51 Care of the pregnant patient
Aortocaval Compression (Scott Syndrome): Obstruction of the inferior vena cava and the pelvic veins by the enlarging uterus.
Aspiration Pneumonitis: An inflammatory condition of the lungs and bronchi caused by material in the stomach regurgitated into the pharynx and inhaled through the epiglottis into the lungs and bronchi.
Cesarean Section: A surgical procedure in which the abdomen and pregnant uterus are incised and the baby is delivered transabdominally.
Cricoid Pressure (Sellick Maneuver): Used in rapid sequence intubation of the trachea in which the cricoid cartilage is pushed against the body of the sixth cervical vertebra in an effort to compress the esophagus to prevent passive regurgitation.
Defasciculation: Administration of a nondepolarizing muscle relaxant 1 to 3 minutes before the administration of succinylcholine to prevent the muscle twitches that usually occur after the administration of a depolarizing muscle relaxant with the intended outcome of reducing the amount of gastric pressure created by the muscle twitches or fasciculations.
Esophagitis: The inflammation of the mucosal lining of the esophagus.
Gastric Motility: The spontaneous peristaltic movements of the stomach that move the stomach contents through the pyloric sphincter into the duodenum.
Gastroesophageal Reflux: Often referred to as heartburn; a result of a backflow of stomach contents as a result of an incompetent lower esophageal sphincter muscle.
Hypovolemia: A reduction from normal in blood volume.
Physiologic Anemia of Pregnancy: A normal reduction in hemoglobin in the blood as a result of the normal physiologic process of pregnancy.
Plasma Cholinesterase: An enzyme in the plasma that is responsible for the metabolic breakdown of acetylcholine to choline and acetate.
Pruritus: The symptom of itching of the skin.
Retained Placenta: After the birth of the infant, the placenta is usually delivered within 30 minutes; if it is expelled after 30 minutes, it is considered to be a retained placenta.
Sepsis: Infection or contamination.
Thromboembolism: A situation in which a blood vessel becomes obstructed by a clot or thrombus that had been carried by the bloodstream from its site of formation.
The incidence rate of surgery performed on pregnant women for reasons unrelated to the pregnancy itself has been reported to be as high as 50,000 to 75,000 cases per year, with a frequency range of 0.75% to 2%.1 The most common conditions that require surgical intervention are acute appendicitis, ovarian cysts, and breast tumors, with laparoscopy being the most common first-trimester procedure. However, more complicated procedures have been reported and include craniotomy, open-heart surgery, and aneurysm repair that have been performed successfully in pregnant patients.1,2
In care of the pregnant patient after surgery, one must remember that two patients require nursing care and assessment: the mother and the fetus. Perianesthesia nursing care should be directed toward emotional support for the mother and avoidance of uterine stimulation that could produce preterm labor. Also of prime importance are prevention of respiratory depression in the mother and maintenance of normal uterine placental blood flow to ensure adequate fetal supply of oxygen and nutrients.1–3
Physiologic changes of pregnancy
Almost every system in the body is affected in some way during pregnancy, either from hormonal changes or from the increasing size of the uterus. The changes that affect perianesthesia nursing care are outlined in Box 51-1 and are discussed in the following sections.
BOX 51-1 Physiologic Changes in Pregnancy
Cardiovascular system
Respiratory system
Cardiovascular changes
Hemodynamic alterations
The cardiovascular system undergoes significant change as pregnancy advances. Cardiac output and heart rate increase progressively during pregnancy until, at 30 to 34 weeks’ gestation, the cardiac output is 30% to 50% higher than normal and the heart rate is approximately 15% greater than the nonpregnant normal level, with electrocardiographic changes and heart sounds possibly developing (Box 51-2). The systolic blood pressure is minimally affected by pregnancy, with a maximum decline of approximately 8% during early to middle gestation and a return to the pregnant level at term. Diastolic blood pressure falls to a greater degree than does systolic pressure, with early to middle gestational decreases of approximately 20%. It also returns to a prepregnancy level at term.4
BOX 51-2 Possible Alterations in Cardiovascular Parameters
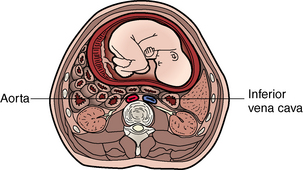
Perhaps the most significant effect on the cardiovascular system for the nurse to consider in routine postanesthesia management is obstruction of the inferior vena cava and the pelvic veins by the enlarging uterus (Figs. 51-1 and 51-2). This condition, known as aortocaval compression or Scott syndrome, can develop by the second trimester and cause supine hypotension. Avoidance of the supine position becomes mandatory after surgery, because it can significantly aggravate the obstruction. Treatment includes the administration of additional intravenous crystalloid, the placement of the mother in the side-lying position, and the administration of supplemental oxygen (Fig. 51-3).5,6
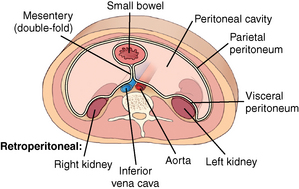
FIG. 51-1 Cross section of lower abdomen (nonpregnant).
(From Bontrager KL, Lampignano JP: Textbook of radiographic positioning and related anatomy, ed 7, St. Louis, 2010, Mosby.)
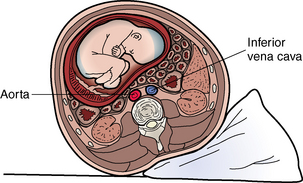
FIG. 51-3 Uterine displacement with wedge under hip to relieve aortocaval compression.
(From Lowdermilk DL, et al: Maternity and women’s health care, ed 10, St. Louis, 2012, Mosby.)
Collateral circulation for venous return develops through the intervertebral venous plexus and the azygos vein. This condition reduces the volume of the epidural and subarachnoid spaces; therefore the amount of drug during regional anesthesia should be decreased. With this in mind, the perianesthesia nurse should assess the patient on admission for a high block and monitor dermatome levels frequently thereafter (see Chapter 25).5,6
In the nonpregnant patient, the sympathetic nervous system plays a role in promoting venous return to the heart from the lower extremities. This sympathetic stimulation of vasomotor tone is enhanced during pregnancy in an effort to counteract the negative effects of uterine compression of the vena cava. Clinically, this protective mechanism is abolished with spinal or epidural anesthesia because it acts as a pharmacologic sympathectomy. Without an appropriate preload of fluids (500 to 1000 mL intravenous lactated Ringer solution), the pregnant patient could have a 30% to 50% decrease in blood pressure during the anesthesia. The pregnant patient must receive an appropriate preload of fluids before epidural or spinal anesthesia. Hemodynamic stability can be secured with the infusion of 15 mL/kg of colloid solution or 30 mL/kg of crystalloid solution. If the patient is to receive an inhalation anesthetic agent such as isoflurane or sevoflurane, similar fluid preloading is given because the inhalation anesthetic agents produce peripheral vasodilation.7
This increased fluid requirement has significant implications for the perianesthesia care of the pregnant patient. Consequently, the patient’s cardiac and hydration status must be monitored closely throughout the emergence phase of regional anesthesia (see Chapter 25).7,8
Hematologic alterations
Blood volume along with the number of platelets, fibrinogen levels, and the level of activity of several clotting factors (VII, VIII, IX, X, and XII) increases by 15% during the first trimester, rises rapidly during the second trimester to 50% above the pregnant levels, and changes little during the remainder of the pregnancy.7,8 However, a smaller rise in the number of circulating red blood cells occurs. This difference results in lower hematocrit and hemoglobin levels (see Box 51-1), although red blood cell mass actually increases. This condition is known as physiologic anemia of pregnancy.7,8
The plasma concentration of the enzyme cholinesterase is decreased during pregnancy. Because plasma cholinesterase is involved in the mechanisms of clotting, the perianesthesia nurse should monitor the pregnant patient for thromboembolism. Plasma cholinesterase is also involved in the destruction of the depolarizing muscle relaxant succinylcholine. The recovery time from succinylcholine is unaltered and in fact may be somewhat faster in pregnant women, which is explained by the fact that the volume distribution of succinylcholine increases during pregnancy because of an elevation in the plasma volume. In the immediate postpartum period, the plasma cholinesterase concentration and the plasma volume distribution are further reduced.7–10
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree