CHAPTER 15 As indicated in Figure 15–1, neostigmine contains a quaternary nitrogen atom, and hence always carries a positive charge. Because of this charge, neostigmine cannot readily cross membranes, including those of the GI tract, blood-brain barrier, and placenta. Consequently, neostigmine is absorbed poorly following oral administration and has minimal effects on the brain and fetus. Neostigmine and the other reversible cholinesterase inhibitors can be envisioned as poor substrates for ChE. As indicated in Figure 15–2, the normal function of ChE is to break down acetylcholine into choline and acetic acid. This process is termed a hydrolysis reaction because of the water molecule involved. As depicted in Figure 15–3A, hydrolysis of ACh takes place in two steps: (1) binding of ACh to the active center of ChE, followed by (2) splitting of ACh, which regenerates free ChE. The overall reaction between ACh and ChE is extremely fast. As a result, one molecule of ChE can break down a huge amount of ACh in a very short time. As depicted in Figure 15–3B, the reaction between neostigmine and ChE is much like the reaction between ACh and ChE. The only difference is that ChE splits neostigmine more slowly than it splits ACh. Hence, once neostigmine becomes bound to the active center of ChE, the drug remains in place for a relatively long time, thereby preventing ChE from catalyzing the breakdown of ACh. ChE remains inhibited until it finally succeeds in splitting neostigmine off. The effects of cholinesterase inhibitors on skeletal muscle are dose dependent. At therapeutic doses, these drugs increase force of contraction. In contrast, toxic doses reduce force of contraction. Contractile force is reduced because excessive amounts of ACh at the NMJ keep the motor end-plate in a state of constant depolarization, thereby causing depolarizing neuromuscular blockade (see Chapter 16). Most of the precautions and contraindications regarding the cholinesterase inhibitors are the same as those for the direct-acting muscarinic agonists. These include (1) obstruction of the GI tract, (2) obstruction of the urinary tract, (3) peptic ulcer disease, (4) asthma, (5) coronary insufficiency, and (6) hyperthyroidism. The rationales underlying these precautions are discussed in Chapter 14. In addition to precautions related to muscarinic stimulation, cholinesterase inhibitors are contraindicated for patients receiving succinylcholine.
Cholinesterase inhibitors and their use in myasthenia gravis
Reversible cholinesterase inhibitors
Neostigmine
Chemistry
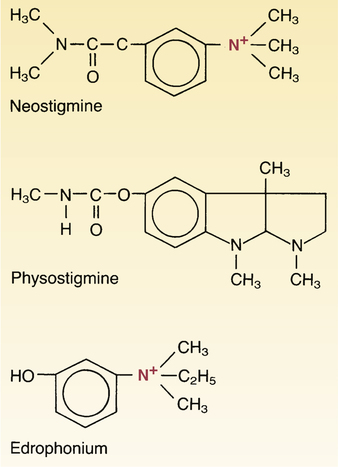
 Structural formulas of reversible cholinesterase inhibitors.
Structural formulas of reversible cholinesterase inhibitors.
Note that neostigmine and edrophonium are quaternary ammonium compounds, but physostigmine is not. What does this difference imply about the relative abilities of these drugs to cross membranes, including the blood-brain barrier?
Mechanism of action
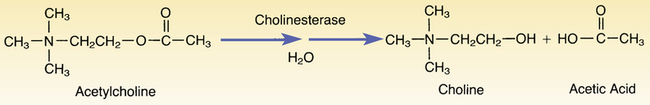
 Hydrolysis of acetylcholine by cholinesterase.
Hydrolysis of acetylcholine by cholinesterase.
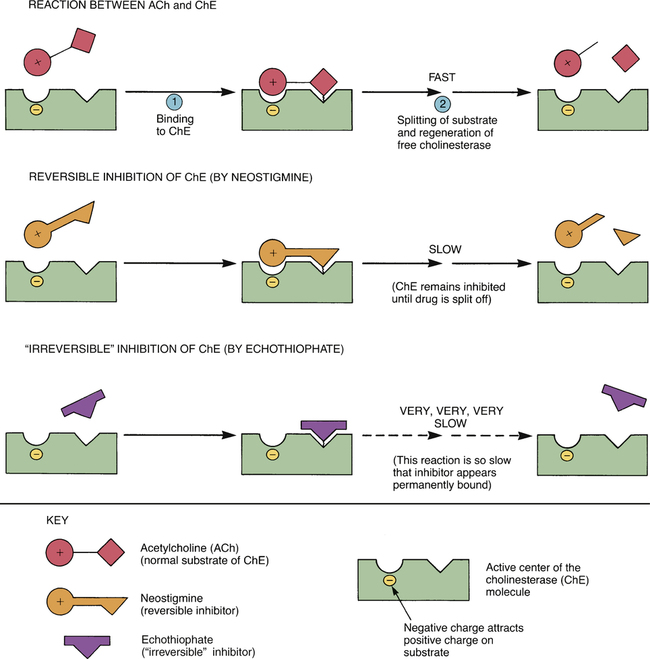
 Inhibition of cholinesterase by reversible and “irreversible” inhibitors. (See text for details.)
Inhibition of cholinesterase by reversible and “irreversible” inhibitors. (See text for details.)
Pharmacologic effects
Neuromuscular effects.
Precautions and contraindications
















