47 Care of the laser/laparoscopic surgical patient
Absorption: The action of the tissue taking up the laser energy, which causes a reaction within the tissue. Thermal damage caused by laser absorption depends on the wavelength and fluence of the laser beam and the tissue consistency, color, and water content.
Coherence: A state in which all the waves travel in the same phase and direction and all the peaks and troughs of the waves are synchronized.
Collimation: A state in which light waves travel parallel to each other and do not diverge or spread, which reduces the loss of power and allows for better focus and precision.
Laparoscopic Surgery: A form of endoscopic surgery with a fiberoptic laparoscope inserted into the peritoneum for surgical assessment or treatment of a wide and continually expanding range of conditions.
Laser (Light Amplification by Stimulated Emission of Radiation): A process by which energy is converted into a light form or light energy.
Monochromatic: Light composed of one color or wavelength.
Pneumoperitoneum: Created when gas is delivered into the abdominal cavity through a Veress needle that is advanced through the abdominal wall. A mechanical insufflator with a pressure-limiting function is connected with tubing to the Veress needle to inflate the peritoneum. When a pneumoperitoneum is achieved, the surgical team is able to visualize the abdomen and perform the indicated procedure.
Reflection: Occurs when the direction of the laser beam is changed after it comes in contact with a surface.
Scattering: Process in which the laser beam is distributed in many different paths after entering the tissue.
Transmission: Occurs when the laser beam passes through or is transmitted through a medium, such as fluids or tissue, with little or no thermal effect.
Laser surgery
The term laser is actually an acronym for light amplification by stimulated emission of radiation. It describes a process by which energy is converted into a light form or light energy. The theory on which laser technology is based was developed by Albert Einstein in 1917. Schawlow and Townes further explored this theory while Gordon Gould also researched light technology. The principle of LASER was introduced in 1958 by these researchers, and the first true laser device was built by Theodore H. Maiman in 1960. Laser devices, although initially controversial, revolutionized surgical procedures; technology and use continue to expand.1,2 The benefits of laser-assisted surgery are many (Box 47-1).2,3
BOX 47-1 Benefits of Laser Surgery
• Seals small blood vessels, possibly reducing intraoperative and postoperative blood loss
• Often decreases postoperative edema and the chance of the spread of malignant cells with sealing effects of lymphatic and vascular vessels
• Sometimes seals nerve endings, thus reducing postoperative pain in certain procedures
• Decreases scarring through the possible reduction of postoperative stenosis and decrease in collagen reformation
• Laser beam precision usually minimizes adjacent tissue damage
• Usually decreases operative and anesthesia time
• Allows for increased use of local anesthetic techniques as opposed to general anesthesia
• More procedures can be done on an ambulatory basis
• Often quickens recovery time and return to activities of daily living
Modified from Houck PM: Comparison of operating room lasers: uses, hazards, guidelines, Nurs Clin North Am 41(2):193-218, 2006; Ball KA: Surgical modalities. In Rothrock JC: Alexander’s care of the patient in surgery, ed 14, St. Louis, 2011, Mosby; Babin-Ebell J: Transmyocardial laser revascularization combined with intramyocardial endothelial progenitor cell transplantation in patients with intractable ischemic heart disease ineligible for conventional revascularization: preliminary results, Thorac Cardiovasc Surg 58(1):11-16, 2010.
Laser light
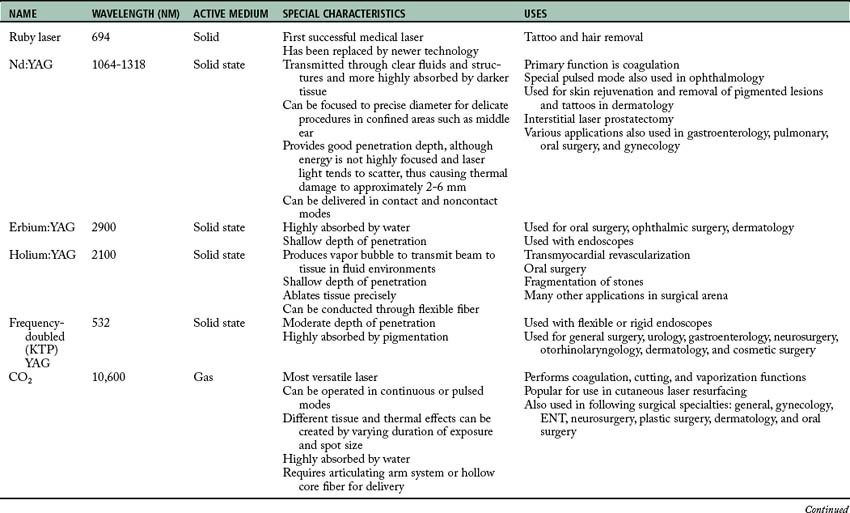
Laser energy is measured by the wavelength of the light, which is the distance between two successive peaks of a wave. Laser wavelengths are often measured in nanometers. One nanometer is equal to 10–9 m.3 Some of the lasers used in surgery today are longer (e.g., the CO2 laser at 10,600 nm or the Nd:YAG laser at 1064 nm) and are within the infrared section of the electromagnetic spectrum. Other laser wavelengths are in the visible area of the electromagnetic spectrum (400 to 750 nm), whereas shorter wavelengths are found in the ultraviolet region of the electromagnetic spectrum (100 to 400 nm; Fig. 47-1).1,3
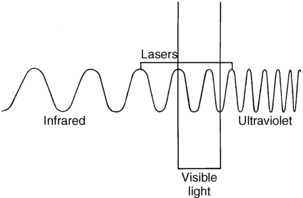
FIG. 47-1 Electromagnetic spectrum.
(From Rothrock JC: Alexander’s care of the patient in surgery, St. Louis, 2011, Mosby.)
Laser light differs from ordinary light in three distinct ways that make it both unique and effective in the surgical setting.1,3
1. Laser light is monochromatic, which means one color or wavelength. This pure color can determine how it reacts with certain tissues. Ordinary light, in comparison, is polychromatic, which means that it comprises a multiple array of colors or wavelengths.
2. Laser light is collimated. The light waves travel parallel to each other and do not diverge or spread. Collimation reduces the loss of power and allows for better focus and precision. Ordinary light spreads out in space as it travels away from its source.
3. Laser light is coherent. All the waves travel in an orderly manner in the same phase and direction, and all the peaks and troughs of the waves are synchronized. This coherence gives the laser beam its power. Ordinary light, in comparison, is incoherent as its waves travel out in random directions.
Tissue interaction
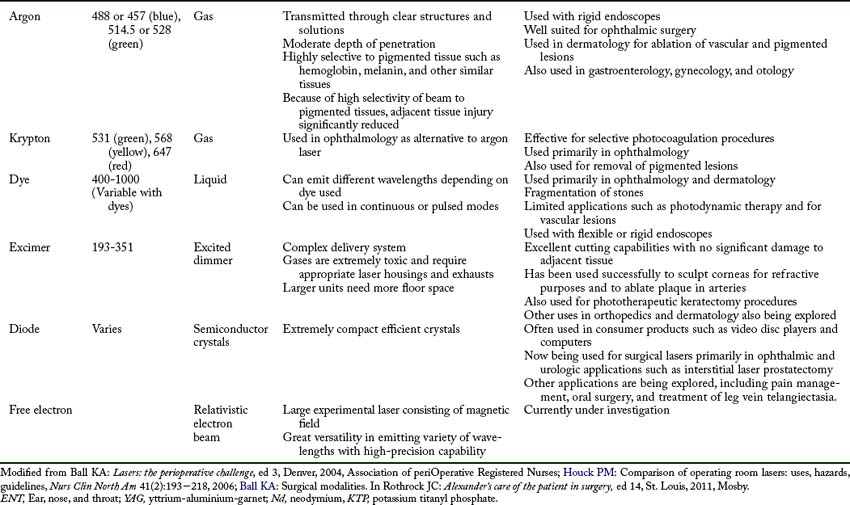
Four different interactions can occur when laser energy comes into contact with human tissue (Fig. 47-2). These interactions include reflection, scattering, transmission, and absorption.3 The extent of this interaction is dependent on the wavelength of the laser, power settings, spot size, duration of exposure of the laser beam with the tissue, and the characteristics of the tissue. These interactions can have both positive and negative effects.1–3
• Reflection. Reflection occurs when the direction of the laser beam is changed after it comes into contact with a surface. This direction change can be intentional or accidental and thus can have both positive and negative effects. Mirrors can be used to intentionally reflect the laser beam to direct the beam to a hard-to-reach area. This action must be done carefully, however, to prevent an inadvertent strike and possible damage to a nontargeted area. Reflection can also occur if the laser beam hits an obstacle (e.g., a surgical instrument) and then is inadvertently reflected to another area, thus causing a tissue burn. Reflection can be either specular (direct reflection) or diffuse (scattered reflection).
• Scattering. The laser beam can also scatter as it enters certain tissues. This scattering causes the beam to disperse over a large area and weakens its strength. Backscattering can also occur as the beam scatters backward up the endoscope, thus causing damage to the operator’s eye, the endoscope optics, or the distal end of the scope.
• Transmission. Transmission occurs when the laser beam passes or is transmitted through fluids or tissue with little or no thermal effect. Transmission depends on the wavelength of the laser beam and the tissue with which it comes in contact. For example, an argon laser beam can be transmitted through the clear structures and solutions of the eye to coagulate a bleeding vessel on the retina. This action occurs because the argon energy is not absorbed by clear structures and solutions; therefore no thermal effect is noted on these tissues.
• Absorption. Thermal effects and tissue response occur only when tissue absorbs the energy of the laser that contacts it. The amount of absorption and penetration depends on the beam’s wavelength and power, the characteristics of the contact tissue (color, consistency, and water content), the duration of the beam exposure, and the beam spot size. A thermal response can occur when tissue absorbs laser energy, thus heating the target cells. The degree of tissue change or thermal damage depends on the temperature to which the cells are heated. This temperature change is purposely regulated to affect the desired tissue response (Table 47-1).
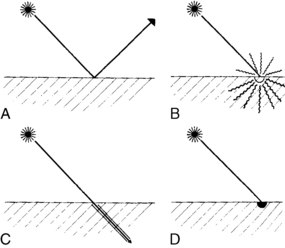
FIG. 47-2 Laser tissue interaction. A, Reflection. B, Scattering. C, Transmission. D, Absorption.
(From Ball KA: Endoscopic surgery, St. Louis, 1997, Mosby.)
Table 47-1 Tissue Changes with Temperature Increases
| TEMPERATURE (°C) | VISUAL CHANGE | BIOLOGIC CHANGE |
|---|---|---|
| 37-60 | No visual change | Warming, welding |
| 60-65 | Blanching | Coagulation |
| 65-90 | White/gray | Protein denaturization |
| 90-100 | Puckering | Drying |
| >100 | Smoke plume | Vaporization, carbonization |
From Ball KA: Lasers: the perioperative challenge, ed 3, Denver, 2004, Association of periOperative Registered Nurses.
Laser surgery can be categorized into three different types of tissue response, including thermal, mechanical, and chemical effects.1 The thermal effect, as discussed previously, is the most common laser effect as tissue is vaporized, coagulated, ablated, cut, and welded depending upon the degree of thermal interaction. The mechanical (acoustical) effect from laser energy results when sound energy is created by the laser beam which disrupts tissue. The chemical effect is produced as the laser energy is used to activate a light-sensitive dye to disrupt and change tissue.
Types of lasers
Lasers are classified by the four active mediums used to generate the laser energy: gas, solid, liquid, and semiconductor crystals. In a gas medium, electric energy is pumped through a gas, such as argon, to produce the laser energy. A solid medium uses a special rod doped with an element that is activated with exposure to flash lamps to create the laser energy. Liquid mediums are organic dyes that produce a wide range of wavelengths when activated with another laser beam. Semiconductor crystals are used in the medical field and in consumer products and fiberoptic communication systems. Experimental mediums that are currently being explored include free electron lasers. The actual laser name is usually derived from the active medium substance that is used to generate the laser energy.1–3 A summary of the various lasers currently in use can be found in Table 47-2.
Preoperative care
For example, transmyocardial revascularization with the laser is generally limited to patients with advanced cardiovascular disease who have hemodynamically stable conditions and are not candidates for traditional bypass surgery. This new laser treatment may offer a method to revascularize the heart muscle for patients with intractable ischemic heart disease.1,4 Dermatologic procedures may require extensive skin preparation at home, preoperative administration of prophylactic antibiotics or antivirals, multiple treatments, and extensive postoperative skin care regimens that may last up to 1 month or more.1,2,5Preoperative care must include education concerning these issues and must be used to determine whether the patient will be able to comply with the treatment regimen.
