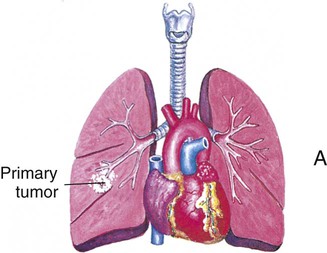
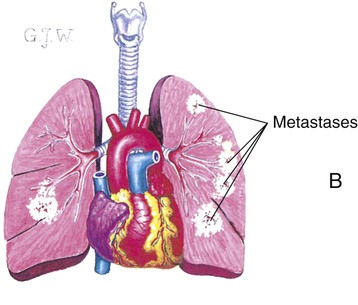
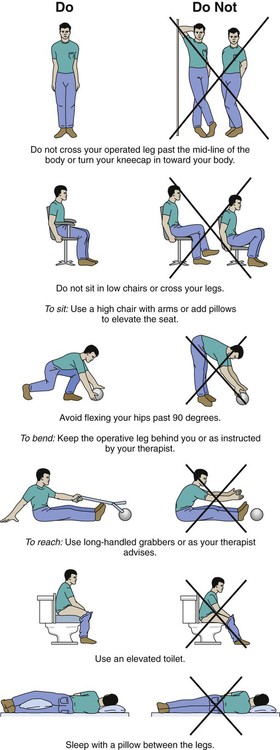
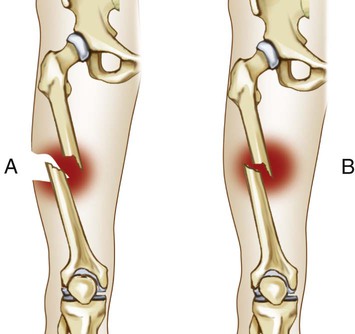
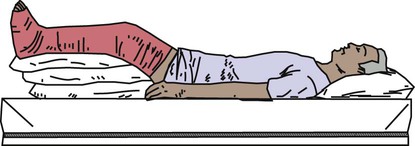
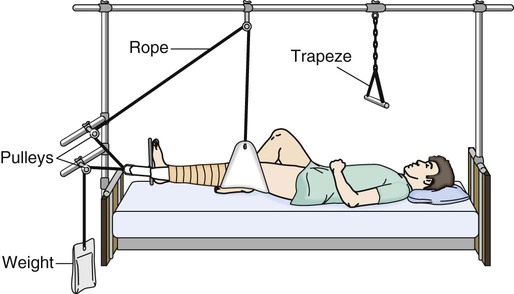
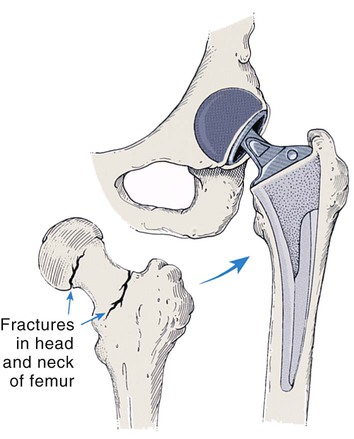
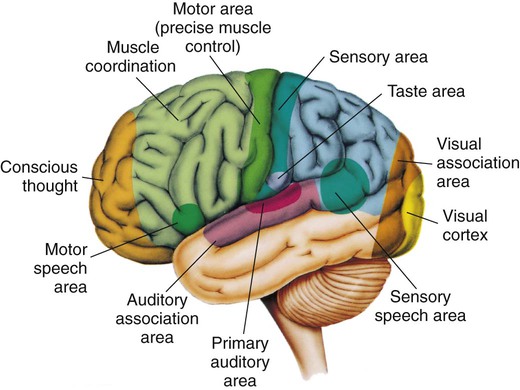
AIDS Acquired immunodeficiency syndrome ALS Amyotrophic lateral sclerosis BPH Benign prostatic hyperplasia COPD Chronic obstructive pulmonary disease HIV Human immunodeficiency virus STD Sexually transmitted disease • Define the key terms and key abbreviations listed in this chapter. • Describe cancer and how it is treated. • Describe musculo-skeletal and nervous system disorders and the care required. • Describe hearing loss and eye disorders and the care required. • Describe cardiovascular and respiratory disorders and the care required. • Describe digestive, urinary, and reproductive disorders and the care required. • Describe endocrine, immune system, and skin disorders and the care required. • Explain how to promote PRIDE in the person, the family, and yourself. Understanding common health problems gives meaning to the required care. The nurse gives you more information as needed. Refer to Chapter 7 as you study this chapter. Cells reproduce for tissue growth and repair. Cells divide in an orderly way. Sometimes cell division and growth are out of control. A mass or clump of cells develops. This new growth of abnormal cells is called a tumor. Tumors are benign or malignant (Fig. 28-1). • Benign tumors do not spread to other body parts. They can grow to a large size, but rarely threaten life. They usually do not grow back when removed. • Malignant tumors (cancer) invade and destroy nearby tissues. They can spread to other body parts. They may be life-threatening. Sometimes they grow back after removal. Metastasis is the spread of cancer to other body parts (Fig. 28-2). Cancer cells break off the tumor and travel to other body parts. New tumors grow at those sites. This occurs if cancer is not treated and controlled. • Growing older. Cancer occurs in all age-groups. However, most cancers occur in persons over 65 years of age. • Tobacco. This includes using tobacco (smoking, snuff, and chewing tobacco) and being around tobacco (second-hand smoke). • Sunlight. Sun, sunlamps, and tanning booths cause early aging of the skin and skin damage. These can lead to skin cancer. • Ionizing radiation. This can cause cell damage that leads to cancer. Sources are x-rays and radon gas that forms in the soil and some rocks. Radioactive fallout is another source. It can come from the production, testing, or use of atomic weapons. • Certain chemicals and other substances. Examples include paint, pesticides, and used engine oil. • Some viruses and bacteria. Certain viruses increase the risk of cancers—cervical, liver, lymphoma, leukemia, Kaposi’s sarcoma (associated with AIDS, p. 452), stomach. • Certain hormones. Hormone replacement for menopause is an example. It may increase the risk of breast cancer. • Family history of cancer. Certain cancers tend to occur in families. They include melanoma and cancers of the breast, ovary, prostate, and colon. • Alcohol. More than 2 drinks a day increases the risk of certain cancers—mouth, throat, esophagus, larynx, liver, and breast. • Poor diet, lack of physical activity, and being over-weight. A high-fat diet increases the risk of cancers of the colon, uterus, and prostate. Lack of physical activity and being over-weight increase the risk for cancers of the breast, colon, esophagus, kidney, and uterus. If detected early, cancer can be treated and controlled (Box 28-1). Treatment depends on the tumor type, its site and size, and if it has spread. The treatment goal may be to: Surgery, radiation therapy, and chemotherapy are the most common treatments. • Radiation therapy kills cells. X-ray beams are aimed at the tumor. Sometimes radioactive material is implanted in or near the tumor. Cancer cells and normal cells receive radiation. Both are destroyed. Burns, skin breakdown, and hair loss can occur at the treatment site. Special skin care measures are ordered. Extra rest is needed for fatigue. Discomfort, nausea, vomiting, diarrhea, and loss of appetite (anorexia) are other side effects. • Chemotherapy involves drugs that kill cells. Cancer cells and normal cells are affected. Side effects include hair loss (alopecia), poor appetite, nausea, vomiting, diarrhea, and stomatitis—inflammation (itis) of the mouth (stomat). Bleeding and infection are risks from decreased blood cell production. Persons with cancer have many needs. They include: • Preventing bowel problems—constipation from pain-relief drugs; diarrhea from some cancer treatments • Dealing with treatment side effects • Psychological and social needs Persons dying of cancer often receive hospice care (Chapters 1 and 32). Support is given to the person and family. See Focus on Communication: The Person’s Needs. There is no cure. Treatment involves: • Pain relief. Drugs decrease swelling and inflammation and relieve pain. • Heat and cold. Heat relieves pain, increases blood flow, and reduces swelling. Cold applications may be used after joint use. • Exercise. Exercise decreases pain, increases flexibility, and improves blood flow. It helps with weight control and promotes fitness. Mental well-being improves. The person is taught what exercises to do. • Rest and joint care. Good body mechanics, posture, and regular rest protect the joints. Relaxation methods are helpful. Canes and walkers provide support. Splints support weak joints and keep them in alignment. • Weight control. If over-weight, weight loss reduces stress on weight-bearing joints. And it helps prevent further joint injury. • Healthy life-style. The focus is on fitness, exercise, rest, managing stress, and good nutrition. RA occurs on both sides of the body. For example, if the right wrist is involved, so is the left wrist. The wrist and finger joints near the hand are often affected (Fig. 28-3). Other joints affected are the neck, shoulders, elbows, hips, knees, ankles, and feet. Joints are tender, warm, and swollen. Other body parts may be affected. Fatigue and fever are common. The person does not feel well. Symptoms may last for many years. The person’s care plan may include: • Rest balanced with exercise. Short rest periods during the day are better than long times in bed. An exercise program is prescribed. Range-of-motion (ROM) exercises are included. Exercise helps maintain healthy and strong muscles, joint mobility, and flexibility. It also promotes sleep, reduces pain, and helps weight control. • Proper positioning. Contractures and deformities are prevented. Bed-boards, a bed cradle, trochanter rolls, and pillows are used. • Joint care. Good body mechanics and body alignment, wrist and hand splints, and self-help devices reduce stress on joints. Some need walking aids. • Weight control. Excess weight places stress on the weight-bearing joints. Exercise and a healthy diet help control weight. • Measures to reduce stress. Relaxation, distraction, exercise, and regular rest help reduce stress. All ethnic groups are at risk. Other risk factors include a family history of the disease, being thin or having a small frame, eating disorders (Chapter 29), tobacco use, alcoholism, lack of exercise, bedrest, and immobility. Exercise and activity are needed for bone strength. Bone must bear weight to form properly. If not, calcium is lost from the bone. The bone becomes porous and brittle. A fracture is a broken bone. Fractures are open or closed (Fig. 28-5). • Open fracture (compound fracture). The broken bone has come through the skin. • Closed fracture (simple fracture). The bone is broken but the skin is intact. • Loss of function or movement • Movement where motion should not occur • Deformity (the part is in an abnormal position) • Bruising and skin color changes at the fracture site • Closed reduction and external fixation. The bone is moved back into place. The bone is not exposed. • Open reduction and internal fixation. This requires surgery. The bone is exposed and moved into alignment. Nails, rods, pins, screws, plates, or wires keep the bone in place. • Casts. Casts are made of plaster of Paris, plastic, or fiberglass. Plastic and fiberglass casts dry quickly. A plaster of Paris cast dries in 24 to 48 hours. It is odorless, white, and shiny when dry. When wet, it is gray and cool and has a musty smell. The nurse may ask you to assist with care (Box 28-3). • Traction. A steady pull from 2 directions keeps the bone in place. Weights, ropes, and pulleys are used (Fig. 28-8). Traction is applied to the neck, arms, legs, or pelvis. To assist with the person’s care, see Box 28-4, p. 432. Fractured hips are common in older persons (Fig. 28-9). The fracture requires internal fixation (p. 431) or partial or total hip replacement. Adduction, internal rotation, external rotation, and severe hip flexion are avoided after surgery. Rehabilitation is usually needed. Post-operative problems present life-threatening risks. They include respiratory complications, urinary tract infections, and thrombi (blood clots) in the leg veins. Pressure ulcers, constipation, and confusion are other risks. Box 28-5 describes the required care. Gangrene is a condition in which there is death of tissue. Causes include infection, injuries, and vascular disorders. Blood flow is affected. Tissues do not get enough oxygen and nutrients. Tissues become black, cold, and shriveled (Fig. 28-11). Surgery is needed to remove dead tissue. Gangrene can cause death. The person is fitted with a prosthesis—an artificial replacement for a missing body part (Fig. 28-12). Occupational and physical therapists help the person use the prosthesis. Brain cells in the affected area do not get enough oxygen and nutrients. Brain damage occurs. Functions controlled by that part of the brain are lost (Fig. 28-13). Stroke is a leading cause of death and disability among adults in the United States. See Box 28-6 for warning signs. The person needs emergency care. Blood flow to the brain must be restored as soon as possible. Warning signs may last a few minutes. This is called a transient ischemic attack (TIA). (Transient means temporary or short term. Ischemic means to hold back [ischein] blood [hemic].) Blood supply to the brain is interrupted for a short time. A TIA may occur before a stroke. The person also may have nausea, vomiting, and memory loss. Unconsciousness, noisy breathing, high blood pressure, slow pulse, redness of the face, and seizures may occur. So can hemiplegia—paralysis (plegia) on 1 side (hemi) of the body. The person may lose bowel and bladder control and the ability to speak. (See “Aphasia.”) All stroke-like symptoms signal the need for emergency care. The effects of stroke include: • Loss of face, hand, arm, leg, or body control • Changing emotions (crying easily or mood swings, sometimes for no reason) • Difficulty swallowing (dysphagia) • Aphasia or slowed or slurred speech • Changes in sight, touch, movement, and thought • Urinary frequency, urgency, or incontinence • Loss of bowel control or constipation Rehabilitation starts at once. The person may depend in part or totally on others for care. The health team helps the person regain the highest possible level of function (Box 28-7). • Expressive aphasia (motor aphasia, Broca’s aphasia) is difficulty expressing or sending out thoughts. Thinking is clear. The person knows what to say but has difficulty speaking or cannot speak the words. There are problems speaking, spelling, counting, gesturing, or writing. The person may: • Omit small words such as “is,” “and,” “of,” and “the.” • Speak in single words or short sentences. “Walk dog” can mean “I will take the dog for walk” or “You take the dog for a walk.” • Put words in the wrong order. Instead of “bathroom,” the person may say “room bath.” • Think 1 thing but say another. The person may want food but asks for a book. • Call people by the wrong names. • Produce sounds and no words. • Receptive aphasia (Wernicke’s aphasia) is difficulty understanding language. The person has trouble understanding what is said or read. People and common objects are not recognized. The person may not know how to use a fork, toilet, cup, TV, phone, or other items. Parkinson’s disease is a slow, progressive disorder with no cure. Movement is affected. Persons over the age of 50 are at risk. Signs and symptoms become worse over time (Fig. 28-14). They include: • Tremors—often start in the hand. Pill-rolling movements—rubbing the thumb and index finger—may occur. The person may have trembling in the hands, arms, legs, jaw, and face. • Rigid, stiff muscles—in the arms, legs, neck, and trunk. • Slow movements—the person has a slow, shuffling gait. • Stooped posture and impaired balance—it is hard to walk. Falls are a risk. • Mask-like expression—the person cannot blink and smile. A fixed stare is common. Symptoms usually start between the ages of 20 and 40. The risk increases if a family member has MS. Signs and symptoms may include: • Blurred or double vision; blindness in 1 eye • Muscle weakness in the arms and legs • Balance and coordination problems • Tingling, prickling, or numb sensations • Partial or complete paralysis • Concentration, attention, memory, and judgment problems • Problems with sexual function MS can present in many ways. For example: • The symptoms last for a few weeks or a few months. The symptoms gradually disappear with partial or complete recovery. The person is in remission. At some point, symptoms flare up again (relapse). • The person’s condition gradually declines with more and more symptoms. There are no remissions. • Symptoms become worse. More symptoms occur with each flare-up. The person’s condition declines.
Caring for Persons With Common Health Problems
Key Abbreviations
Cancer
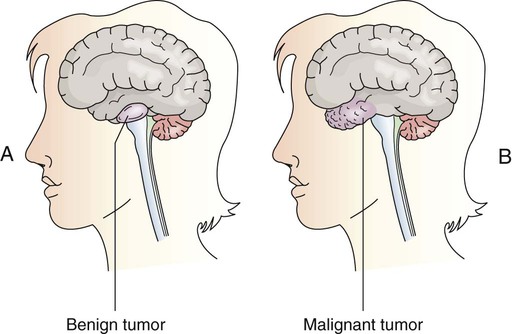
A, A benign tumor grows within a local area. B, A malignant tumor invades other tissues.
Cancer Risk Factors
Cancer Treatment
The Person’s Needs
Musculo-Skeletal Disorders
Arthritis
Osteoarthritis (Degenerative Joint Disease).
Rheumatoid Arthritis.
Osteoporosis
Fractures
Hip Fractures.
Loss of Limb
Nervous System Disorders
Stroke
Aphasia
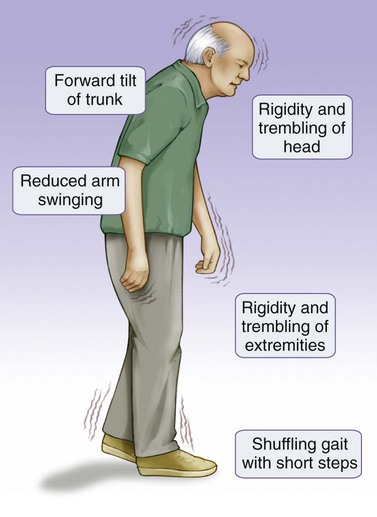
Parkinson’s Disease
Multiple Sclerosis
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nurse Key
Fastest Nurse Insight Engine
Get Clinical Tree app for offline access