal defect (ASD) can be recognized on cardiac auscultation by a mild systolic ejection murmur and wide, fixed splitting of S2.
 Ventricular septal defect (VSD) is the most common congenital heart defect.
Ventricular septal defect (VSD) is the most common congenital heart defect.
 Eisenmenger’s complex refers to a right-to-left shunt (resulting in cyanosis) that occurred because a left-to-right shunt (VSD, ASD, or patent ductus arteriosus [PDA]) caused right-sided heart overload and pulmonary hypertension, leading to high right-sided heart pressures and shunt reversal.
Eisenmenger’s complex refers to a right-to-left shunt (resulting in cyanosis) that occurred because a left-to-right shunt (VSD, ASD, or patent ductus arteriosus [PDA]) caused right-sided heart overload and pulmonary hypertension, leading to high right-sided heart pressures and shunt reversal.
 Tetralogy of Fallot is characterized by VSD, overriding aorta, pulmonary stenosis, and right ventricular hypertrophy. It is the most common cause of right-to-left cyanotic shunt in infants.
Tetralogy of Fallot is characterized by VSD, overriding aorta, pulmonary stenosis, and right ventricular hypertrophy. It is the most common cause of right-to-left cyanotic shunt in infants.