Chapter 33. Caring for a child with a neurological disorder
Joanna Smith and Catherine Martin
LEARNING OUTCOMES
At the end of reading this chapter you will be able to:
• Outline the overall structure and function of the nervous system.
• Understand the general principles of caring for a child and family, where the child has a neurological disorder.
• Appreciate the range of neurological disorders in childhood and the potential impact on the child and family.
• Describe the common neurological disorders of childhood.
Introduction
Disorders of the nervous system are an important group of childhood conditions; central nervous system malformations account for approximately 75% of fetal deaths and 40% of deaths within the first year of life (Padgett 2006). Approximately 15–20% of hospitalised children have a neurological problem either as the sole or associated complaint. Diseases of the neurological system have a profound effect on the lives of the child and family and are probably the most disruptive of all ailments. Caring for the child with a nervous system disorder and their families is challenging because the outcome is often uncertain, many disorders are rare and the family will have expert knowledge of the child’s needs, which can lead to frustration for parents and feelings of inadequacy for healthcare professionals. Traditional models of care focusing on the disease process (illness, dependence and treatment) are inappropriate. Although key principles can be applied, care must be individually designed, have a developmental focus and be influenced by encouraging the child to reach their full potential.
The role, structure and function of the nervous system
The nervous and endocrine systems are the main regulatory systems of the body. The nervous system is the most rapid means of maintaining homeostasis, which is achieved by reacting and responding to internal and external stimuli. The nervous system is descriptively divided into the central nervous system (CNS) and the peripheral nervous system (PNS) (Sugerman 2006). The CNS consists of the brain, the control centre for the entire nervous system and the spinal cord. The PNS consists of the nerve networks, which link the CNS with the periphery.
The PNS has two main subdivisions, the somatic nervous system (SNS) and the autonomic nervous system (ANS). Actions carried out by the SNS are both voluntary and involuntary with sensations being perceived consciously, whereas actions carried out by the ANS are involuntary and not usually perceived consciously. The ANS has sympathetic and parasympathetic divisions and is primarily concerned with the innervation and control of visceral organs, smooth muscles and secretory glands. Where there is both sympathetic and parasympathetic nerve innovation their actions have an antagonistic effect, for example sympathetic activity increases the force of contraction of cardiac muscle and the heart rate, whereas parasympathetic activity reduces the force of contraction and decreases the heart rate.
Development of the nervous sytsem
Many neurological problems in infancy may be a result of a malformation that has occurred during embryological development (Padgett 2006). The ectoderm, one of the three primary germ layers, forms nervous tissue, the ears, eyes and epidermis. The first obvious sign of nervous system development is during the 3rd week of embryonic life when the dorsal midline of the ectoderm thickens to form the neural plate (Padgett 2006). The lateral margins of the plate become elevated resulting in a midline depression known as the neural groove. Eventually the folds become apposed and fuse together creating the neural tube. The neural tube is completely closed by the end of the 4th week of embryonic development and becomes the CNS (Longstaff 2005). By the 5th week of gestation the rostral portion of the neural tube enlarges and differentiates into the forebrain (cerebrum), midbrain and hindbrain (pons, cerebellum and medulla oblongata) (Fig. 33.1).
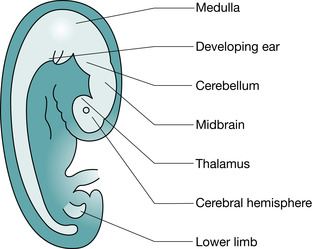 |
| Fig. 33.1 Representation of the brain and spinal cord at 5 weeks’ gestation. |
In addition to structural developments, neuroepidermal cells increase in numbers. They are the precursors of both the supporting cells and the nerve cells and begin to organise themselves into zones. This results in the typical appearance of the brain: an outer layer of grey matter (cell bodies) and an inner layer of white matter (nerve tracts). Epidermal cells, precursors of both supporting (glial) cells and specialist (nerve) cells, increase in number and migrate through the layers of previously formed cells, adding to the expanding cerebral cortex. During the final stages of specialisation, nerve cells lose the ability to divide, and therefore do not increase in number after birth. Glial cell proliferation and nerve myelination increase the weight and size of the brain, particularly during the 1st year of life. Nerve myelination occurs from 22 weeks of gestation and is probably not complete until adult life (Padgett 2006).
Cells of the nervous system and their function
The two cellular components, the neuralgia (glial cells) and the neuron (nerve cells), are unique to the nervous system. Glial cells form the connective tissue of the nervous system; astrocytes provide mechanical support and help maintain the blood–brain barrier; microglia correspond to brain phagocytes; oligodendroglia and Schwann cells form myelin in the CNS and PNS respectively; and ependymal cells form the epithelial linings.
The neuron has a specialised structure that facilitates the transmission of electrical impulses (Fig. 33.2). A stimulus of sufficient strength applied to a dendrite receptor site generates a nerve impulse, which is transmitted along the dendrite to the cell body. The impulse exits via the main axonal process (nerve fibre) ending at the terminal boutons. These contain chemical transmitters capable of stimulating adjacent neurons or affector organs. Generating and conducting a nerve impulse is based on the neuron’s ability to maintain a difference in the ion concentration outside and inside the cell membrane. Disruption of the ion concentration causes an ionic current flow, which is conducted along the entire neuron, is independent of any further stimulus and is unidirectional. The speed of the nerve impulse increases if (Longstaff 2005):
• body temperature increases
• the diameter of the fibre increases
• myelin is present.
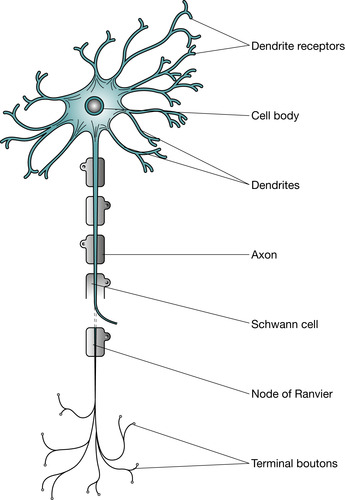 |
| Fig. 33.2 A typical motor neuron. |
Information passes between neurons at junctions (synapses). When a nerve impulse arrives at the terminal bouton, neurotransmitters such as noradrenaline or acetylcholine are released. These cross the synapse and bind with the receptor site on the adjacent dendrite. Calcium ions are necessary to facilitate this process. Neurotransmitters stimulate or inhibit postsynaptic dendrites, allowing impulses either to proceed or be inhibited. Once the neurotransmitter binds with the receptor site it is rapidly deactivated by enzymes in the postsynaptic junction.
Anatomy of the brain
The brain consists of the cerebrum (two cerebral hemispheres), diencephalon, brainstem and cerebellum (Fig. 33.3). The hemispheres are joined at the base by the corpus callosum (a sheet of nerve fibres allowing communication between the hemispheres).
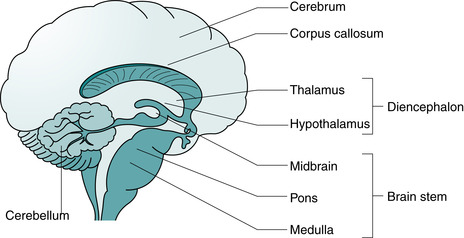 |
| Fig. 33.3 Cross-sectional view of the brain. |
The cerebrum is by far the largest part of the brain, and is divided into important functional areas (Fig. 33.4). Specific areas of the cortex perform specific functions (Fitzgerald & Folan-Curran 2002):
• The frontal lobe contains the primary motor cortex responsible for controlling movement, the speech area and higher functions including personality and behaviour.
• The parietal lobes contains the primary somatosensory cortex where sensations such as touch, pressure, pain and temperature are consciously perceived.
• The occipital lobe contains the visual cortex.
• The temporal lobes contain the auditory cortex, and areas involved in memory and emotions.
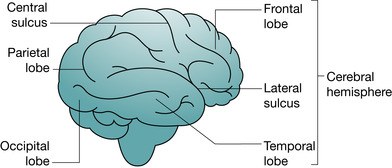 |
| Fig. 33.4 Major subdivisions of the cerebral hemispheres. |
Due to the cross over (decussation) of the nerve fibres at the medulla oblongata each hemisphere communicates with the opposite side of the body.
The diencephalon contains several specialist areas, with the two most important being the thalamus and hypothalamus. The thalamus is a relay and integration centre. The hypothalamus coordinates homeostatic mechanisms and has autonomic, neuroendocrine and limbic functions.
The brainstem collectively describes the midbrain, medulla oblongata and the pons. The midbrain contains part of the auditory system. Most nerve fibres from the body transcend the medulla and midbrain, which function as important relay and integration centres. Although anatomically the brain stem is a relatively small component of the brain, its importance cannot be underestimated. It contains many nuclei and tracts that are essential to key vital body functions, for example the medulla contains nuclei that regulate blood pressure, respiration, maintenance of arousal and initiation of sleep. Like the medulla, the pons contains many functional structures but primarily acts as a relay centre between the cerebrum and cerebellum.
The cerebellum sits in the base of the cranial cavity in an area known as the posterior fossa. The cerebellum is important in relation to the coordination of motor activities functions such as tone and posture, and operates at an unconscious level. Unlike the cerebral cortex, responses of the cerebellum affect the same side of the body (ipsilateral).
The ventricular system
The ventricular system is a network of connected chambers or ventricles deep within the brain which contain cerebrospinal fluid (CSF). There are four chambers: two lateral ventricles situated within the cerebral hemispheres, the third ventricle situated in the diencephalon and the fourth ventricle situated between the brainstem and the cerebellum. The fourth ventricle tapers at its base and becomes the very narrow central canal of the spinal cord.
CSF flows constantly beginning in the lateral ventricles before flowing into the third ventricle, and continuing via the aqueduct of Sylvius to the fourth ventricle. CSF leaves the fourth to circulate around the brain and spinal cord via the subarachnoid space (Fig. 33.5). CSF is reabsorbed into the bloodstream via capillaries on the surface of the cerebral hemispheres.
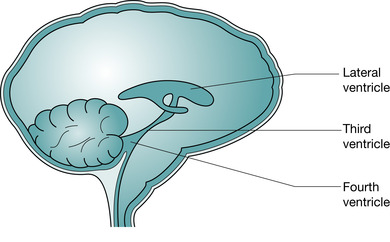 |
| Fig. 33.5 Cerebrospinal fluid flow through the ventricular system. |
CSF helps maintain the cerebral chemical environment by supplying nutrients and removing toxic substances, is a shock absorber, contributes to maintaining the blood–brain barrier, and gives the brain buoyancy. CSF has high sodium, chlorine and bicarbonate levels, low potassium, urea, glucose and amino acid levels, and a negligible protein content (Sugerman 2006).
Blood supply
The brain requires a continual input of glucose and oxygen, with 20% of the total cardiac output reaching the brain each minute (Sugerman 2006). The internal vertebral and carotid arteries, and their subsidiaries ensure the brain has a rich blood supply. These vessels form a system of interconnecting arteries in the base of the brain, known as the circle of Willis. The physiological principle behind the circle of Willis is that in the event of damage to one of the arteries supplying the brain there is the potential for compensation from the communicating arteries thus offering some protection from severe ischaemic damage.
Venous blood primarily returns to the circulation via the superficial veins that drain into the venous sagittal sinus that eventually flows into the internal jugular vein. The deep veins of the cerebral hemispheres drain into the vein of Galen and then into the sagittal sinus.
The composition of the brain’s extracellular fluid needs to be regulated because circulatory chemicals are toxic to neurons. This is achieved by the blood–brain barrier, a complex process that is the consequence of specific characteristics of the cerebral capillaries resulting in a highly selective exchange of substances across their endothelial end plates.
Protection and coverings
The brain is supported and protected by the skull and the membranous coverings collectively known as the meninges. The bones of the skull are separated at birth, allowing for brain moulding during delivery and rapid growth within the 1st year of life. Complete ossification occurs at about 8 years of age, and the sutures (Fig. 33.6) cannot be separated even in the presence of raised intracranial pressure after about 12 years of age (Padgett 2006).
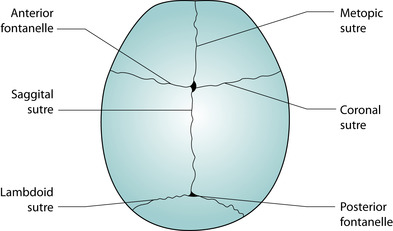 |
| Fig. 33.6 Sutures of the skull. |
Neuron regeneration
The traditional approach to neuroanatomy and physiology associates discrete body functions with specific brain structures (Stephenson 1996). Recent studies suggest latent areas within the brain may be able to assume the functions of damaged areas (Rose et al 1997). In addition, it was presumed that because neuron cell bodies do not have centrioles and the meiotic spindles that are necessary for cell division, there is little capacity to repair and regain function following damage. However, neurons can survive damage, regenerate new axons and form new synaptic connections (Stephenson 1996). The process known as reactive synaptogenesis may result in the recovery of function, but can also result in the development of abnormal connections with abnormal recovery.
 Activity
Activity
 Activity
ActivityRevisit your knowledge and add more depth by accessing the Evolve website:
The following textbooks and web sites may be useful
• Crossman AR, Neary D 2000 Neuroanatomy – an illustrated colour text, 2nd edn. Churchill Livingstone, Edinburgh
• Fitzgerald MJT, Folan-Curran J 2002 Clinical neuroanatomy and related neuroscience, 4th edn. WB Saunders, Edinburgh
• Brain source; aimed at sharing neuroscience knowledge http://www.brainsource.com/
• Encyclopedia of Life Sciences; comprehensive coverage of a range of topics including neurosciences http://www.mrw.interscience.wiley.com/
Overview of neurological disorders affecting children
The range of neurological disorders in childhood is vast, terminology is complex and many children who present with a neurological dysfunction may never have a definitive diagnosis. A lack of diagnosis is particularly difficult and can be frustrating for the child and family. It is vital for disorders where there is a potential genetic mode of inheritance that the child and family are referred for genetic counselling to assist the parents in decisions relating to planning future children. The outcome of neurological disorders is extremely variable. It is essential the child and family are viewed as unique with individual needs when planning care. The diversity of neurological conditions are presented in Table 33.1.