The patient must also be prepared for expectations both during and after surgery. Many of these procedures are conducted without any anesthesia or with moderate sedation. The patient must be prepared for the sights, smells, and other sensations that will be experienced. Eye protection must be provided. Odors can include the smell of tissue burning or being vaporized. The patient may also have burning or stinging types of painful sensations with certain procedures.1,6
Intraoperative issues
Intraoperative issues with laser procedures primarily concern safety. Lasers are considered a class III medical device and, as such, are subject to U.S. Food and Drug Administration jurisdiction.3 Many other regulatory, industry, and professional bodies also address the safe use of lasers. Regulations addressed include the registration of laser devices, training requirements, laser safety officer responsibilities, and safety rules.1,3
Lasers must be further classified by the manufacturer according to their potential to cause biologic harm and their inherent level of hazard. The classification system is based on the laser output power, wavelength, exposure duration, and emergent beam exposure. The classification system ranges from I to IV; the higher the class, the greater the potential hazard. Most lasers used in surgery are classified as a class IV and can damage eyes and skin and present a fire hazard.1,3 Because of the many provider and patient risks associated with laser use, a laser safety program should be in place in any facility in which laser procedures are conducted. This includes freestanding ambulatory facilities and physician’s offices. A laser safety committee complete with a laser safety officer should be established and responsible for guiding and overseeing all laser use in the facility. Issues that should be addressed include staff education, physician credentialing, and the monitoring of quality and safety issues. All staff involved in laser use must receive appropriate education before using or being involved in laser procedures. Topics included in these special training classes include laser biophysics, laser equipment, laser-tissue interaction, safety procedures, and clinical applications. Knowledge and skills should be verified through a competency-based credentialing program, and the skills should be reassessed and updated on a regular basis.1–3 The three most important areas of safe laser use include eye protection, smoke evacuation, and fire safety.
The eyes are susceptible to damage from laser radiation. The damage may occur acutely or may go unnoticed and develop gradually over time. The type of damage also varies with the type of laser being used. Anyone who enters an operating room or treatment area where a laser is in use (including the patient) is at risk for eye damage and therefore should wear protective eyewear specific to the laser in use. Filtering devices should also be placed on operative microscopes and endoscopes. The patient’s eyes should be protected with either the appropriate eyewear or moist gauze pads.1–3 The protective eyewear should have inscribed on the side of the frame the laser wavelength that the lenses are protecting against along with the optical density (i.e., the lenses’ filtering capabilities).1–3
Another major safety concern with the use of laser technology is the control of the smoke that the laser energy produces as it impacts tissue. This surgical smoke is also called laser plume or surgical plume. Surgical smoke contains extremely small particles of vaporized tissues, toxins, and steam. If inhaled, this particulate can end up in the alveoli of surgical team members or can coat the inside lumen of unprotected suction lines if used for smoke evacuation. Even short exposure to smoke particulate and odor from toxic gases may be related to headaches, nausea, myalgia, rhinitis, conjunctivitis, and respiratory conditions and complications.1–3 In one study, perioperative nurses were shown to have twice the incidence of targeted respiratory problems, probably because of the repeated inhalation of surgical smoke.7–9 In addition, there is a high chance that surgical smoke can transmit viable pathogenic material within the plume.1–3,7
Patients are also exposed to hazards when surgical smoke is not evacuated appropriately. One study demonstrated that laparoscopic surgery patients can absorb the byproducts of laser tissue interaction (surgical smoke), thus increasing the level of the patient’s methemoglobin and carboxyhemoglobin. This in turn, will decrease the oxygen-carrying capabilities of the red blood cells. The patient is absorbing the toxins produced within surgical smoke and then exhibits symptoms of headache, double vision, or nausea in the postanesthesia care area.10 When surgical smoke is properly evacuated during laparoscopy, vision of the surgical site is maintained, smoke is not absorbed by the patient, and these untoward symptoms are not routinely present in the recovering patient.
Implications for practice
For smoke evacuation recommendations to be followed, a comprehensive educational program on smoke hazards along with smoke evacuation equipment training needs to be implemented. Leadership support and active communication among health care providers need to be fostered. Barriers to compliance must be addressed to minimize any obstacles preventing the achievement of a 100% smoke-free surgical environment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree