Chapter 10
Claim Forms
1. Define terms, phrases, abbreviations, and acronyms.
2. Explain the purpose of claim forms.
3. Describe manual and electronic claim submission and discuss advantages and disadvantages of each method.
4. Explain the difference between the CMS-1500 and CMS-1450 (UB-04) and outline when they are used.
5. Discuss variations in claim form usage and coding systems used for outpatient and inpatient claims.
6. Demonstrate an understanding of data requirements and completion instructions for the CMS-1450 (UB-04).
Electronic data interchange (EDI)
National Provider Identifier (NPI)
National Uniform Billing Committee (NUBC)
North American Industry Classification System (NAICS) Code
State Uniform Billing Committees (SUBC)
Tax identification number (TIN)
American National Standards Institute
Centers for Medicare and Medicaid Services
Employer identification number
Healthcare Common Procedure Coding System
Health Insurance Association of America
Health Insurance Portability and Accountability Act
Health Insurance Prospective Payment System
International Classification of Diseases, 10th Revision, Clinical Modification
International Classification of Diseases, 10th Revision, Procedure Coding System
Medicare Severity-Diagnosis Related Groups
North American Industry Classification System Code
National Uniform Billing Committee
State Uniform Billing Committees
Uniform Hospital Discharge Data Set
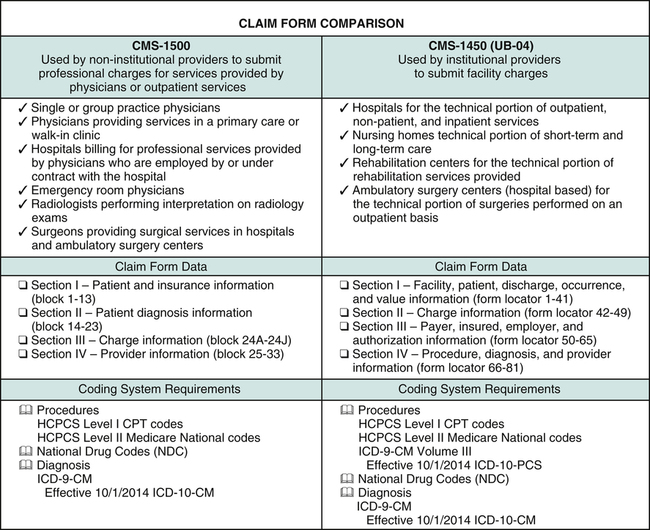
Hospital coding and billing professionals will be required to have an understanding of the ICD-9-CM coding system and will need to transition to ICD-10. For this reason, this chapter will provide examples of claim form completion using the ICD-10 coding systems. The chapter illustrates how various elements relate to claim forms. Although hospitals may use both claim forms to submit charges, the CMS-1450 (UB-04) is the primary claim form used for submission of charges for most services, procedures, and items. Therefore, this chapter will provide a brief overview of the CMS-1500, followed by an in-depth discussion on claim form completion requirements for the CMS-1450 (UB-04).
Claim Form Submission
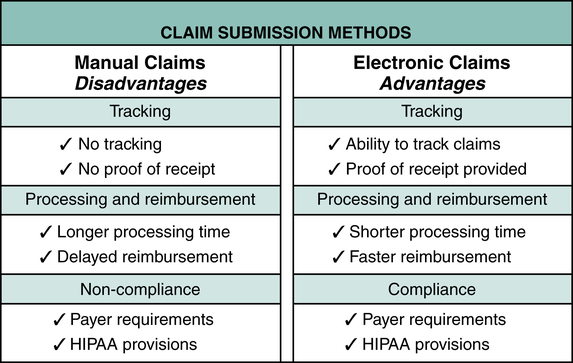
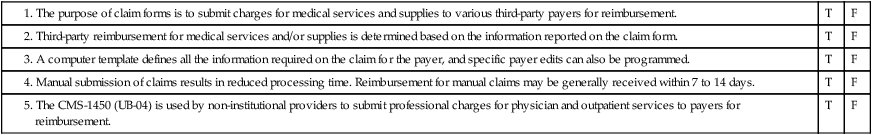
Today, most claim forms are computer generated and submitted electronically in accordance with payer requirements and Health Insurance Portability and Accountability Act (HIPAA) Title II provisions. Two universal claim forms are used to submit charges to all payers, the CMS-1500 and CMS-1450 (UB-04). Although these claim forms are universal, the guidelines for completion vary by payer. These variations are addressed by setting up a computer template that includes required information by payer type. A template defines all the information required on the claim for the payer, and specific payer edits can also be programmed. The payer-specific knowledge is beyond the scope of this text; however, an overview of general claim form completion requirements is provided. Hospital billing and coding professionals should have knowledge of payer specifications available when submitting claims to various payers. The following review of electronic versus manual claim submission is illustrated in Figure 10-1.
Electronic Claim Submission
In accordance with HIPAA regulations, standard formats for electronic transactions have been adopted. The adopted standard formats were developed by the American National Standards Institute (ANSI). The standard transaction format for the CMS-1500 is the ANSI X12 837 and the format for the CMS-1450 (UB-04) is ANSI X12 837I. The standard transaction formats contain elements found on the CMS-1500 and CMS-1450 (UB-04) paper claims. The current standard format, Version 5010, was adopted and implemented. The compliance date for all HIPAA-covered entities to transition to Version 5010 was January 1, 2012. Details regarding Version 5010 can be viewed on the CMS Web site at http://www.cms.gov/ICD10/11a_Version_5010.asp#TopOfPage.
Transmission Through a Clearinghouse
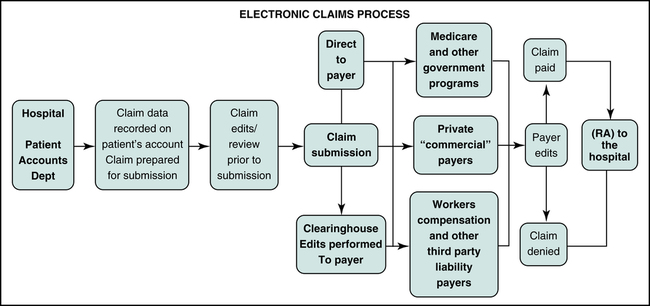
The electronic claim submission process for a hospital is illustrated in Figure 10-2. Functions required to complete the process are performed by the hospital’s Patient Financial Services (PFS) Department. Data required for claim submission is recorded on the patient’s computerized account during the patient visit. The hospital’s computer system performs edits to identify issues with the claim data. Any issues identified during the edit process can be resolved before transmission. Claims are then prepared and transmitted to the payer directly or through a clearinghouse. The clearinghouse may also conduct edits. After the claim has satisfied the payer’s edit, payment determination is made. A remittance advice (RA) is forwarded to the hospital that explains payment determination. Remittance advices can also be transmitted electronically by various payers.
Claim Form Variations
Two claim forms are universally accepted by payers today: the CMS-1500 and the CMS-1450 (UB-04). The CMS-1500 is used by non-institutional providers to submit professional charges for physician and outpatient services to payers for reimbursement. The CMS-1450 (UB-04) is used by institutional providers to submit hospital facility charges for services, procedures, and items to payers for reimbursement. It is necessary to complete these claim forms in accordance with payer guidelines and specifications. Claim form completion specifications vary by payer. Hospital billing professionals are required to gain knowledge regarding various payer specifications for claim form completion. The category of service generally dictates which claim form is used. Claim form variations for outpatient, inpatient, and non-patient services are outlined in Figure 10-3.
CMS-1450 (UB-04) Claim Form Overview
Claim Form Data
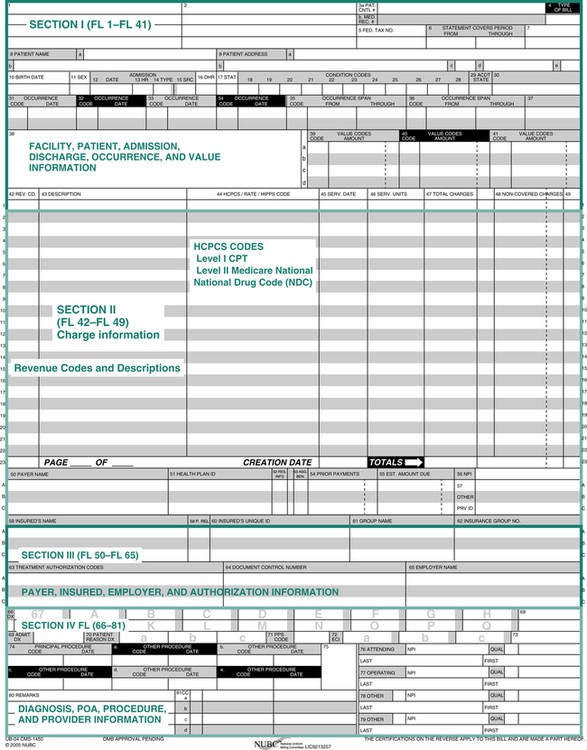
The CMS-1450 (UB-04) consists of 81 data fields that are referred to as form locators (FL). The billing requirements for each field and the revenue codes are revised on an ongoing basis by the NUBC, SUBC, and CMS. The CMS-1450 (UB-04) can be viewed in four sections, in which information about the patient, facility, charges, and physicians involved in the patient’s care is recorded, as illustrated in (Figure 10-4).
CMS-1450 (UB-04) Instructions
The CMS-1450 (UB-04) is a summary of the hospital visit and charges incurred. Information used to complete the claim form is entered into the patient’s account on the computer. Required claim data for each field are pulled from the patient’s account and the hospital data file. Information about charges for services provided is outlined on the detailed itemized statement, which may be attached to manual claims. Payers who require electronic claims submission may request a detailed itemized statement after initial review of the CMS-1450 (UB-04) claim data. Completion requirements and specifications for the CMS-1450 (UB-04) vary by payer; therefore, it is critical to obtain payer specifications to ensure compliance with payer guidelines. Detailed information regarding the claim form and instructions for completion can be viewed on the CMS Web site at https://www.cms.gov/ElectronicBillingEDITrans/15_1450.asp. General instructions for each form locator (FL) are outlined below in four sections to provide a basic understanding of the data required.
Section I: Facility, Patient, Admission, Discharge, Occurrence, and Value Information (FL 1 to 41)
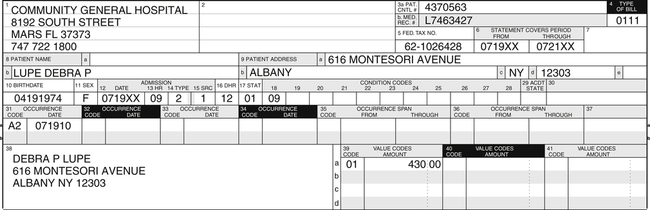
This section is used to provide information about the facility, when the patient was admitted and discharged, the patient’s name and address, and other information about the hospital visit, as illustrated in Figure 10-5. An overview of data required for each form locator (FL) is outlined below.
FL 4: Type of Bill
The four-digit type of bill number is recorded in this field to provide information about the facility bill type. The first digit is zero. The second digit describes the facility type. The third digit indicates the type of care. The fourth digit is designed to let the payer know the expected frequency of the bills that will be submitted. Examples of type of bill code options include 0111 (Hospital inpatient-admit through discharge claim) and 0113 (Hospital outpatient-admit through discharge claim) as illustrated in Concept Review Box 10-7. A detailed listing of FL 4, type of bill, three-digit options and common fourth-digit frequency code options is outlined in Appendix B.