 www
www
 www
wwwDevelop your knowledge of these conditions by accessing the following websites:
• Association for Spina Bifida and Hydrocephalus: http://www.asbah.org.uk
• Association for Tuberous Sclerosis: http://www.tuberous-sclerosis.org.uk
• Children’s Hemiplegia and Stroke Association: http://www.hemikids.org
• Meningitis Trust UK: http://www.meningitis-trust.org.uk
• Scope (focuses on providing supporting for people with disabilities, primarily with cerebral palsy): http://www.scope.org.uk
• Muscular Dystrophy Campaign: http://www.muscular-dystrophy.org/
• Child Brain Injury Trust: www.cbituk.org/
• Headlines Children with Craniosynostosis: www.headlines.org.uk
| Features | Example | |
|---|---|---|
| Congenital malformations | Disruption to normal CNS development, usually occurs early in gestational period Often multifactorial genetic transmission | Hydrocephalus Agenesis of the corpus callosum Microcephaly |
| Neurocutaneous disorders | Errors occurring in early ectodermal cell proliferation results in a group of disorders, which present with combined CNS, ophthalmic and skin abnormalities | Tuberous sclerosis Sturge–Weber syndrome |
| Vascular disorders | A diverse group of disorders with various aetiologies from structural anomalies to spontaneous intracranial bleeds | Arteriovenous malformations Intracranial arterial aneurysms Moyamoya disease |
| CNS infections | Common cause of acute neurological disorders Despite improved preventative programmes through vaccination and improved antimicrobial agents remain a challenge with significant morbidity | Meningitis Intracranial abscesses Encephalitis (measles, herpes simplex, mumps) |
| Neoplastic disorders | Most common solid tumours in children Often difficult to treat | Medulloblastoma Astrocytoma Brainstem glioma Craniopharyngioma |
| Progressive degenerative disorders | Includes the many neurometabolic disorders, which although individually rare, collectively are an important group of disorders Most follow an autosomal recessive inheritance pattern Two major groups are the neuronal storage diseases and the leucodystrophies | Tay–Sachs disease Battens disease Niemann–Pick disease Krabbe’s disease |
| Non-progressive brain damage | Persistent disorder as a result of brain insult during early development The underlying problem is static but subsequent development is affected | Cerebral palsy |
| Neuromuscular disorders | Normal muscle functioning is dependent upon effective muscle and nerve functioning. Children with this group of disorders present with hypotonia and increasing muscle weakness | Duchenne muscular dystrophy Myasthenia gravis Guillain–Barré |
| Learning disabilities | A wide range of learning disabilities exist from very specific skill deficiencies to complex disorders affecting the ability to carry out activities of living and achieve independent living Aetiology is often due to hereditary and environmental factors | Fragile-X syndrome Down syndrome Autism Asperger’s syndrome |
Principles of caring for a child with a cerebral dysfunction
Understanding the principles that underpin the management of the child with both acute and long-term neurological dysfunction is essential if care delivery is to be safe and appropriate. Neurological disorders have a unique effect and care must be based on assessment and meeting individual needs. Therefore the general principles of care need to be adapted to each situation, and the child and family’s needs. Seizure management is covered in Chapter 23.
Diagnostic procedures
Diagnostic procedures are vital in order to: assist the clinician to establish, where possible, the correct diagnosis; determining the potential prognosis for the child; and to monitor disease progression and/or the effects of treatments.
The child and family require detailed explanation and effective preparation prior to investigative procedures. Consent must be obtained. The type of diagnostic investigations will vary depending on the child’s presentation but may include:
• blood profiling, including urea and electrolytes, metabolic and immunological assays, and genetic screening
• lumbar puncture performed to collect CSF samples in order to detect the presence of bacteria or tumour deposits, and the measurement of CSF pressure. Performing a lumbar puncture in a child with a high intracranial pressure may cause brainstem compression with fatal consequences
• neuroimaging; ultrasound, X-rays, computerised axial tomography (CT), magnetic resonance imaging (MRI)
• specialised physiological imaging techniques such as positron emission tomography (PET) and single-photon computed emission tomography (SPECT), assist with evaluating cerebral metabolic functioning and cerebral blood flow
• cerebrovascular studies such as angiography, used to identify cerebrovascular abnormalities such as aneurysms and arteriovenous malformations
• electroencephalogram (EEG) records the electrical activity of the brain and is primarily used to detect changes in brain activity during seizures. Often used as a continuous monitoring procedure with video recording to correlate a child’s presentation with EEG changes (video telemetry)
• electromyography (EMG) conduction studies are used to measure electrical activity and velocity times in muscle fibres. Particularly useful in assisting in the diagnosis of neuromuscular and peripheral nerve disorders
• muscle biopsies measure a range of muscle enzymes. Useful in identifying whether a problem is neurogenic or myogenic in origin, assisting in the diagnosis of neuromuscular conditions.
Some of these procedures, such as PET and SPECT, are only available in specialised centres.
 Activity
Activity
 Activity
ActivityCommon imaging techniques are now widely available; therefore all nurses must have appropriate knowledge of these procedures associated care related to these procedures:
Think about the advantages, disadvantages and care needs of the child who requires an X-ray, CT scan or MRI scan.
What strategies would you use to ensure a 2-year-old child successfully undergoes a CT scan?
You might want to add more depth to your knowledge by accessing the Evolve website:
• file chapter 9 imaging techniques.
Raised intracranial pressure
Intracranial pressure (ICP) is the pressure exerted by the cranial contents on the skull. Typical values in older children are 5–15 mmHg and 3–7 mmHg in infants and young children (Chitnavis & Polkey 1998). The rigidity of the skull results in the total intracranial volume being fixed. The intracranial contents (brain, CSF, and blood) must be maintained in a state of equilibrium. Therefore an increase in volume in one component must be reciprocated by a reduction in volume in another component, known as the Monro–Kellie doctrine (Chitnavis & Polkey 1998), which can be represented by the following equation:
However, there is little ability of the brain to significantly reduce any of these components and an increase in overall volume results in a rise in ICP (Fig. 33.7). Raised intracranial pressure (RICP) is usually described as an ICP above 20 mmHg sustained for 5 minutes or more (Miller & Dearden 1992). Causes include:
• conditions which increase the brain volume:
• space occupying lesions such as tumour, abscess, haematoma
• cerebral oedema for example following traumatic brain injury or cerebral infection
• conditions which increase the blood volume or blood flow:
• obstruction to venous outflow
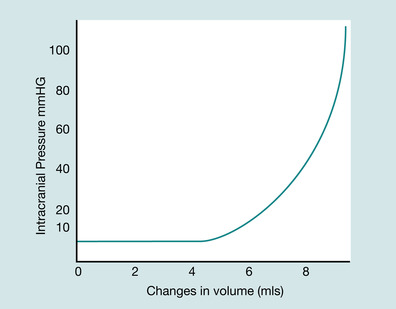 |
| Fig. 33.7 Volume/pressure curve. |
The signs and symptoms of RICP include (Hazinski et al 1999):
• alteration in conscious levels; irritability, lethargy, confusion, decreased responsiveness
• dilated pupils, decreased response to light
• abnormal motor activity or reflexes
• headaches, nausea and vomiting
• Cushing’s response (increased blood pressure with a compensatory bradycardia), bradycardia on its own, apnoea. These are late and ominous signs.
The signs and symptoms of RICP in an infant, prior to fusion of the skull sutures, usually occur late because increased volume forces the membranes between the skull bones to splay, accommodating pressure changes. There will be more insidious signs such as irritability, poor feeding, general developmental delay, large and tense anterior fontanelle even when the infant is in the sitting position, and increased head circumference (Brett & Harding 1997a).
Once the intracranial pressure starts to rise a cycle of events occurs: ICP increases, cerebral blood flow (CBF) decreases, leading to tissue hypoxia resulting in cerebral vasodilation and oedema, causing further increases in ICP. The brain will shift from the area under pressure to an area of less pressure, resulting in compression, traction and shearing of brain structures. Eventually, downward brain shift occurs, resulting in brainstem herniation with vital centres becoming compressed. Management of RICP is based on the need to prevent cerebral ischaemia by maintaining cerebral perfusion pressure (CPP) between 70 and 80 mmHg (Rosner & Daughton 1990), with care best provided in paediatric intensive care unit.
 Evidence-based practice
Evidence-based practice
 Evidence-based practice
Evidence-based practiceThere are evidence-based guidelines relating to the management of RICP as a consequence of significant brain injury in both children and adults (Adelson et al., 2003 and Bullock et al., 2000). The principles within these guidelines include:
• ventilate and maintain oxygenation, aim for a PaCO 2 between 30 and 35 mmHg and PaO 2 between 90 and 100 mmHg. Hyperventilation is not a recommended treatment for TBI but may be of value for brief periods where the PaCO 2 is elevated and there is associated acute neurological deterioration, such as acute rises in ICP
• minimising the brain’s metabolic needs and preventing activities which normally produce transient rises in ICP by providing adequate sedation, analgesia and paralysis. No specific evidence is currently available relating to the best sedative, analgesia or neuromuscular blocking agent in the management of head injury. Choice will depend on local guidelines and practices. The use of sedation, analgesia and paralysis will limit the ability to perform full neurological assessments
• maintaining an adequate systemic mean arterial pressure, above 75 mmHg for children over 10 years of age and above 65 mmHg for those less than 10 years of age in order to ensure an adequate CPP.
• this is achieved by appropriate fluid resuscitation and the administration of inotropic drugs. An inotrope is an agent which alters the force or energy of cardiac muscular contractions. This group of drugs is useful for resuscitation of seriously ill patients, and for the treatment of hypotension in intensive care settings. In these situations inotropes such as dopamine or dobutamine are administered by continuous infusion. Fluid resuscitation must be judicious due to the potential of increasing cerebral oedema if over hydration occurs
• maintaining CPP above 60 mmHg for children over 10 years of age and above 50 mmHg for those less than 10 years of age. Maintaining an adequate mean arterial pressure will require the use of inotropic support
• maintaining normal electrolyte balance with precise fluid management
• monitoring and record ICP levels and wave patterns; identify ‘plateau’ waves early. ICP above 20 mmHg will require active treatment such diuretic therapy. Mannitol 20% is the diuretic of choice and the usual dose is 0.25–0.5 g/kg. Monitor serum osmolarity with mannitol use and maintain a level of less than 320 mOmols/L
• decompression surgery may be indicated if the child has an extremely high ICP and high blood pressure due to generalised cerebral oedema but the child’s brain is likely to recover
• optimising cerebral venous return by maintaining the head at an angle of 30° and position the head in the midline to prevent constriction of the blood vessels
• maintain normothermia
• monitor EEG in order to detect seizure activity and ensure prompt treatment of seizures.
Neurological assessment
Accurate neurological assessment and skilled observations are essential if changes in neurological function are to be detected. The purpose of a neurological assessment includes (Hickey 2003a):
 Reflect on your practice
Reflect on your practice
• identifying the child’s normal abilities and developmental stage
• providing a baseline record of the child’s neurological status at the time of admission
• identifying the presence and effects of neurological dysfunction
• detecting life-threatening situations
• identifying changes promptly through serial observations
• influencing management decisions by monitoring overall improvements or deteriorations in the child
• assisting in the prediction of the eventual outcome of the neurological insult.
 Reflect on your practice
Reflect on your practiceThink about the last time you performed neurological observations on a child:
• Why were the observations being undertaken?
• How frequently were the observations being undertaken? Why?
• How and why did you apply a painful stimuli?
• How and why did you act on any changes in the child’s condition?
Neurological observations include: assessment of conscious levels, pupillary reactions, motor functioning and other parameters including the presence of seizures and changes to vital signs. The frequency of undertaking observations will depend on the initial assessment, the stability of the child and the underlying problem. In the acute situation half- to 1-hourly observations seem to be the norm (Ferguson-Clark & Williams 1998). Unless a full assessment is carried out, unconsciousness cannot be distinguished from normal sleep.
Assessment of consciousness
Consciousness is a state of awareness and in general can be thought of as two components – arousal and wakefulness – and is a sensitive indicator of neurological functioning (Hickey 2003a). The first and the most frequently used numerical scale for assessing conscious levels is the Glasgow Coma Scale (GCS) (Teasdale & Jennett 1974). It was developed in the 1970s to reduce the subjectivity and ambiguity when assessing a patient’s conscious level. The Glasgow Coma Scale (GCS) assesses three parameters, eye opening, verbal response and motor response, with a numerical score given for the best response within each parameter (Table 33.2).
| Parameter | Score | Components |
|---|---|---|
| Eye opening | 4 | Eyes open spontaneously in response to normal environmental activities |
| 3 | Eyes open in response to direct commands | |
| 2 | Eyes open in response to a painful stimulus | |
| 1 | Absence of eye opening despite application of a painful stimulus | |
| Verbal response | 5 | Answers appropriately to questions |
| 4 | Converses but confused | |
| 3 | Makes little sense | |
| 2 | Incompressible sounds | |
| 1 | No verbal response despite the application of a painful stimulus | |
| Motor response | 6 | Obeys commands |
| 5 | Localisation of a painful stimulus and purposefully moves in an attempt to locate the stimulus and remove it | |
| 4 | Withdrawal from the painful stimuli in an attempt to move away from the stimulus but it is not a purposeful movement | |
| 3 | Flexion response to a painful stimulus | |
| 2 | Extension to a painful stimulus | |
| 1 | Flaccidity, there is no detectable movement or change in tone of the limbs despite repeated and varied stimulation |
The GCS has undergone several adaptations for use in children, including the James’ adaptation (James & Trauner 1985) and the Adelaide Scale (Reilly et al 1988). The National Paediatric Neuroscience Benchmarking group (Tatman et al., 1997 and Warren, 2000) and the National Institute for Clinical Excellence (NICE 2007) advocate using the James’ adaptation because it is easy to use, the scoring system (a maximum of 15 and minimum of 3) is internationally recognised and it takes into account the child’s developmental stage. The addition of the grimace score makes it suitable for use in intensive care settings (Warren 2000). Spontaneous eye opening in response to normal environmental activities achieves a maximum score of 4, indicating that the arousal mechanisms in the brain stem are functioning. The normal verbal response will depend on the linguistic and cognitive developmental stage of the child and, where possible, should be ascertained from the child or carer prior to undertaking the first assessment (Table 33.3). The final component of the GCS assesses the ability of the child to respond to an instruction that requires the child to undertake a motor action. This requires the child to have an appropriate level of understanding in order to interpret and act on the instructions given. In babies or young infants that do not have the cognitive ability to response to instructions a maximum score of 6 would be recorded if there are normal spontaneous movements.
| Score | Verbal response | ||
|---|---|---|---|
| Infant/young child | Older child/adult | Grimace – all ages | |
| 5 | Alert, babbles, coos/uses words or sentences/usually ability | Orientated | Spontaneous normal facial/oro-motor activity |
| 4 | Less than usual ability or spontaneous irritable cry | Confused | Less than usual facial/oro-motor spontaneous activity or only response to touch stimuli |
| 3 | Cries inappropriately | Inappropriate words | Vigorous grimace to pain |
| 2 | Occasional whimpers/moans | Inappropriate sounds | Mild grimace to pain |
| 1 | No response | No response | No response |
If a child does not respond to an auditory stimulus or light tactile pressure, and therefore has not achieved the maximum score, the continuation of the assessment requires the application of a painful stimulus. When assessing the motor component of the GCS, it is important to use a central stimulus to ascertain whether the child can locate the site of the stimulus, for example applying pressure over the supraorbital area (Teasdale & Jennett 1974). Sternal rub, although a central stimulus, can potentially damage soft tissues (Hickey 2003a). Nail bed pressure may elicit a flexion reflex response and can be misinterpreted as an attempt to localise to pain. Supraorbital pressure is not appropriate to elicit eye opening because it causes grimacing, and simultaneous eye closing. Under 6 months the normal motor response to painful stimulation is flexion (Brett & Kaiser 1997).
Summation of the three components of the GCS provides a summary of the child’s conscious state and can act as a quick reference guide when reviewing the child’s condition (Watson et al 1992). The summation ranges in value from 3 to 15, with 15 indicating full consciousness. The score becomes lower as the degree of neurological impairment increases. Coma is usually defined as a score of 8 or less (Kraus et al 1987). Summation of the GCS can conceal the whole picture, and may not be accurate in terms of predicting long-term outcome of the neurological injury particularly following traumatic brain injury (McNett 2007). However, in an acute intracranial catastrophe all three components of the GCS are usually depressed.
Motor function
Evaluating limb responses can assist in determining the site of brain damage; specific deficits will correlate to the specific area of brain damage. Damage to the motor cortex and cerebellum will result in abnormalities in motor function. Assessing motor function is not the same as assessing the motor response in the GCS. The assessment of motor function aims to provide an overview of the function of each of the four limbs independently, in terms of muscle strength, muscle tone, posture and the coordination of movements and whether movements are spontaneous or in response to painful stimuli or flaccid (Peters 2007). Abnormal posture and movements should be documented. The neonate’s normal response to stimulation is flexion (Brett & Kaiser 1997).
Pupil reactions
Assessment of pupil function provides valuable insights into the physiology of the brainstem. The response of the pupils to light is dependent on intact cranial nerves II and III, which transmit nerve impulses from the retina to the midbrain and from the midbrain to the pupillary muscles, respectively. Assessment of pupils should include size, equality and reactivity to light (Hickey 2003a). The normal response to a direct light stimulus is an immediate brisk constriction of the pupil, and a brisk dilation of the pupil once the light source is removed (Hickey 2003a). Although each eye is examined independently, the response should be observed in both eyes. Light directed into one eye will constrict the pupil in the opposite eye due to the consensual light reflex. The pupillary response is graded and recorded descriptively in terms of brisk, sluggish or non-reactive (fixed). The size of the pupil is either recorded as pinpoint, small, moderate or dilated, or on a scale ratio of 1:8. Pupils are usually between 2 and 6 mm in size, but there may be slight discrepancies between the two pupils.
The assessment of the pupil responses is important because:
• pupil responses can be undertaken on patients who are receiving anaesthetic or paralysing agents
• extremely small pupils can indicate narcotic overdose or direct lower brain stem compression
• a large pupil or unequal pupils usually indicate compression of the midbrain and consequently the oculomotor nerve
• a dilated fixed pupil is an ominous finding and suggestive of a terminal state (Hickey 2003a). These findings should arouse immediate concern and be reported immediately to medical staff.
• an irregular or oval pupil may indicate raised intracranial pressure and be the first sign of oculomotor nerve compression due to transtentorial herniation
• drugs that either constrict or dilate the pupils should be accurately recorded.
Vital signs
Alterations in vital signs can indicate pathophysiological changes within the brain, particularly the brainstem. Cardiovascular observations are particularly important because of the relationship between cerebral haemodynamics and cerebral functioning (Hickey 2003a). Compromise to cerebral blood flow will result in a vasomotor response, with blood being diverted from other body systems in order to maintain adequate cerebral perfusion. The resultant rise in arterial blood pressure is known as Cushing’s reflex or response (Hickey 2003a). Tachycardia will initially occur as a result of mild hypoxia. Significant compromises to cerebral blood flow cause further increases in blood pressure resulting in a compensatory bradycardia, suggestive of a dangerously high intracranial pressure and usually denotes an intracranial catastrophe is impending.
Changes in respiratory rate and rhythm can occur with neurological dysfunction. Alterations to normal respirations such as hyperventilation, shallow breathing or irregular breathing should raise concerns. Rapidly expanding lesions such as intracranial haemorrhage, direct medulla damage or brainstem herniation are likely to cause respiratory arrest (Hickey 2003a).
Alterations in body temperature, both hypo- and hyperthermia, can be manifestations of neurological impairments. Hyperthermia is probably more common (Hickey 2003a) and can be due to infective and non-infective conditions. Central fever due to neurogenic aetiologies are typically associated with brain tumours, trauma and following neurosurgery.
Additional components of the neurological assessment should include observation of the adequacy of the cough and gag reflex, which can become depressed following widespread brain damage. Brain insults have the potential to cause seizures requiring appropriate monitoring and management because of the resultant hypoxia, which will compound existing problems.
Care of the unconscious child
Unconsciousness is a lack of awareness of one’s self, the environment, an impairment of cognitive functioning and an inability to respond to sensory stimuli (Hickey 2003b). There is a myriad of neurological conditions that result in unconsciousness, with the depth and duration lasting for seconds, for example during a seizure, to months, for example following major head trauma.
 Activity
Activity
 Activity
ActivitySally is 14 years old and has suffered a cerebrovascular accident necessitating emergency craniotomy and resulting in a prolonged period in paediatric intensive care. She is now stable and able to maintain her own airway. Her nutrition is primarily maintained via gastrostomy feeding. She remains unresponsive and dependent on carers for all her needs. Her family, primarily her mother, although not resident, is actively involved in Sally’s care.
• Identify Sally’s actual and potential problems.
• Write a detailed nursing care plan outlining how Sally’s needs will be met.
Children with impaired levels of consciousness and who are unable to maintain their own airway are at risk of hypoxia and hypercarbia, with potential respiratory failure and therefore will require intensive care (Hazinski et al 1999). However, many children who have impaired levels of consciousness do not require intensive care facilities but are dependent on the healthcare team to meet their needs. The aims of caring for these children are: to ensure activities necessary to sustain life are maintained, prevent complications relating to immobility, maximise the restoration of functions and offer support to the family. Table 33.4 outlines the needs of the child with impaired conscious levels in relation to maintaining essential activities of daily living and preventing complications.
| Actual/potential problems | Nursing interventions |
|---|---|
| Altered neurological functioning due to cerebral dysfunction | Monitor neurological functioning through regular assessment Manage alterations in sleep patterns and periods of irritability through structuring activities appropriately, having planned rest periods, using relaxation techniques such as aromatherapy and massage Drugs such as melatonin may be prescribed for sleep disturbances – review their use regularly Ensure stimulation activities are planned and appropriate for the child’s age and condition Assess and manage pain appropriately |
Risk of altered respiratory function due to underlying cerebral dysfunction, inability to maintain airway and immobility Potential problem of atelectasis and chest infection | Assess respiratory function and identify risk of airway obstruction, ensure position does not compromise the airway, use airway aids and suctioning as appropriate Appropriate monitoring such as respiratory rate and effort, colour, peripheral perfusion and pulse oximetry Assess gag and swallow reflexes, in conjunction with a speech and language therapist, keep the child ‘nil by mouth’ until these reflexes have returned Ensure regular chest physiotherapy, ensure position changes and passive movements are incorporated into care activities Monitoring for signs of chest infection by recording temperature and changes in the amount and colour of secretions |
Unable to maintain nutrition and hydration Potential problems of malnutrition, anaemia, electrolyte disturbances and gastric ulcers | Assess nutritional status, including monitoring of the child’s weight Provide a good nutritional intake by appropriate methods that meet the needs of the child, enteral feeding via a naso-gastric/jejunal tube may be necessary. A gastrostomy tube may be more appropriate if long-term enteral feeding is required Ensure nutritional intake reflects increased calorific intake, liaise with the dietician to ensure the correct composition and volume of feed Monitoring intake and output, observing for signs of under/over-nourishment and dehydration If gag and swallow reflex have been assessed to be adequate and there are no other contraindications oral food and fluids should be encouraged. The re-introduction of oral feeding may need to be supplemented by enteral feeding because neurological problems may result in oral-motor difficulties, reduced alertness and increased fatigability contributing to inadequate nutritional intake Consider the child’s needs in relation to positioning and supportive seating, taste and textures, likes and dislikes, choice of utensils, and effective age appropriate communication |
| Unable to maintain self-care needs | Ensure care is appropriate in meeting individual needs and consider usual family practices in relation to maintaining hygiene needs There needs to be particular emphasis on the assessment of the mucous membranes of the eyes and oral cavity for dryness, take appropriate action to keep clean and moist: • corneal dryness will require instillation of artificial tear drops or gels such as hypromellose drops • protecting the eyes by the use of patching if the child is unable to completely close the eyes Assessing oral hygiene needs and involvement of dental hygienist/dentist as appropriate, ensure frequent teeth brushing, consider the need to use suction techniques to prevent aspiration |
| Potential complications of immobility including: | |
1. Skin breakdown | Assess pressure areas using a recognised child-appropriate assessment tool. Implement preventative measure based on the assessment to ensure the integrity of the skin is maintained |
2. Muscular skeletal deformities; muscle wasting, muscle contractures, peripheral nerve impairment and poor muscle tone | Liaise with the therapy team to establish individual positioning regimens. Principles include maintaining the child’s head in neutral position, with the spine and hips positioning in alignment with the head, maintaining flexion of the limbs and preventing extension of the ankles Ensure staff and child safety by used appropriate moving and handling equipment and techniques Ensure correct positioning is used at all times and use splints where appropriate |
3. Poor circulation and inadequate lung functioning | Undertake passive exercises and regular position changes in order to improve circulation, relieve pressure, facilitate lung expansion, prevent urinary stasis, improve gut mobility and minimise muscle atrophy Anti-coagulant therapy and anti-embolism stockings will be necessary in older children |
4. Infections particularly chest and urine infections | Ensure regular chest physiotherapy, ensure position changes and passive movements are incorporated into care activities Monitoring for signs of chest infection by recording temperature and changes in the amount and colour of secretions Minimising the risk of urine infection; where appropriate nurse the infant child in nappies and older child in pads; ensure meticulous skin care. An indwelling catheter is a potential sources of infection, if required maintain local policies in relation to the care of indwelling catheters and apply the principles of universal infection precautions Assess for the risk of infection by observing colour, smell and concentration of urine and measurement of body temperature |
5. Constipation | Monitor bowel motions and manage constipation appropriately including high-fibre diet or supplements, adequate hydration and use of suppositories as necessary |
Nursing care of the child undergoing neurosurgery
The principles that apply to every child requiring surgery are also important for the child undergoing cranial surgery. The main goals of care are to minimise potential complications of the surgical procedure and effects of the anaesthetic by ensuring the child and family are prepared appropriately and safely for surgery and recovery needs are met. Surgery and anaesthesia disrupt normal functioning and homeostatic mechanisms and are potentially life threatening.
In general there are few specific preoperative requirements. The child will require preoperative blood sampling, including cross-match, because of the potential for blood loss during surgery. The child and family must be prepared for the immediate postoperative period, including the possibility of being nursed in intensive care, the child’s appearance including descriptions of the wound/bandages, drains, facial swelling, and the range and function of monitoring equipment. It is usual practice to undertake skin preparation and hair removal after induction of the anaesthetic. However, it is essential the child and family are prepared for hair removal.
 Activity
Activity
 Activity
ActivityJamie is 6 months old and has been admitted for insertion of a ventricular shunt.
• Write a care plan outlining the principles of the pre- and postoperative care Jamie and his family will require.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
