52 Care of the substance-using patient
Alcoholic: A person who is excessively dependent on alcohol and who has a noticeable degree of mental, physical, psychologic, or pathologic disorders.
Alcoholic Cirrhosis (Laënnec’s Cirrhosis): A fibrotic form of cirrhosis precipitated by alcohol abuse.
Anterograde Amnesia: The inability to form new memories or recall events that occur after the onset of the amnesia.
Delirium Tremens: An acute and sometimes fatal psychotic reaction caused by cessation of excessive intake of alcoholic beverages over a long period of time.
Endocarditis: Inflammation of the endocardium and heart valves.
Hallucinations: A sensory perception that does not result from an external stimulus and that occurs in the waking state.
Plasma Cholinesterase: An enzyme in the blood plasma that acts as a catalyst in the hydrolysis of acetylcholine to choline and acetate.
Potentiated: A synergistic action in which the effect of two drugs given simultaneously is greater than the sum of the effects of each drug given separately.
Sensorium: The part of the consciousness that includes the special sensory perceptive powers and their central correlation and integration in the brain. A clear sensorium conveys the presence of a reasonably accurate memory together with spacial orientation.
Substance Abuse: The overuse of stimulant, depressant, or other chemicals or drugs that is detrimental to the patient’s physical or mental health.
Substance Dependence: The total psychophysical state of one addicted to drugs or alcohol who must receive an increasing amount of the substance to prevent the onset of withdrawal symptoms.
Substance Use: A maladaptive pattern of the use of a drug, chemical, or biologic entity that is capable of being abused because of its physiologic or psychologic effects.
Substance abuse is the major public health issue in America. More than 25 million Americans have used illicit drugs on a monthly basis, and more than 80% of all the opioids in the world are probably used primarily in the United States.1–5 Add to this the fact that the abuse of prescription drugs has become a major contributing factor to the increase in the use of illicit drugs. Consequently, the significant increase in the number of persons who use opioids, amphetamines, cocaine, hallucinogens, barbiturates, and date rape drugs has created new problems in today’s perianesthesia nursing care. One in five patients in the perioperative area has an alcohol use disorder, one in three patients has a nicotine use disorder, and one in 10 patients has a drug use disorder.6
Drug dependence is the nonmedical use of a drug and consists of the self administration of any drug in a manner that deviates from the approved medical or social practices within a given culture.5 Physical dependence is an altered physiologic state caused by repeated administration of a drug that necessitates the continued administration of the drug to prevent the appearance of withdrawal or abstinence syndromes characteristic for that drug. Psychologic dependence is habituation-compulsive drug use. In this type of dependence, a drug is used to alter mood and feeling. Eventually, dependent people come to believe that the effects of the drug are necessary to maintain an optimal state of well being. Another term that should be defined in discussions of substance dependence is tolerance. Drug tolerance is a state in which, after repeated administration of a drug, a given dose produces a decreased effect or in which increasingly larger doses are needed to obtain the same effect as that of the original dose.
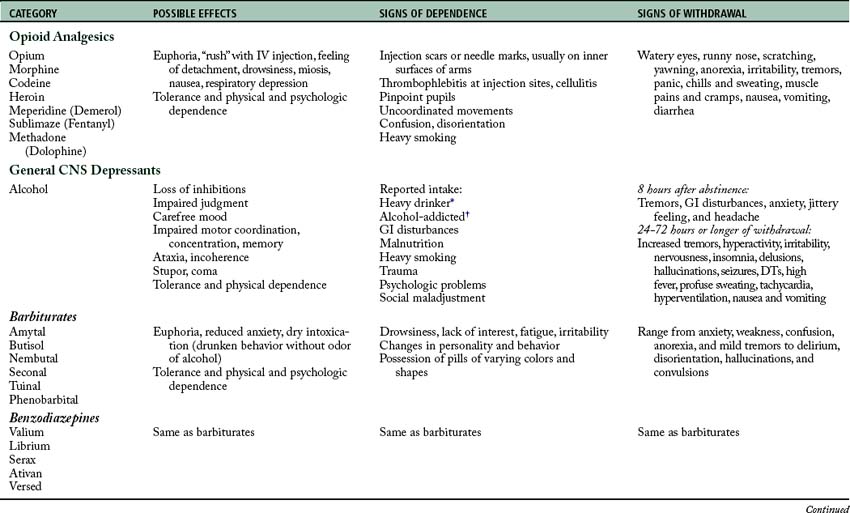
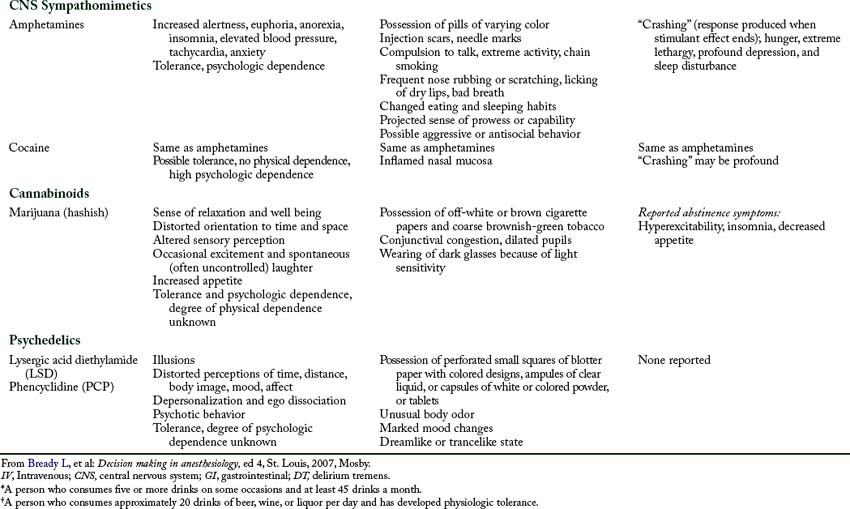
The pharmacologic agents that are most commonly seen in dependence can be grouped as follows: (1) opioid analgesics; (2) general central nervous system (CNS) depressants, such as alcohol and barbiturates; (3) CNS sympathomimetics, such as amphetamines and cocaine; (4) cannabinoids, such as marijuana; and (5) psychedelics (of which lysergic acid diethylamide (LSD) and phencyclidine are the prototypic drugs; Table 52-1), inhalants, club drugs, and date rape drugs.
Opioid analgesics
Opioid analgesics cause strong psychological dependence. Physical dependence is manifested by the withdrawal syndrome of autonomic storm and CNS irritability. A strong tolerance for these drugs and a cross tolerance with other drugs of the same classification of opioid analgesics develop. Studies indicate that in people who are chronically addicted to opioid analgesics such as morphine, the minimum alveolar concentration of inhalation anesthetics (see Chapter 20) is increased, which indicates that a cross tolerance with general inhalation anesthetics may exist.7,8
Perianesthesia nursing care of a patient who is dependent on an opiate, such as heroin dependency, focuses on monitoring the patient for complications.3 Monitoring for the withdrawal (abstinence) syndrome is the foremost concern. The abstinence syndrome after dependence on an opiate occurs in two phases. The acute phase occurs during the first few days. The protracted phase, which is not readily treatable, can persist for as long as 2 to 6 months. The acute opiate abstinence phase is not dangerous to life because it usually is not associated with convulsions and delirium. Instead, the symptoms are anxiety, nervousness, jittery behavior, anorexia, rhinorrhea, hypotension, muscle twitching, insomnia, sweating, pupillary dilation, gooseflesh, nausea, and vomiting. Symptoms during the protracted phase include those of the acute phase, along with convulsions and delirium. Treatment for the acute opiate abstinence phase is accomplished with any opioid analgesic; reports indicate that clonidine has proved to be most effective in attenuating the symptoms. New research indicates that dexmedetomidine may also be effective in attenuating the symptoms. Treatment for the protracted phase focuses on protection of the patient and abatement of the symptoms shown by the patient. If a patient is suspected of dependence on an opiate, opioid antagonists such as naloxone (Narcan) should not be administered because the withdrawal syndrome can be precipitated. No attempt should be made at withdrawal of the patient who is actively dependent on an opiate during the postanesthesia care unit (PACU) period. Liberal use of morphine or methadone in the PACU appears to be satisfactory. Patients who are formerly dependent on opioids should not receive opioids; analgesics such as pentazocine (Talwin) and butorphanol (Stadol) should be used in their place. Nonsteroidal antiinflammatory drugs may also be considered in a multimodal approach for these patients.6
General central nervous system depressants
The dependency rate of persons taking benzodiazepine compounds has increased significantly during the last decade. The benzodiazepine drug is usually taken in combination with marijuana or alcohol to obtain a high. Chronic intoxication has been reported with the use of these compounds. The benzodiazepine that produces the most dependency is diazepam (Valium); however, midazolam (Versed) will soon rank at the same level as diazepam. These drugs are becoming popular because of their rapid onset of action coupled with their pleasure-giving effects. The pharmacologic effects of the benzodiazepines are similar to those of the barbiturates.9 This classification of drugs is somewhat addictive and includes withdrawal syndromes.
For treatment of mild to moderate overdoses of benzodiazepines, the drug physostigmine in an adult dosage of 1 to 2 mg given intravenously can be used. Flumazenil (Romazicon), is a true benzodiazepine receptor antagonist with longer action and fewer side effects. The usual adult dose is 0.1 to 0.2 mg given intravenously. As with naloxone for patient dependence on an opioid, flumazenil must be used with caution with patients who are benzodiazepine dependent. More specifically, reversal of benzodiazepine dependence is associated with precipitating the withdrawal syndrome, including seizures (see Chapter 21).
Alcoholism has long been widespread, but it is difficult to define. An alcoholic, for the purposes of this discussion, is a person who is excessively dependent on alcohol and who has developed a noticeable degree of mental, physical, psychologic, or pathologic disorders. Alcohol was the first anesthetic; it can produce anesthesia, respiratory depression, and hypotension. Alcoholic dependency has been linked to complications during the perianesthesia phase including alcohol withdrawal syndrome, increased infections, acute respiratory distress syndrome, cardiovascular complications, and secondary hemorrhage.6
Alcohol affects many of the body’s major systems.10 Cirrhosis of the liver is common in the later stages of alcoholism. This knowledge is of importance to the perianesthesia nurse because the liver detoxifies many drugs administered during the perioperative period (see Chapter 16). Hepatic cirrhosis can produce significant alterations in pulmonary and cardiovascular functions. Hyperventilation and arterial oxygen desaturation are common findings caused by an increase in shunting of blood away from areas in the lung where diffusion of oxygen occurs. Concomitant with this is an increase in blood volume that can lead to cardiac hypertrophy and eventually to congestive heart failure. Fluid balance is affected by the presence of alcohol, because alcohol exhibits antidiuretic effects by inhibiting the release of antidiuretic hormone. Alcoholic cirrhosis (Laënnec’s cirrhosis) is also associated with portal vein hypertension, renal failure, hypoglycemia, duodenal ulcer, esophageal varices, and hepatic encephalopathy.
In approximately 5% of the alcoholic population, the severe alcohol withdrawal syndrome, or delirium tremens, occurs with abrupt cessation of alcohol ingestion. The mortality rate from this syndrome is approximately 15%; it is considered a medical emergency. The time of onset of delirium tremens is 48 to 72 hours after the abrupt discontinuation of alcohol ingestion.11
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree