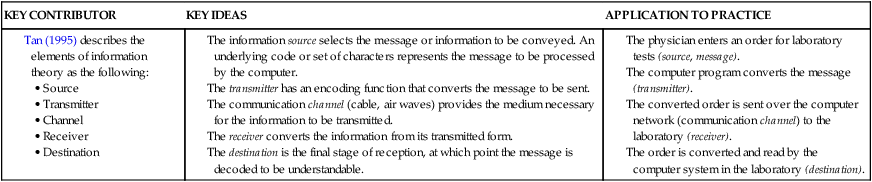
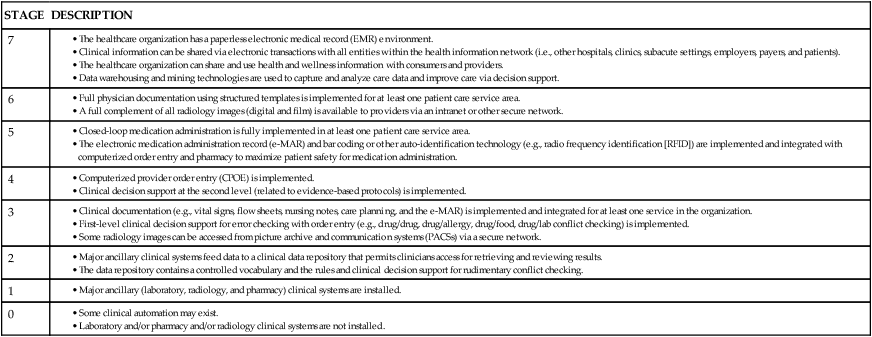
• Articulate the role of several new technologies in patient safety. • Describe the core components of informatics: data, information, and knowledge. • Evaluate a model to change accepted practice into evidence-based practice. • Describe three types of healthcare information technology trends. • Apply one structured nursing terminology to a nursing scenario. • Analyze three types of technology for capturing data at the point of care. • Discuss decision support systems and their impact on patient care. • Explore the issues of patient safety, ethics, and information security and privacy within information technology. In the hospital of the future, technology will be the foundation of patient care planning, organization, and delivery (Parker, 2005). Poor resource use is widespread in the U.S. healthcare system, as cited in the Institute of Medicine (IOM) report, “Crossing the Quality Chasm” (IOM, 2001). Many leaders in health care see technology as a means to facilitate decision making, improve efficacy and efficiency, enhance patient safety and quality, and decrease healthcare costs (Ball, Weaver, & Abbot, 2003; IOM, 2000, 2001, 2004). If appropriately implemented and fully integrated, technology has the potential to improve the practice environment for nurses, as well as for patients and their families. However, we are also cautioned by patient safety and quality experts that technology is not a panacea (IOM, 2004). Good decision making for patient care requires good information. Nurses are knowledge workers, who need data and information to provide effective and efficient patient care. Knowledge work is not routine or repetitive but, instead, requires considerable cognitive activity and critical thinking (Drucker, 1993). Data and information must be accurate, reliable, and presented in an actionable form. Technology can facilitate and extend nurses’ decision-making abilities and support nurses in the following areas: (1) storing clinical data, (2) translating clinical data into information, (3) linking clinical data and domain knowledge, and (4) aggregating clinical data (Snyder-Halpern, Corcoran-Perry, & Narayan, 2001). Data about adverse events in hospitalized patients indicate that a majority of physiologic abnormalities are not detected early enough to prevent the event, even when some of the abnormalities are present for hours before the event occurs (Considine & Botti, 2004; Liewelyn, Martin, Shekleton, & Firlet, 1998). Patient surveillance systems are designed to provide early warning of a possible impending adverse event. One example is a system that provides wireless monitoring of heart rate, respiratory rate, and attempts by a patient at risk for falling to get out of bed unassisted; this monitoring is via a mattress coverlet and bedside monitor. Nurses at one hospital decreased the rate of patient falls by 60% with the use of surveillance monitoring (Matsuo et al., 2008). Innovative technology permits physiologic monitoring and patient surveillance by expert clinicians who may be distant from the patient. The remote or virtual intensive care unit (vICU) is staffed by a dedicated team of experienced critical care nurses, physicians, and pharmacists who use state-of-the-art technology to leverage their expertise and knowledge over a large group of patients in multiple intensive care units (Breslow, 2007; Myers & Reed, 2008). Intracranial pressure (ICP) monitoring systems monitor the cranial pressure in critically ill patients with closed head injuries or postoperative craniotomy patients. The ICP, along with the mean arterial blood pressure, can be used to calculate perfusion pressure. This allows assessment and early therapy as changes occur. When the ICP exceeds a set pressure, some systems allow ventricular drainage. Similarly, monitoring pressure within the bladder has recently been demonstrated to accurately detect intra-abdominal hypertension as measures of maximal and mean intra-abdominal pressures and abdominal perfusion pressure are made. Intra-abdominal hypertension occurs with abdominal compartment syndrome and other acute abdominal illnesses and has been demonstrated to be independently associated with mortality in these patients (Malbrain et al., 2005; Vidal et al., 2008). Continuous dysrhythmia monitors and electrocardiograms (ECGs) provide visual representation of electrical activity in the heart and can be used for surveillance and detection of dysrhythmias and for interpretation and diagnosis of the abnormal rhythm. Although not a new technology, these systems have grown increasingly sophisticated. More important, integration with wireless communication technology permits new approaches to triaging alerts to nurses about cardiac rhythm abnormalities. Voice technology and integrated telemetry and nurse paging systems have both been demonstrated to close the communication loop and dramatically decrease response time to dysrhythmia alarms (Bonzheim, 2006). Intravenous (IV) fluid and medication distribution and dispensing via Automated Dispensing Cabinets (ADCs) were introduced in the 1980s and are used in a majority of hospitals today. ADCs can decrease the amount of time before a medication is available on patient care units for administration, ensure greater protection of medications (especially controlled substances), and efficiently and accurately capture drug charges. Most important, ADCs can reduce the risk of medication errors but only when safeguards are available and used. The Institute for Safe Medication Practices (ISMP) has developed guidelines for safest use of ADCs (ISMP, 2008). The guidelines contain 12 core practices associated with safe ADC use and are available on the ISMP website (www.ismp.org/Tools/guidelines/labelFormats/comments/default.asp). Health care is an information-intensive and knowledge-intensive enterprise. Information technology can help healthcare providers acquire, manage, analyze, and disseminate both information and knowledge. Health care in the twenty-first century should be safe, effective, patient-centered, timely, efficient, and equitable (IOM, 2001). Comprehensive data on patients’ conditions, treatments, and outcomes are at the foundation of such care (Stead & Lin, 2009). Humans process data continuously, but in an analog form. Computers process data in a digital form, process data faster and more accurately than humans, and provide a method of storage so that data can be retrieved as needed. The Theory Box above provides key concepts of information processing, and Box 11-1 describes the development of information management skills from novice to expert. Since the mid-1980s, nursing has recognized the importance of demonstrating its distinct contributions to patient care. Clark and Lang (1992, p. 109) stated, “If we cannot name it (nursing), we cannot control it, practice it, research it, teach it, finance it or put it into public policy.” Werley and Lang (1988) convened a work group to define essential data elements to be collected on all patients, defining the Nursing Minimum Data Set (NMDS). Four elements in the NMDS are unique to nursing: nursing diagnosis, nursing intervention, nursing outcome, and intensity of nursing care. Box 11-2 lists the elements of the NMDS. The purposes of the NMDS are the following: 1. To establish the comparability of patient care data across clinical populations, settings, geographic areas, and time 2. To describe the care of patients and families in various settings 3. To provide a means to mark the trends in the care provided and the allocation of nursing resources based on health problems or nursing diagnosis 4. To stimulate nursing research through links to existing data 5. To provide data about nursing care to influence and facilitate healthcare policy decision making Some NMDS elements (e.g., interventions and outcomes) are not collected as easily as the demographic and service elements, which are often captured at patient registration or discharge. This is because we lack uniform or unified structured nursing terminology. Significant efforts have been made to bridge this gap. Thirteen classification systems have been recognized by the American Nurses Association (ANA) (Elfrink, Bakken, Coenen, McNeil, & Bickford, 2001). These recognized classification systems differ. Some contain vocabularies for diagnosis, interventions, and outcomes, whereas others focus on only one or two of these groups. Some terminologies are specialty specific, such as the perioperative nursing data set. During the 1990s, a few nursing terminology leaders began to recognize the importance of nursing terminologies being computerized and connected (interoperable) with one another and with other terminologies in health care. Since 1999, terminology leaders have worked together in a series of nursing terminology summit conferences to develop a united, global, standardized reference terminology for nurses (Ozbolt & Saba, 2008). At the end of the first decade of the twenty-first century, nursing has the data and terminology tools to create patient care records that reflect what nurses have contributed and permit comparison of nursing interventions and patient outcomes. However, many challenges remain. Nurses need education to appreciate the importance and power of standard terminologies compared with locally used terms (Ozbolt & Saba, 2008). • Nursing records must be integrated with other records so that patient information is integrated and can be communicated among the healthcare team. • Clinical nursing experts are needed to work with terminology experts to develop standard language in areas of nursing not yet adequately developed. • Nursing leaders must advocate for use of structured nursing terminologies with the creators and vendors of information systems. Adopting the technology necessary to computerize patient care information systems is complex and must be accomplished in stages. The Health Information and Management Systems Society (HIMSS) has described seven stages of adoption—the seventh of which marks achievement of a fully electronic healthcare record. The seven stages of adoption are listed and described in Table 11-1. It is important to note that only 1% of U.S. hospitals have achieved stage 6 and that fewer than 0.1% have achieved stage 7 (HIMSS Analytics, 2008). TABLE 11-1 ELECTRONIC MEDICAL RECORD ADOPTION MODEL* *From HIMSS Analytics, Health Information Management Systems Society. (2008). EMR Adoption Model. Retrieved from www.himssanalytics.org/hc_providers/emr_adoption.asp. A second chapter in the 2009 accreditation manuals is “The Record of Care, Treatment and Services.” This chapter provides standards and recommendations for the components of a complete medical record. It details documentation requirements that include accuracy, authentication, and thorough, timely documentation. Other standards address the requirements for auditing and retaining records (The Joint Commission [TJC], 2009). Selection of a clinical information system and software partner may be one of the most important decisions of a chief nursing officer and the nursing leadership team (Simpson, 2003). Nurse leaders and direct care nurses must be members of the selection team, participate actively, and have a voice in the selection decision. Remember, nurses are knowledge workers who require data, information, and knowledge to deliver effective patient care. The information system must make sense to the people who use it and fit effectively with the processes for providing patient care. Box 11-3 identifies key elements of an ideal clinical information system that can guide the decision making necessary for selecting or developing health information software. It is imperative to make site visits at organizations already using the software being considered for selection. Discussions at site visits include both the utility and performance of the software and the customer service and responsiveness of the vendor.
Caring, Communicating, and Managing with Technology

Introduction
Types of Technologies
Biomedical Technology
Physiologic Monitoring
Intravenous Fluid and Medication Administration
Information Technology
Structured Terminologies
Information Systems
Information Systems Quality and Accreditation
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nurse Key
Fastest Nurse Insight Engine
Get Clinical Tree app for offline access